Data from Australian EDs are routinely collected and reported to the National Non-Admitted Patient Emergency Department Care Database (NNAPEDCD). This database currently does not incorporate data on presenting problem or diagnosis.1 A nationally consistent approach to collecting these data for patients attending EDs is becoming increasingly important for the NNAPEDCD, and to support e-health systems designed to improve patient care.
The manner and consistency of data collected on presenting problem and diagnosis within EDs often differ from hospital to hospital and from state to state. Most commonly, the data are collected using a combination of descriptions and codes of the International Classification of Diseases, 10th revision, Australian modification (ICD-10-AM), plus local refinements of this classification and free text. ICD-10-AM is designed for reporting patient morbidity and mortality, with allocation of descriptions and codes at the end of an inpatient episode.2 It is not ideal for recording ED data; the use of free text, and the many and varied terms currently in use across EDs, as well as data fields being left blank, are all evidence of this.
As an example in one state, a Queensland Health technical report showed that ED data for 1.1% (11 709) of total ED presentations for 2007–08 were missing an ICD code in the appropriate field; the most common code recorded — for 7.3% of presentations — was “Z53 – Procedures not carried out”.3 While this may reflect workflow processes, it also reflects the inappropriateness of the use of ICD coding in this context.
Appropriate and clear communications are a major contributor to patient safety within health care environments,4 and this includes information captured for future use in electronic systems. With the advent of electronic health records, the recording of clinical data within EDs is becoming increasingly important, with patient information from the ED visit being included in hospital admission notes and discharge summaries. Current ED data collections focus more on performance data rather than providing efficient and consistent information on the condition diagnosed and the treatment phase of the patient. With about three out of five presentations to Australian EDs leading to a hospital admission,5 recording information on diagnosis is vital in determining and communicating the treatment pathway for a patient through the ED and beyond, in both primary and secondary health care settings.
Diagnostic classifications such as ICD-10-AM typically do not offer the detail required to adequately record patient data for meaningful use in an actual situation at the point of care. In contrast, the Systematized Nomenclature of Medicine – Clinical Terms (SNOMED CT) is a large and comprehensive clinical terminology that enables consistent documentation, exchange and aggregation of data on clinical encounters, and facilitates representing clinically relevant information in electronic health records.6 SNOMED CT has a hierarchical structure made up of concepts and descriptions for these concepts as well as the relationships between them.
As a standard, SNOMED CT complies with Cimino’s seminal desiderata for 21st century medical terminology,7,8 and has been recognised as the most comprehensive clinical terminology available.9 It has been adopted as the principal clinical terminology supporting 15 of the world’s leading national e-health implementation programs.10 The Australian version of SNOMED CT, termed SNOMED CT-AU, which is maintained and distributed by the National E-Health Transition Authority (NEHTA), has one key difference — the identification of content suitable for the Australian health system.
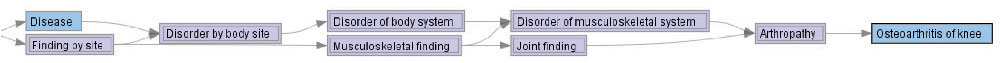
The following example highlights the difference between how a condition such as “Osteoarthritis of knee” is defined using ICD-10-AM and SNOMED CT. In ICD-10-AM, “Osteoarthritis of knee” is represented as “M17.9 – Gonarthrosis, unspecified” in the section “Diseases of the musculoskeletal system and connective tissue” under the heading “Arthropathies”.2 However, in SNOMED CT, this condition is explicitly represented by a series of “IS A” relationships, defining the parent and ancestor concepts, to give greater knowledge of the disorder. Its position within the hierarchy, with parent concept “Arthropathy” and ancestor concepts including “Disorder of musculoskeletal system” and “Joint finding”, is shown in the Box(A). Concepts in SNOMED CT may be fully modelled as shown in the Box(B): in this case, “Osteoarthritis of knee” has an additional relationship “Finding site” with value “Joint structure”. These definitional characteristics of SNOMED CT are what make it more suitable for clinical use and for computer-based systems.
As shown above, SNOMED CT provides a common language, with inbuilt logical definitions. However, it contains a very large number of terms, and EDs do not need access to all of these. Thus, a reference set — a smaller, specialised version of SNOMED CT — is being developed for use within EDs. The reference set uses existing common sets of terms, gleaned from free-text presenting problem and diagnosis fields within ED systems. These terms are then mapped to SNOMED CT. Mapping clinical terms to SNOMED CT is an arduous and time-consuming exercise,6,11 requiring a relatively high level of knowledge of the clinical domain and the structure, content and concept model guidelines of SNOMED CT.
The CSIRO (Commonwealth Scientific and Industrial Research Organisation) Australian e-Health Research Centre has developed Snapper, a software tool to support mapping processes (http://www.aehrc.com.au/snapper/). Snapper provides an easy-to-use platform for mapping existing terms to SNOMED CT to create an ED reference set.
- David P Hansen1
- Madonna L Kemp1
- Sandra R Mills2
- Megan A Mercer2
- Paul A Frosdick2
- Michael J Lawley1
- 1 Australian e-Health Research Centre, CSIRO ICT Centre, Brisbane, QLD.
- 2 National E-Health Transition Authority, Sydney, NSW.
The CSIRO has received licence fees from the International Health Terminology Standards Development Organisation and NEHTA for use of the Snapper software. NEHTA is funded by the Australian Government Department of Health and Ageing.
- 1. Australian Institute of Health and Welfare. National non-admitted patient emergency department care data service. http://www.aihw.gov.au/hospitals/napedc_database.cfm (accessed Feb 2010).
- 2. International classification of diseases and related health problems, 10th revision. Volume 2. Second revision. 2.1 Purpose and applicability. http://www.who.int/classifications/icd/ICD-10_2nd_ed_volume2.pdf (accessed Nov 2010).
- 3. Johnston T, Endo T. Data quality issues impacting on reporting on presentations to emergency departments in Queensland hospitals: data quality issues in emergency department data, 2007–08 update. Technical report — emergency department data report #2. Brisbane: Health Statistics Centre, Queensland Health, 2009.
- 4. Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians. JAMA 2007; 297: 831-841.
- 5. Australian Institute of Health and Welfare. Australian hospital statistics 2007–08. Chapter 5: Non-admitted patient care. Canberra: AIHW, 2009. (AIHW Cat. No. HSE 71; Health Services Series No. 33.) http://www.aihw.gov.au/publications/hse/hse-71-10776/hse-71-10776-c05.pdf (accessed Dec 2009).
- 6. International Health Terminology Standards Development Organisation. SNOMED Clinical Terms (SNOMED CT) International release, January 2009. http://www.cap.org/apps/docs/snomed/documents/january_2009_release.pdf (accessed Dec 2009).
- 7. Cimino JJ, Hripcsak G, Johnson SB, Clayton PD. Designing an introspective, multi-purpose controlled medical vocabulary. In: Kingsland LC, editor. Proceedings of the 13th Annual Symposium on Computer Applications in Medical Care; 1989 Nov 5-8; Washington, DC. Washington, DC: IEEE Computer Society Press, 1989: 513-518.
- 8. Cimino JJ. Desiderata for controlled medical vocabularies in the twenty-first century. Methods Inf Med 1998; 37: 394-403.
- 9. Elkin PL, Brown SH, Husser CH, et al. Evaluation of the content coverage of SNOMED CT: ability of SNOMED clinical terms to represent clinical problem lists. Mayo Clin Proc 2006; 81: 741-748. http://www.mayoclinicproceedings.com/content/81/6/741.full (accessed Sep 2010).
- 10. International Health Terminology Standards Development Organisation. Members of IHTSDO. http://www.ihtsdo.org/members (accessed Sep 2010).
- 11. Rosenbloom ST, Brown SH, Froehling D, et al. Using SNOMED CT to represent two interface terminologies. J Am Med Inform Assoc 2009; 16: 81-88.






Abstract
Emergency departments around Australia use a range of software to capture data on patients’ reason for encounter, presenting problem and diagnosis. The data collected are mainly based on descriptions and codes of the International Classification of Diseases, 10th revision, Australian modification (ICD-10-AM), with each emergency department having a tailored list of terms.
The National E-Health Transition Authority is introducing a standard clinical terminology, the Systematized Nomenclature of Medicine – Clinical Terms (SNOMED CT), as one of the building blocks of an e-health infrastructure in Australia. The Australian e-Health Research Centre has developed a software platform, Snapper, which facilitates mapping of existing clinical terms to the SNOMED CT terminology.
Using the Snapper software, reference sets of terms for emergency departments are being developed, based on the Australian version of SNOMED CT (SNOMED CT-AU). Existing software systems need to be able to implement these reference sets to support standardised recording of data at the point of care.
As the terms collected will be part of a larger terminology, they will be useful for patients’ admission and discharge summaries and for computerised clinical decision making.
Mapping existing sets of clinical terms to a national emergency department SNOMED CT reference set will facilitate consistency between emergency department data collections and improve the usefulness of the data for clinical and analytical purposes.