Vitamin D3 (cholecalciferol) is a provitamin obtained through exposure of the skin to sunlight and from dietary sources. Vitamin D is essential for calcium homeostasis and bone health, and deficiency has been associated with several chronic diseases.1 Vitamin D requires metabolism in the liver to 25-hydroxyvitamin D (25[OH]D),2 the major circulating form and indicator of vitamin D status.3
There is debate about what serum level of 25(OH)D constitutes deficiency or sufficiency. While deficiency can be regarded as a 25(OH)D level below 50 nmol/L (< 20 ng/mL),4 a recent Institute of Medicine report suggested a level of 50 nmol/L represents adequacy,5 and that further randomised trials are needed before a higher level can be recommended. However, it has elsewhere been suggested that a level of 75 nmol/L (30 ng/mL) should represent sufficiency.6 To maintain a 25(OH)D level of 75 nmol/L, a daily intake or synthesis of at least 1000 IU (25 μg) of vitamin D is required.6
Exposure of skin to ultraviolet B (UVB) radiation in sunlight is the body’s principal vitamin D source.7 UVB penetrates outer layers of skin, causing temporary redness (erythema). UVA radiation penetrates deeper layers of the skin, causing photoageing8 and increased risk of cutaneous malignant melanoma.9 Although UVB is lower early and late in the day, UVA may be relatively high at these times.10 The Ultraviolet Index (UVI) measures ultraviolet radiation (UVR) intensity, and ranges from 1 to about 14 in Australia (higher towards lower latitudes in the north, and decreasing towards higher latitudes in the south).
Melanoma incidence is associated with higher UVI, lower latitude11 and history of sunburn.12 Australian skin cancer prevention campaigns advise sun protection (shade, protective clothing, broad-brimmed hats, sunglasses, sunscreen) during “peak UVI periods”, typically promoted as between 10 am and 3 pm, or when the UVI reaches 3.4,13,14 Conversely, bone health experts recommend short periods of unprotected exposure of the face, arms and hands to sunlight three to six times per week to prevent vitamin D deficiency.15,16 Adherence to protective guidelines without compensatory vitamin D intake increases the risk of deficiency, as clothing,17 shade18 and sunscreen19 reduce vitamin D synthesis. Although evidence is limited, high rates of vitamin D deficiency have been reported in Australians.20,21 Vitamin D deficiency is more prevalent in winter, and insufficiency is common in summer and autumn, suggesting that regular sunlight exposure or intake is required year-round.
The cumulative or standard erythemal dose (SED) of UVR determines the magnitude of vitamin D synthesis. Minimal erythemal dose (MED) is the measure of cumulative UVR exposure that causes erythema, and is equal to about 2 SED. Whole-body exposure to 1 MED is equivalent to an oral dose of about 20 000 IU of vitamin D in fair-skinned individuals.22
Data on hourly UVI and SED between 1 June 1996 and 30 December 2005 were obtained from the Australian Radiation Protection and Nuclear Safety Agency23 for seven cities with data loggers — Darwin (12.4°S), Townsville (19.3°S), Brisbane (27.5°S), Perth (31.9°S), Sydney (34.0°S), Adelaide (34.9°S) and Melbourne (37.7°S). Data from Tasmania were unavailable for the study period. When SED was below 0.005, a value of zero was given. Missing values, indicating data monitor failure, were excluded from calculations.
The Lund–Browder burn diagram24 was used to estimate skin surface exposure percentages (Box 1). The face was not included, as sun protection of the eyes and face is always recommended.14 Estimated body surface areas for children and adolescents did not differ greatly from adults.
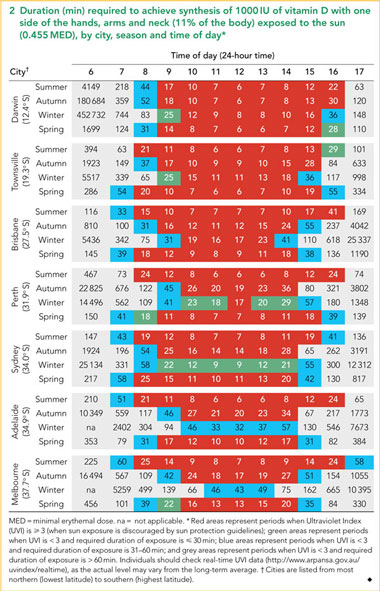
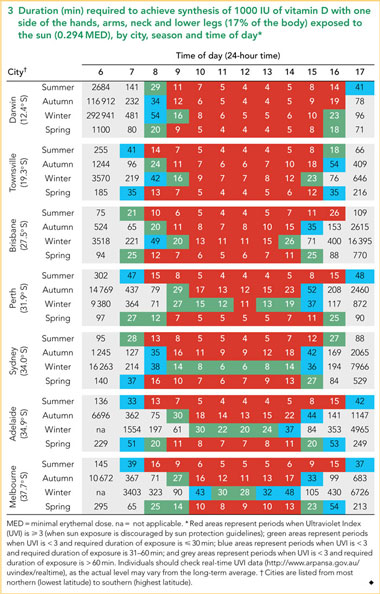
Current guidelines suggest exposure of 15% of the body to one-third of an MED to produce 1000 IU of vitamin D, four to five times a week.13,16 Excluding the face equates to 11% body exposure, which would reportedly produce 733 IU of vitamin D.22 We calculated that when hands, arms and neck on one side of the body (11% of the body) are exposed to the sun, a dose of 0.455 MED is required for fair-skinned individuals to achieve 1000 IU of vitamin D, whereas including one side of the lower legs (17% of the body) decreases the required dose to 0.294 MED (Box 1). We then determined the duration of sun exposure required to achieve each of these MEDs for each hour of daylight between 6 am and 5 pm, by season and city.
Our data showed it was possible for fair-skinned individuals to obtain 1000 IU of vitamin D within 30 min of exposure of 11% (Box 2) or 17% (Box 3) of the skin to the sun, but there were few occasions when this could be achieved at times not excluded by sun protection guidelines. More opportunities to achieve synthesis of 1000 IU in ≤ 30 min occurred, and required duration was shorter, when 17% of the body was exposed to the sun, relative to 11%, as seen by the greater number of green cells in Box 3 relative to Box 2.
UVIav often reached 3 outside the publicised peak UVI period of 10 am–3 pm (Box 2, Box 3). In summer, the UVIav was ≥ 3 between 8 am and 5 pm in all cities except Townsville and Sydney (8 am–4 pm) and Darwin (9 am–5 pm). In winter in Darwin, Townsville, and Brisbane, the UVIav was ≥ 3 from 10 am until 4 pm, 3 pm and 2 pm, respectively. In contrast, in winter in Sydney, Adelaide, and Melbourne, the UVIav remained < 3 throughout the day, allowing exposure without protection during the warmer parts of the day.
UVIav and duration of sun exposure required to achieve 1000 IU of vitamin D synthesis varied according to time of day, season and city (Box 2, Box 3). Opportunities when this could be achieved within 30 min when the UVI was < 3 were limited.
With 11% body exposure, there were no opportunities in summer and autumn to achieve 1000 IU of vitamin D synthesis in ≤ 30 min except Townsville in summer, whereas during winter and spring there were some opportunities in most cities (Box 2).
When lower legs were included in exposure, 1000 IU synthesis could be achieved within 30 min on at least one occasion each day for almost all seasons (with the exceptions of Adelaide, Perth and Melbourne in summer; Townsville in spring; and Darwin and Sydney in autumn) (Box 3). As the UVI was < 3 during the middle part of the day in winter in Perth (except at midday), Sydney, Adelaide and Melbourne, sun exposure of ≤ 30 min during the middle of the day could achieve 1000 IU of vitamin D synthesis.
Overall, when 11% of the body is exposed to the sun, there are few opportunities to synthesise 1000 IU of vitamin D within 30 min at times of the day when sun exposure without protection is not discouraged. In nearly all cities during summer and autumn, there are no opportunities to achieve this, whereas there are more opportunities during winter and spring, particularly in southern cities such as Sydney and Melbourne. For exposure durations of 31–60 min, most cities have at least one opportunity each day to synthesise 1000 IU; however, as these periods mostly occur early and late in the day, we advise caution due to the potentially damaging effects of UVA light at these times.10 It may be preferable to instead increase the amount of skin exposed to the sun to reduce the required duration.
We consider 30 min as the maximum duration that individuals could feasibly spend in the sun each day on a regular basis. Formation of pre-vitamin D plateaus in fair-skinned individuals within 15–45 min of exposure to UVR, after which further exposure causes the breakdown of pre-vitamin D into biologically inactive lumisterol and tachysterol.2
Our findings extend previous guidelines,1,16 which suggest that the majority of fair-skinned individuals in Australia can achieve vitamin D requirements at 10 am or 3 pm, and individuals with no other risk factors for skin cancer can achieve their requirements at 12 noon. However, our findings suggest that UVIav is often ≥ 3 at these times, and the risk of overexposure is therefore higher. We found that UVIav often reached 3 outside commonly promoted peak UVI periods, indicating sun protection behaviour should extend beyond these times.
Our UVI data cover a period of 10 years, and therefore are likely to be robust and based on “typical” cloud cover, although daily variation in cloud cover and pollution levels will alter the required exposure durations. As reported previously,25 we found that the UVIav remains below 3 throughout the day in Sydney, Adelaide and Melbourne during winter, suggesting that there may be a wider safety margin to allow sufficient sunlight exposure to achieve adequate vitamin D synthesis in winter in these cities.
Our recommendations take into account Australian guidelines that suggest sun protection is not required when the UVI is below 3.4 Our suggested doses of 0.455 and 0.294 MED are unlikely to cause sunburn, as 1 MED produces only a faint pinkness in fair-skinned individuals.26 We recommend individuals check real-time UVI data,27 as the actual level may vary from the long-term average.
A limitation of our study is our inability to take into account physiological factors that contribute to vitamin D deficiency, such as increased age,28 increased skin pigmentation,29 fat malabsorption,30 and obesity,31 and as such our recommendations are likely to be an underestimate for individuals affected by these factors.
1 Estimated percentage of skin exposure on one side of the body, and vitamin D synthesis from exposure to 0.294 or 0.455 MED*
MED = minimal erythemal dose. * Extrapolated from Lund–Browder burn diagram24 and Holick.22 |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
Received 2 June 2010, accepted 24 January 2011
- Kellie L Stalgis-Bilinski1
- John Boyages1
- Elizabeth L Salisbury1
- Colin R Dunstan2
- Stuart I Henderson3
- Peter L Talbot4
- 1 Westmead Breast Cancer Institute, University of Sydney, Sydney, NSW.
- 2 Biomedical Engineering, School of Aerospace, Mechanical and Mechatronic Engineering, University of Sydney, Sydney, NSW.
- 3 Non-ionising Radiation Branch, Australian Radiation Protection and Nuclear Safety Agency, Yallambie, VIC.
- 4 Department of Dietetics and Nutrition, Westmead Hospital, Sydney, NSW.
None identified.
- 1. Holick MF. Vitamin D: a D-Lightful health perspective. Nutr Rev 2008; 66 (10 Suppl 2): S182-S194.
- 2. Holick MF. The cutaneous photosynthesis of previtamin D3: a unique photoendocrine system. J Invest Dermatol 1981; 77: 51-58.
- 3. Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press, 1997.
- 4. Risks and benefits of sun exposure: position statement. Approved by the Australian and New Zealand Bone and Mineral Society, Osteoporosis Australia, the Australasian College of Dermatologists and the Cancer Council Australia. 3 May 2007. http://www.cancer.org.au/File/PolicyPublications/PSRisksBenefitsSunExposure03 May07.pdf (accessed Oct 2010).
- 5. Ross AC, Taylor CL, Yaktine AL, Del Valle HB, editors; Committee to Review Dietary Reference Intakes for Vitamin D and Calcium, Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press, 2011.
- 6. Bischoff-Ferrari HA. Optimal serum 25-hydroxyvitamin D levels for multiple health outcomes. Adv Exp Med Biol 2008; 624: 55-71.
- 7. Heaney RP, Davies KM, Chen TC, et al. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 2003; 77: 204-210.
- 8. Sjerobabski Masnec I, Poduje S. Photoaging. Coll Antropol 2008; 32 Suppl 2: 177-180.
- 9. Moan J, Dahlback A, Porojnicu AC. At what time should one go out in the sun? In: Reichrath J, editor. Sunlight, vitamin D and skin cancer. New York: Springer Science+Business Media, 2008: 86-88.
- 10. MacKinley AF, Diffey BL, editors. A reference action spectrum for ultraviolet induced erythema in human skin. CIE Journal 1987; 6: 17-22.
- 11. Eide MJ, Weinstock MA. Association of UV index, latitude, and melanoma incidence in nonwhite populations — US Surveillance, Epidemiology, and End Results (SEER) Program, 1992 to 2001. Arch Dermatol 2005; 141: 477-481.
- 12. Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer 2005; 41: 45-60.
- 13. Working Group of the Australian and New Zealand Bone and Mineral Society, Endocrine Society of Australia and Osteoporosis Australia. Vitamin D and adult bone health in Australia and New Zealand: a position statement. Med J Aust 2005; 182: 281-285. <MJA full text>
- 14. Global Solar UV Index: a practical guide. A joint recommendation of the World Health Organization, World Meteorological Organization, United Nations Environment Programme, and the International Commission on Non-Ionizing Radiation Protection. Geneva: WHO, 2002.
- 15. Nowson CA, Diamond TH, Pasco JA, et al. Vitamin D in Australia. Issues and recommendations. Aust Fam Physician 2004; 33: 133-138.
- 16. Samanek AJ, Croager EJ, Gies P, et al. Estimates of beneficial and harmful sun exposure times during the year for major Australian population centres. Med J Aust 2006; 184: 338-341. <MJA full text>
- 17. Parisi AV, Wilson CA. Pre-vitamin D effective ultraviolet transmission through clothing during simulated wear. Photodermatol Photoimmunol Photomed 2005; 21: 303-310.
- 18. Trouton KJ, Mills CJ. A place in the shade: reducing the risks of UV exposure. CMAJ 1997; 157: 175-178.
- 19. Matsuoka LY, Wortsman J, Hanifan N, Holick MF. Chronic sunscreen use decreases circulating concentrations of 25-hydroxyvitamin D. A preliminary study. Arch Dermatol 1988; 124: 1802-1804.
- 20. van der Mei IA, Ponsonby AL, Engelsen O, et al. The high prevalence of vitamin D insufficiency across Australian populations is only partly explained by season and latitude. Environ Health Perspect 2007; 115: 1132-1139.
- 21. Pasco JA, Henry MJ, Nicholson GC, et al. Vitamin D status of women in the Geelong Osteoporosis Study: association with diet and casual exposure to sunlight. Med J Aust 2001; 175: 401-405.
- 22. Holick MF. Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health. Curr Opin Endocrinol Diabetes 2002; 9: 87-98.
- 23. Australian Radiation Protection and Nuclear Safety Agency. UV-Index Models. http://www.arpansa.gov.au/uvindex/models/ (accessed Jul 2009).
- 24. Royal Children’s Hospital Melbourne. Clinical practice guidelines. Burn diagram. http://www.rch.org.au/clinicalguide/cpg.cfm?doc_id=5250 (accessed Jul 2009).
- 25. Gies P, Roy C, Javorniczky J, et al. Global Solar UV Index: Australian measurements, forecasts and comparison with the UK. Photochem Photobiol 2004; 79: 32-39.
- 26. Holick MF. McCollum Award Lecture, 1994: vitamin D — new horizons for the 21st century. Am J Clin Nutr 1994; 60: 619-630.
- 27. Australian Radiation Protection and Nuclear Saftey Agency. Realtime UV Index data. http://www.arpansa.gov.au/uvindex/realtime/index.cfm (accessed Oct 2010).
- 28. Holick MF, Matsuoka LY, Wortsman J. Age, vitamin D, and solar ultraviolet. Lancet 1989; 2: 1104-1105.
- 29. Matsuoka LY, Wortsman J, Haddad JG, et al. Racial pigmentation and the cutaneous synthesis of vitamin D. Arch Dermatol 1991; 127: 536-538.
- 30. Lo CW, Paris PW, Clemens TL, et al. Vitamin D absorption in healthy subjects and in patients with intestinal malabsorption syndromes. Am J Clin Nutr 1985; 42: 644-649.
- 31. Blum M, Dolnikowski G, Seyoum E, et al. Vitamin D(3) in fat tissue. Endocrine 2008; 33: 90-94.





Abstract
Objective: To examine the feasibility of balancing sunlight exposure to meet vitamin D requirements with sun protection guidelines.
Design and setting: We used standard erythemal dose and Ultraviolet Index (UVI) data for 1 June 1996 to 30 December 2005 for seven Australian cities to estimate duration of sun exposure required for fair-skinned individuals to synthesise 1000 IU (25 μg) of vitamin D, with 11% and 17% body exposure, for each season and hour of the day. Periods were classified according to whether the UVI was < 3 or ≥ 3 (when sun protection measures are recommended), and whether required duration of exposure was ≤ 30 min, 31–60 min, or > 60 min.
Main outcome measure: Duration of sunlight exposure required to achieve 1000 IU of vitamin D synthesis.
Results: Duration of sunlight exposure required to synthesise 1000 IU of vitamin D varied by time of day, season and city. Although peak UVI periods are typically promoted as between 10 am and 3 pm, UVI was often ≥ 3 before 10 am or after 3 pm. When the UVI was < 3, there were few opportunities to synthesise 1000 IU of vitamin D within 30 min, with either 11% or 17% body exposure.
Conclusion: There is a delicate line between balancing the beneficial effects of sunlight exposure while avoiding its damaging effects. Physiological and geographical factors may reduce vitamin D synthesis, and supplementation may be necessary to achieve adequate vitamin D status for individuals at risk of deficiency.