Rabies poses a threat to over 3.3 billion people worldwide, and causes an estimated 55 000 deaths each year.1 The disease is endemic in Asia, Africa, Europe and the Americas, and is maintained by a wide range of animals. The vast majority of deaths occur in Asia and Africa and, annually, more than 15 million people receive postexposure prophylaxis (PEP) for rabies.1 Australia is free of rabies, but Australian bat lyssavirus causes a rabies-like illness.2
Australians make 6.8 million short-term international departures each year, with over 3 million of these to Asia.3 Many travellers are therefore exposed to the risk of rabies. The emergence of rabies in Bali, Indonesia, since 2008 has resulted in over 100 human deaths,4 and returned travellers from Bali now account for a significant proportion of those seeking rabies PEP in Australia.5
Travellers can be protected from rabies by either vaccination before exposure, or PEP. The World Health Organization (WHO) recommendations for PEP include prompt wound cleaning, administration of rabies immunoglobulin (RIG) into or around the wound, followed by a course of rabies vaccines.1 Ideally, PEP should be commenced as soon as possible after any potential exposure to rabies. Although it is possible for travellers to seek PEP overseas, it can be difficult for them to obtain treatment promptly, and RIG is often unavailable.1 Vaccination against rabies before exposure eliminates the need for RIG, reduces the number of vaccine doses after a potential exposure, and reduces the urgency of starting PEP.
The Australian National Health and Medical Research Council (NHMRC) immunisation guidelines recommend pre-exposure rabies vaccination for:2
“Expatriates and travellers who will be spending prolonged periods (ie, more than a month) in rabies-endemic areas. (NB. This time interval, of more than a month, is arbitrary, and rabies has occurred in travellers following shorter periods of travel)”, and
“People working with mammals in rabies-endemic areas”.
The questionnaire used by doctors at each clinic sought routine information on:
demographic characteristics of the injured traveller;
the geographical location where the injury occurred;
the nature of the injury;
the type of activity the traveller was engaged in when injury occurred, and any initiation of animal contact;
pre-exposure rabies vaccination; and
PEP obtained overseas and on return to Australia.
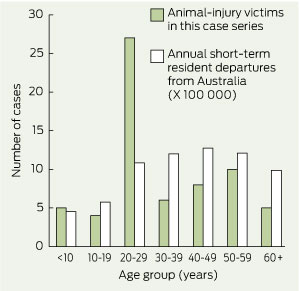
The 65 returned travellers (45 from Queensland and 20 from Perth) who presented for PEP during the 16-month study period included 36 males (55%) and 29 females (45%). The highest number of injuries was seen in travellers aged 20–29 years. Box 1 shows the age distribution of travellers in our study compared with the age distribution of all Australian residents making short-term departures from Australia in 2010.6
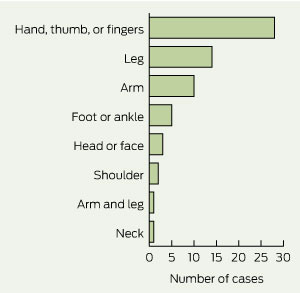
Fifty-one travellers (78%) reported bites, and 11 (17%) reported scratches. The most common body parts injured were the hand (including thumb or fingers), followed by the leg and the arm (Box 2).
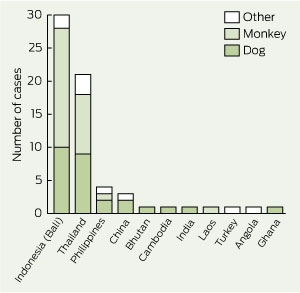
Box 3 shows that the most common destinations where travellers were injured were Bali, Indonesia (30 travellers [46%]), and Thailand (21 [32%]). Currently, 9.6% of Australian short-term resident departures are made to Indonesia, and 6.4% to Thailand.3
Only one traveller had received pre-exposure rabies vaccination. Forty travellers (62%) commenced PEP while overseas, and only nine of these (14%) were able to obtain RIG. Some travellers received RIG after they returned to Australia, and those who presented more than 7 days from their first rabies vaccine dose did not receive RIG (as recommended by the NHMRC).2 Overall, only 35 travellers (54%) completed PEP as recommended by the WHO and received RIG and all doses of the vaccine; 29 travellers (45%) received vaccines only (Box 4).
Our study highlights Indonesia (Bali) and Thailand as particularly high-risk destinations. Considering the recent emergence of rabies in Bali since 2008,7 and the disproportionate number of travellers who were injured while feeding or interacting with monkeys at a monkey temple or monkey forest, we recommend that all travellers to Bali should be warned against these high-risk activities. Travellers aged between 20 and 29 years are at particular risk, and special consideration should be given to this age group when recommending rabies pre-exposure vaccination.
Our findings confirm the difficulties of obtaining adequate PEP and RIG in developing countries.5,8-10 As a result, there were delays in starting PEP, and only half of our travellers were able to comply with WHO recommendations. With the current worldwide shortage of human RIG,1 difficulties of access are likely to continue. Delays in starting or failure to complete timely PEP may result in vaccine failure and the risk of fatal rabies infection.11 Pre-exposure vaccination against rabies will also reduce the cost of PEP to the health care system, but additional evidence would be required to inform a formal cost–benefit analysis.
Rabies vaccination is safe and effective, and provides long-term protection.1 Pre-exposure vaccination using the intradermal route has been proven to be safe and effective for immunocompetent people when performed at a travel medicine clinic with adequately trained nurses, and can be completed at a third of the cost of intramuscular injections.1,12 However, postvaccination serological testing is recommended 2–3 weeks after an intradermal course to confirm immunity,2 and some travellers will not have sufficient time to complete this before departure.
Received 2 December 2010, accepted 30 June 2011
- Deborah J Mills1
- Colleen L Lau2,3
- Philip Weinstein2,4
- 1 Dr Deb — The Travel Doctor, Brisbane, QLD.
- 2 School of Population Health, University of Queensland, Brisbane, QLD.
- 3 Travel Medicine Centre Perth, Perth, WA.
- 4 Barbara Hardy Institute, University of South Australia, Adelaide, SA.
We thank the staff at the Travel Medicine Alliance clinics in Queensland and Western Australia for collecting the data for our study.
No relevant disclosures.
- 1. World Health Organization. Rabies vaccines: WHO position paper. Wkly Epidemiol Rec 2010; 85: 309-320. http://www.who.int/wer/2010/wer8532.pdf (accessed Nov 2011).
- 2. National Health and Medical Research Council. Australian bat lyssavirus infection and rabies. Section 3.1. In: The Australian immunisation handbook [internet]. 9th ed. Canberra: Australian Government Department of Health and Ageing, 2009. http://www.immunise.health. gov.au/internet/immunise/publishing.nsf/Content/Handbook-lyssavirus (accessed Nov 2011).
- 3. Australian Bureau of Statistics. Table 9: Short-term movement, resident departures — selected destinations: original. In: Overseas arrivals and departures, Australia, August 2010. Canberra: ABS, 2010. (ABS Cat. No. 3401.0.) http://www. abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3401.0Aug%202010?OpenDocument (accessed Nov 2011).
- 4. Pro-MED-mail. Rabies, human — Indonesia (18): Bali. 2010; 25 November. (Archive No. 20101125.4254.) http://www.promedmail.org (accessed 20 Nov 2011).
- 5. Gautret P, Lim PL, Shaw M, Leder K. Rabies post-exposure prophylaxis in travellers returning from Bali, Indonesia, November 2008 to March 2010. Clin Microbiol Infect 2011; 17: 445-447.
- 6. Australian Bureau of Statistics. Overseas arrivals and departures, Australia, Dec 2010. Canberra: ABS, 2010. (ABS Cat. No. 3401.0.) http://www. abs.gov.au/AUSSTATS/abs@.nsf/allprimarymain features/5738001A6A1D48F5CA25784900 12A3D7?opendocument (accessed Nov 2011).
- 7. Pro-MED-mail. Rabies, canine, human — Indonesia (21): Bali. 2009; 29 December. (Archive No. 20091229.4373.) http://www. promedmail.org (accessed Nov 2011).
- 8. Wilde H, Briggs DJ, Meslin FX, et al. Rabies update for travel medicine advisors. Clin Infect Dis 2003; 37: 96-100.
- 9. Shaw MT, O’Brien B, Leggat PA. Rabies postexposure management of travelers presenting to travel health clinics in Auckland and Hamilton, New Zealand. J Travel Med 2009; 16: 13-17.
- 10. Gautret P, Shaw M, Gazin P, et al. Rabies postexposure prophylaxis in returned injured travelers from France, Australia, and New Zealand: a retrospective study. J Travel Med 2008; 15: 25-30.
- 11. Wilde H, Sirikawin S, Sabcharoen A, et al. Failure of postexposure treatment of rabies in children. Clin Infect Dis 1996; 22: 228-232.
- 12. Lau C, Sisson J. The effectiveness of intradermal pre-exposure rabies vaccination in an Australian travel medicine clinic. J Travel Med 2002; 9: 285-288.





Abstract
Objectives: To examine the circumstances of animal exposure in a case series of Australian travellers who required rabies postexposure prophylaxis, and to assess the appropriateness of current guidelines for rabies pre-exposure vaccination.
Design, participants and setting: Prospective case series of 65 returned travellers who presented to four Australian travel medicine clinics between 1 April 2009 and 31 July 2010 for rabies post-exposure prophylaxis.
Main outcome measures: Demographic characteristics associated with risk of injury; countries where injuries occurred; circumstances of the injuries; and travellers’ experiences of obtaining postexposure prophylaxis overseas.
Results: Animal bites and scratches occurred most commonly among travellers aged 20–29 years. Most injuries occurred in Bali, Indonesia (30 [46%]) and Thailand (21 [32%]), and the most common animals responsible for the injuries to the 65 travellers were monkeys (29 travellers [45%]) and dogs (27 [42%]). Thirty-nine of the travellers (60%) initiated contact with the animal. Forty travellers (62%) were able to commence rabies vaccination overseas, but only nine (14%) were able to obtain rabies immunoglobulin overseas.
Conclusions: Most travellers had difficulty obtaining rabies postexposure prophylaxis overseas, resulting in significant delays in appropriate treatment. We recommend that current National Health and Medical Research Council guidelines for at-risk persons be broadened, and that the risk of rabies and the option of pre-exposure vaccination be discussed with all travellers to rabies-endemic areas.