Acutaneous dental sinus tract is a channel which leads from a dental focus of infection to drain onto the face or neck.1 These tracts tend to occur more frequently from infected mandibular teeth (80%) than maxillary teeth (20%).2 Hence, they are more common in the submandibular or submental regions of the face.3 Sinus tracts may result from localised infections, such as an infected tooth, periodontal disease, actinomycosis or osteomyelitis.4 There are numerous reports of cutaneous dental sinus tracts in the dental literature,1,4-10 but comparatively few reports in the medical literature.2,3 Patients with these lesions often present first to general practitioners rather than to dentists,1-7 possibly because they do not associate lesions of the face with teeth and often have no associated dental pain.
Lessons from practice
Dental infection can present with cutaneous lesions of the face and neck.
Dental assessment is recommended for non-healing face and neck lesions, particularly in submandibular and submental regions.
Biopsies or excisions are not necessary and can cause scarring.
Management of the dental focus of infection through endodontic (root canal) treatment or tooth extraction will resolve the sinus tract.
Clinically, a cutaneous dental sinus tract may resemble a pimple, ulcer, nodule, or indurated cystic area. Because these tracts have a similar clinical appearance to other facial lesions and are relatively uncommon, they may be misdiagnosed, leading to inappropriate antibiotic therapy, aspiration or surgery. Unless the dental focus of infection is treated, recurrence is likely.1-10 When surgical intervention is attempted, breakdown of the wound can leave scarring and wound contracture.2-8 In our three patients, the dental sinus tracts occurred because of delays in diagnosis or management.
The differential diagnosis includes pyogenic granuloma, furuncle, foreign body reaction, and cysts, such as sebaceous, epidermoid and thyroglossal cysts.3 Neoplastic causes, such as basal and squamous cell carcinomas, should also be considered,1 as well as other infective causes, including osteomyelitis, actinomycosis and tertiary syphilis gumma.2
When cutaneous sinus tracts are involved, the infected tooth is often free of pain as the tract provides an outlet for inflammatory exudates, allowing decompression.6 The infected, non-vital (ie, necrotic) tooth may be slightly tender to percussion. Histologically, sinus tracts show inflammatory tissue, granulation tissue or abscess formation. The tract may have an epithelial lining.4
Elimination of the source of infection by endodontic treatment or tooth removal results in resolution of the sinus tract, typically within 2 weeks.4,7,8 In most cases, the result is cosmetically acceptable, as in our Patients 1 and 2, but wound contraction and scar tissue may necessitate surgical revision (as in Patient 3).3 Biopsy should be avoided as it may lead to exacerbation of infection or scarring. Antibiotic therapy is indicated when there are signs of systemic involvement (eg, pyrexia or lymphadenopathy).
Clinical records
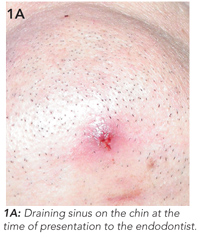
The patient had a history of a car accident which caused trauma to the teeth 15 years previously. He did not receive dental treatment at the time. Clinical examination revealed an erythematous lesion on the chin measuring 0.5 cm in diameter, from which pus drained freely (Figure 1A).
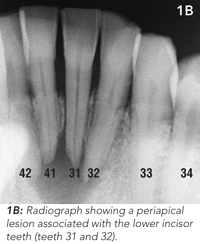
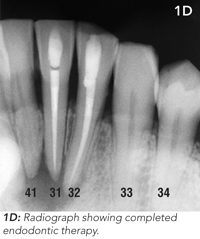
Routine clinical dental tests were conducted, including tooth percussion and CO2 dental pulp testing. Radiographic examination revealed a broad radiolucency associated with three of the lower incisor teeth (Figure 1B). These findings led to a diagnosis of chronic apical periodontitis caused by pulpal necrosis and infection of two lower incisor teeth (teeth 31 and 32). Tooth 41 was vital.
The patient underwent endodontic (root canal) therapy to the lower incisor teeth (31 and 32) and reported that the discharge ceased a week later. Photographs taken at 3-month follow-up showed resolution of the tract (Figure 1C and 1D).

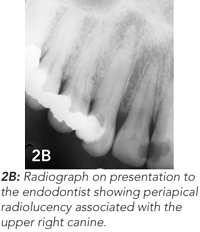
A healthy 41-year-old woman presented to her GP with a non-healing pimple on her right nasolabial fold (Figure 2A). The GP referred the patient to a surgeon who attempted to excise the lesion. Reportedly, the lesion resolved, only to recur 3 months later. By this time, the surgeon suspected a dental aetiology, and referred the patient to an endodontist. Radiographic examination suggested that the lesion was related to an infected upper canine. A radiolucent area around the root of the tooth was characteristic of a periapical abscess (Figure 2B). The tooth was treated endodontically (Figure 2C), and the skin tract resolved.


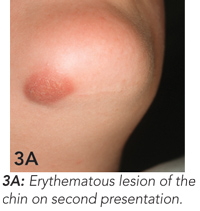
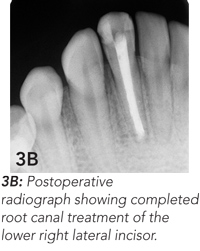
Endodontic treatment was begun, but, because of a dental phobia, the girl delayed completion of this treatment. She presented again 6 months later because the skin lesion had worsened, becoming raised, firm and erythematous (Figure 3A). Endodontic treatment was completed (Figure 3B), and the skin lesion began to heal. At 6-month follow-up, wound contracture had caused dimpling of the skin in the affected area (Figure 3C). This may require surgical revision.

- 1. Tidwell E, Jenkins JD, Ellis CD, et al. Cutaneous odontogenic sinus tract to the chin. Int Endod J 1997; 30: 352-355.
- 2. Cantatore JL, Klein PA, Lieblich LM. Cutaneous dental sinus tract, a common misdiagnosis: a case report and review of the literature. Cutis 2002; 70: 264-265.
- 3. Karp MP, Bernat JE, Cooney DR, Jewett TC. Dental disease masquerading as suppurative lesions of the neck. J Pediatr Surg 1982; 17: 532-536.
- 4. Johnson BR, Remeikis NA, Van Cura JE. Diagnosis and treatment of cutaneous facial sinus tracts of dental origin. JADA 1999; 130: 832-836.
- 5. Cohenca N, Karni S, Rotstein I. Extraoral sinus tract misdiagnosed as an endodontic lesion. J Endod 2003; 29: 841-843.
- 6. McWalter GM, Alexander JB, del Rio CE, et al. Cutaneous sinus tracts of dental aetiology. Oral Surg Oral Med Oral Pathol 1988; 66: 608-614.
- 7. Bender IB, Seltzer S. The oral fistula: its diagnosis and treatment. Oral Surg Oral Med Oral Pathol 1961; 14: 1367-1376.
- 8. Mukerji R, Jones DC. Facial sinus tract of dental origin: a case report. Dent Update 2002; 29: 170-171.
- 9. Sakamoto E, Stratigos GT. Bilateral cutaneous sinus tract of dental etiology: report of a case. J Oral Surg 1973; 31: 701-704.
- 10. Nakamura Y, Hirayama K, Hossain M, Matsumoto K. A case of an odontogenic cutaneous sinus tract. Int Endod J 1999; 32: 328-331.





None identified.