Clinical records
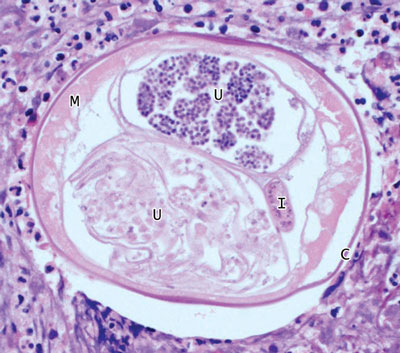
Lymphatic filariasis (LF) is caused by the filarial nematodes Wuchereria bancrofti, Brugia malayi and Brugia timori, which are transmitted between definitive human hosts by multiple mosquito vectors and have varying geographical distributions. LF is common in tropical and subtropical regions — an estimated 120 million people in 81 countries are infected, a third of whom have overt clinical disease.1-2 About one-third of those infected reside in India, a third in Africa, and the remainder in the Americas, South-East Asia and the Pacific, including many of Australia’s neighbours and countries with which Australia shares strong migration links.1 It is difficult to estimate prevalence accurately, but according to antigenic studies, prevalence of LF infection in India (the country with the greatest disease burden) is 5.66%.2 Endemic LF transmission in Australia has not been reported for over 50 years.3All three of the patients described were originally from countries endemic for LF, and their cases highlight the need for clinicians to be aware of the likelihood of LF being imported into Australia. The patients presented with recurrent inguino-scrotal pathology, with or without associated systemic symptoms, emphasising the difficulties of diagnosing this infection.
In non-endemic regions, clinically apparent LF, manifested as adenolymphangitis, hydrocoeles or lymphoedema, is uncommon. Mosquitoes are inefficient vectors for LF — infection is generally restricted to migrants from endemic regions rather than travellers.4
Key clinical features that may assist in making a diagnosis of LF include:
history of residence in an endemic country for several years;
self-limiting nature of attacks, in contrast to bacterial cellulitis, incarcerated hernias or testicular torsion;
bilateral symptoms and signs, as described in Patient 3;
recurrent episodes, as in Patient 2;
palpable regional masses or lymphadenopathy.
Interestingly, many infected people remain asymptomatic. Risk factors for symptomatic disease include duration and intensity of exposure to vectors, adult worm burden, frequency of secondary infections and the host immune response.5
The diagnosis of symptomatic LF requires strong clinical suspicion. Careful ultrasound may identify the random movement of adult worms in dilated lymphatics, known as the “filarial dance sign” (FDS). This is particularly useful in a patient with scrotal symptoms and is considered the gold standard investigation for detecting viable adult worms;6 however, in Patient 3 this did not lead to the diagnosis.
A blood film and serological evaluation are alternative diagnostic options. In most endemic areas, circulating microfilariae (filarial larvae) exhibit nocturnal periodicity (coinciding with peak feeding of local mosquitos) and are best seen on blood films taken between 10 pm and 4 am. If nocturnal samples are not feasible, then provocation with diethylcarbamazine may enhance microfilarial detection 1–2 hours later. Pacific Island infections (except Papua New Guinea) are subperiodic, with maximal microfilaraemia in the late afternoon, and show unresponsiveness to provocation. Importantly, patients with the chronic manifestations of LF often have low levels of circulating microfilariae, resulting in lower blood-film sensitivity.7
Serological tests available in Australia include an in-house enzyme immunoassay (EIA) developed against the dog heartworm Dirofilaria immitis (Westmead Hospital, Sydney, NSW), and an EIA based on IgG4 antibodies to recombinant Bm14 filarial antigen (CELISA, Cellabs, Sydney, NSW).8 Estimates of D. immitis EIA sensitivity and specificity vary and have been limited by an absence of accurate comparators and cross-reactivity. The newer Bm14 test has shown promising sensitivity and specificity. Neither test can differentiate filarial species, or active infection from past infection.
Two tests that may be performed throughout the day are available for filarial antigen detection, which is a measure of adult worm burden (BinaxNOW Filariasis ICT [immunochromatographic test], Alere, Brisbane, QLD; and Og4C3 EIA, TropBio, Townsville, QLD).7 Both tests have limited sensitivity for diagnosing chronic disease manifestations — compared with ultrasound for live adult worms, ICT has 67% sensitivity. Neither test detects antigen from B. malayi or B. timori.6,7,9 BRUGIArapid ICT (Malaysian Biodiagnostics Research, Selangor Bangi, Malaysia) detects antibodies to B. malayi and B. timori only, but must be imported from Malaysia.
In non-endemic areas, the objective of LF treatment is symptom improvement rather than transmission reduction. Traditional LF treatments target microfilariae and have limited activity against macrofilariae. Macrofilariae and the host immune response are responsible for many disease manifestations, but recent evidence has implicated the symbiotic, intracellular bacteria Wolbachia in pathogenesis.5,10,11 Filarial nematodes depend on Wolbachia for normal development and fertility.10 Doxycycline has been shown to clear filaria of Wolbachia symbionts, leading to microfilarial and macrofilarial death, and thus provides an attractive treatment option.11-13
Multiple clinical trials have demonstrated doxycycline’s efficacy in reducing adult worm viability (as measured by scrotal ultrasound), circulating antigenaemia (a marker of adult worm burden) and microfilaraemia.11-13 The degree of reduction of adult worm viability with doxycycline (75%–92%) appears to be far greater than that with any of the commonly used antifilarial agents. Further, doxycycline has significant effects on disease progression, bringing about improvement in lymphatic function, hydrocoele size, lymphoedema, circulating levels of lymphangiogenic factors and rates of lymphangitis.11 The extent to which doxycycline’s effects are mediated through activity against secondary bacterial pathogens has not been evaluated.
The optimal dose and duration for doxycycline therapy is unclear, but studies using 200 mg daily for at least 6 weeks have shown the best results.11,13 Whether doxycycline should be used in conjunction with ivermectin, albendazole or diethylcarbamazine remains unknown. These additional drugs increase adverse events; however, few trials have compared combination regimens to doxycycline alone.12 Overall, the evidence suggests that in non-endemic settings doxycycline is the treatment of choice for symptomatic LF. All patients in this series demonstrated a good clinical response to doxycycline.
Lessons from practice
In non-endemic countries such as Australia, where lymphatic filariasis (LF) is uncommon and can masquerade as other illnesses, the diagnosis may be delayed or missed. A high degree of clinical suspicion should be maintained.
Manifestations of LF include acute adenolymphangitis characterised by acute episodic inguino-scrotal or lower-limb swelling and discomfort, often associated with systemic symptoms and chronic lymphatic dysfunction. Diagnosis is largely based on clinical features, owing to the limitations of diagnostic investigations.
There is growing evidence in support of doxycycline as an effective, well tolerated, affordable disease-modifying treatment that is active against Wolbachia, an essential filarial endosymbiont.
Provenance: Not commissioned; externally peer reviewed.
- 1. Lymphatic filariasis: epidemiology and risk factors (updated 24 Apr 2008). Atlanta: Centers for Disease Control and Prevention. http://www.cdc.gov/ncidod/dpd/parasites/lymphaticfilariasis/epidemiology_lymphatic_filar.htm (accessed Mar 2010).
- 2. Michael E, Bundy DA, Grenfell BT. Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology 1996; 112: 409-428.
- 3. Boreham PFL, Marks NM. Human filariasis in Australia: introduction, investigation and elimination. Proc R Soc Qld 1986; 97: 23-52.
- 4. Hairston NG, de Meillon B. On the inefficiency of transmission of Wuchereria bancrofti from mosquito to the human host. Bull World Health Organ 1968; 38: 935-941.
- 5. Taylor MJ, Hoerauf A, Bockarie M. Lymphatic filariasis and onchocerciasis. Lancet 2010; 376: 1175-1185. Epub 2010 Aug 23.
- 6. Amaral F, Dreyer G, Figueredo-Silva J, et al. Live adult worms detected by ultrasonography in human Bancroftian filariasis. Am J Trop Med Hyg 1994; 50: 753-757.
- 7. Chanteau S, Moulia-Pelat JP, Glaziou P, et al. Og4C3 circulating antigen: a marker of infection and adult worm burden in Wuchereria bancrofti filariasis. J Infect Dis 1994; 170: 247-250.
- 8. Lammie PJ, Weil G, Noordin R, et al. Recombinant antigen-based antibody assays for the diagnosis and surveillance of lymphatic filariasis — a multicenter trial. Filaria J 2004; 3: 9.
- 9. Dreyer G, Lins R, Noroes J, et al. Sensitivity of the immunochromatographic card test relative to detection of adult Wuchereria bancrofti worms by ultrasound. Am J Trop Med Hyg 2008; 78: 28-34.
- 10. Taylor MJ, Bandi C, Hoerauf A. Wolbachia bacterial endosymbionts of filarial nematodes. Adv Parasitol 2005; 60: 245-284.
- 11. Debrah AY, Mand S, Specht S, et al. Doxycycline reduces plasma VEGF-C/sVEGFR-3 and improves pathology in lymphatic filariasis. PLoS Pathog 2006; 2: e92.
- 12. Supali T, Djuardi Y, Pfarr KM, et al. Doxycycline treatment of Brugia malayi-infected persons reduces microfilaremia and adverse reactions after diethylcarbamazine and albendazole treatment. Clin Infect Dis 2008; 46: 1385-1393.
- 13. Taylor MJ, Makunde WH, McGarry HF, et al. Macrofilaricidal activity after doxycycline treatment of Wuchereria bancrofti: a double-blind, randomised placebo-controlled trial. Lancet 2005; 365: 2116-2121.





None identified.