Total hip and knee arthroplasty are elective surgery procedures commonly undertaken at public hospitals in the United Kingdom, Canada and Australia, where they are associated with long waiting lists and waiting times. In 2008–2009, Australian national median waiting times were 95 days for hip replacement and 114 days for knee replacement.1 Australian elective surgery patients are classified into “urgent”, “semi-urgent” and “non-urgent” categories by their surgeons. There are no standardised criteria to guide classification and there is evidence of substantial inconsistency in the way surgeons assign urgency categories.2 Due to this informal approach to prioritisation, patients are not necessarily treated in order of urgency3 or severity of pain and disability.4 Age, sex, deprivation,5 employment status,6 educational status7 and marital status4 have all been linked with access to elective surgery. This is not an equitable, objective and transparent process for allocating surgery.
A more rational approach would determine priority for surgery with a specified set of clinical and non-clinical indicators to assess the impact of joint disease on the patient. Although Canadian and New Zealand tools have been developed to prioritise patients for joint replacement, these primarily reflect the views of surgeons and researchers.8-11 Little is known about how the general public perceives urgency for surgery, or which criteria should be considered in measuring urgency. Our study compares perceptions of urgency for surgery among a range of orthopaedic and non-orthopaedic assessors. We aimed to determine the relative importance of patient-related factors in the assessment of patients’ urgency for joint replacement.
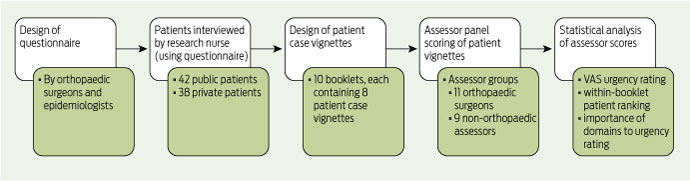
Our study method is outlined in Box 1, following the general method described elsewhere.12
rank the eight patients described in each booklet in order of their perceived urgency for surgery;
assess overall urgency for surgery using a 100 mm visual analogue scale (VAS), where 0 mm represented not urgent and 100 mm represented most urgent; and
assess the level of importance they gave to each domain when determining the urgency rating (scored from 1 to 10, where 1 was not important and 10 was very important).
Eighty patients were recruited to the study. Mean age was 65 years (SD, 12 years), and 54% were women. The major diagnosis was osteoarthritis (79%). Other diagnoses were loose hip prosthesis (5%), avascular necrosis (4%), rheumatoid arthritis (4%) and other miscellaneous conditions (8%). Fifty-five per cent of patients required hip replacement and 45% required knee replacement. Both insured (46%) and uninsured (public) (53%) patients were represented. Using the national clinical urgency category system for elective surgery,13 5% of patients were classified as category 1 (urgent), 91% as category 2 (semi-urgent) and 4% as category 3 (non-urgent).
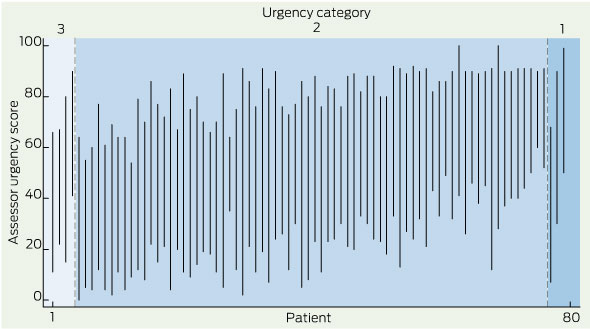
Assessor urgency ratings for each patient, presented in order of the urgency category assigned by their recruiting orthopaedic surgeon, are shown in Box 2. Within each urgency category, the patients are presented in order of mean VAS urgency rating, with each patient’s data presented as a line joining minimum to maximum VAS urgency rating. The results indicate considerable heterogeneity of perceived urgency among the patients in each category and substantial overlap between the perceived urgency of patients across the three categories.
Mean VAS ratings and domain scores for each assessor group are summarised in Box 3. Each assessor group perceived that the pain domain was the most important contribution to their VAS urgency ratings. Both assessor groups also considered the limitations to the mobility domain to be important and the medications and medical comorbidities domains less important. In contrast to the orthopaedic assessors, the non-orthopaedic assessors considered the psychological distress and social circumstances domains to be important (Box 3).
Multivariate analysis (Box 4) demonstrated that the independent correlates of overall urgency varied between assessor groups. Pain and limitations to mobility correlated with urgency for both assessor groups, although the strength of this association varied by assessor group (P for interaction, 0.04 and 0.05 [for interactions of pain and limitations to mobility, respectively, with assessor group]).
The assessors were able to discriminate between different levels of patient urgency using vignettes based on patient interviews. In general, assessors were able to put patients with similar results in order of priority, whether directly ranking patients against each other or using a VAS scale to assign a numerical score. For both assessor groups, pain was the domain most strongly and significantly associated with a patient’s urgency. For orthopaedic surgeons, the limitations to mobility and medical comorbidities domains were also significant predictors of patient urgency, but psychological distress, social circumstances and ADL were considered less important. This is consistent with other evidence indicating that surgeons place less priority on psychological characteristics when prioritising patients for joint replacement.14 We speculate that this is because surgeons find it difficult to assess non-clinical factors and use them to objectively compare the needs of different patients. For the non-orthopaedic assessors in this study, psychological distress, social circumstances and ADL made independent contributions to patient urgency, even after pain and limitations to mobility were taken into account.
In addition to expert orthopaedic surgeons, the study assessors included non-orthopaedic assessors. Until recently, most surgery-related prioritisation studies have only included the views of surgeons and researchers. However, with involvement of the general public in priority setting being increasingly advocated, this is beginning to change. In a recent Spanish study, patients, patients’ relatives, the general public, medical consultants and allied health professionals were involved in identifying priority criteria.15 Also, the Victorian Multi-attribute Prioritisation Tool for joint replacement was developed through a concept-mapping process involving orthopaedic surgeons and patients.16 It is sometimes claimed that members of the public are biased and uninformed; however, all participants bring their own particular biases to priority setting exercises.17 While members of the public may not be experts in the ethical and clinical aspects of health care, they are likely to represent the values of wider society, and incorporation of their views may increase the acceptability of priority setting.18
Received 16 September 2010, accepted 27 July 2011
- Andrea J Curtis1
- Rory Wolfe2
- Colin O H Russell3
- Barry G Elliott4
- John A L Hart5
- John J McNeil6
- Monash University, Melbourne, VIC.
We thank the patients, research nurses, recruiting orthopaedic surgeons, and members of the assessor panel. The study was funded by the Victorian Department of Human Services.
No relevant disclosures.
- 1. Australian Institute of Health and Welfare. Australian hospital statistics 2008–09. Canberra: AIHW, 2010. (AIHW Cat. No. HSE 84; Health Services Series No. 17.)
- 2. Russell C, Roberts M, Williamson TG, et al. Clinical categorisation for elective surgery in Victoria. ANZ J Surg 2003; 73: 839-842.
- 3. Kelly KD, Voaklander DC, Johnston WC, Suarez-Almazor ME. Equity in waiting times for major joint arthroplasty. Can J Surg 2002; 45: 269-276.
- 4. Fitzpatrick R, Norquist JM, Reeves BC, et al. Equity and need when waiting for total hip replacement surgery. J Eval Clin Pract 2004; 10: 3-9.
- 5. Hacker J, Stanistreet D. Equity in waiting times for two surgical specialties: a case study at a hospital in the North West of England. J Public Health (Oxf) 2004; 26: 56-60.
- 6. Clover KA, Dobbins TA, Smyth TJ, et al. Factors associated with waiting time for surgery. Med J Aust 1998; 169: 464-468.
- 7. Siciliani L, Verzulli R. Waiting times and socioeconomic status among elderly Europeans: evidence from SHARE. Health Econ 2009; 18: 1295-1306.
- 8. Western Canada Waiting List Project. From chaos to order: making sense of waiting lists in Canada. Final report. Edmonton: WCWL, 2001. http://www.wcwl.org/media/pdf/library/final_reports.2.pdf (accessed Feb 2011).
- 9. Noseworthy TW, McGurran JJ, Hadorn DC, Waiting for scheduled services in Canada: development of priority-setting scoring systems J Eval Clin Pract 2003; 9: 23-31.
- 10. Arnett G, Hadorn DC. Developing priority criteria for hip and knee replacement: results from the Western Canada Waiting List Project. Can J Surg 2003; 46: 290-296.
- 11. Hadorn DC, Holmes AC. The New Zealand priority criteria project. Part 1: Overview. BMJ 1997; 314: 131-134.
- 12. Curtis AJ, Wolfe R, Russell CO, et al. Prioritizing patients for prostatectomy: balancing clinical and psychosocial factors. ANZ J Surg 2007; 77: 112-117.
- 13. Street A, Duckett S. Are waiting lists inevitable? Health Policy 1996; 36: 1-15.
- 14. Glozier N, Groom G, Prince M. Patient psychological characteristics have minimal influence on surgical prioritization. Psychosom Med 2004; 66: 251-257.
- 15. Sampietro-Colom L, Espallargues M, Rodriguez E, et al. Wide social participation in prioritizing patients on waiting lists for joint replacement: a conjoint analysis. Med Decis Making 2008; 28: 554-566.
- 16. Osborne R, Haynes K, Jones C, et al. Orthopaedic Waiting List Project. Summary report. Melbourne: Victorian Department of Human Services, 2006.
- 17. Bruni RA, Laupacis A, Martin DK, et al. Public engagement in setting priorities in health care. CMAJ 2008; 179: 15-18.
- 18. Allepuz A, Espallargues M, Moharra M, et al. Prioritisation of patients on waiting lists for hip and knee arthroplasties and cataract surgery: instruments validation. BMC Health Serv Res 2008; 8: 76.





Abstract
Objective: To assess which patient characteristics influence the assessments of urgency for surgery by orthopaedic surgeons and non-orthopaedic professionals.
Design, setting and participants: Cross-sectional study of 80 patients requiring elective hip or knee replacement attending a public hospital orthopaedic outpatient clinic or orthopaedic surgeon’s private rooms. Patients were interviewed after being placed on the surgery waiting list. The interview asked about the severity of their joint disease and its effects on physical capability, psychological distress and social circumstances. Patient interviews were summarised and presented to assessors who ranked groups of eight patients in order of their perceived urgency for surgery. Eleven orthopaedic surgeon assessors completed 360 patient ratings and nine non-orthopaedic assessors from various professions, including physiotherapy, social work, research, management and engineering, completed 720 patient ratings.
Main outcome measures: Visual analogue scale rating of patient urgency for surgery; patient rankings for surgery; scores for individual domain contributions to urgency rating.
Results: A broad spread of perceived urgency was evident among the patients. For each group of eight patients, there was moderate agreement on overall urgency rankings between the two groups of assessors. Linear regression demonstrated that pain was the dominant determinant of urgency score for both assessor groups. Orthopaedic surgeons also took into account limitations to mobility and concurrent medical illness but gave less priority to psychological distress or social circumstances. For the non-orthopaedic assessors, limitations to mobility, social circumstances and psychological distress also contributed to urgency.
Conclusion: Both orthopaedic surgeons and non-orthopaedic professionals considered pain the most important factor in establishing urgency and priority for joint replacement. Only the non-orthopaedic professionals considered psychosocial factors important when determining priority for surgery. Broader community discussion about prioritisation for elective surgery is needed to facilitate agreement about which patients factors should be considered.