Clinical record
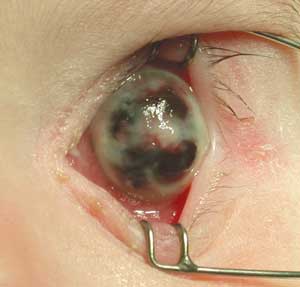
Six hours later, the globe had perforated, with widespread iris prolapse through the now necrotic cornea. Pseudomonas aeruginosa was cultured from the conjunctival specimen taken at the referring hospital. The eye was considered unsalvageable (Box 1), so after discussion with the parents, a decision was made to eviscerate the left eye. After evisceration of the ocular contents, the sclera was closed without an implant, and a conformer was placed in the conjunctival fornix. The eye tissue specimen also grew P. aeruginosa, which was sensitive to gentamicin, tobramycin, timentin, ceftazidime and ciprofloxacin. The child was discharged on the third post-operative day with oral ciprofloxacin 10 mg/kg twice a day and topical tobramycin drops 0.3% four times daily. Three months later, an acrylic ball was inserted into the eye cup to restore orbital volume.
Infectious conjunctivitis is the most common inflammatory eye condition, comprising 0.7% of all presentations to general practitioners in Australia.1 In contrast, infectious keratitis is rare, but is one of the most visually threatening ocular conditions. Infections initially manifesting as conjunctivitis can spread to involve the cornea. Pseudomonas is one pathogen known for this, as appears to have occurred in this patient. The symptoms of conjunctivitis include irritation, stinging and discharge, whereas severe foreign body sensation, pain, photophobia and blurred vision should raise suspicion of keratitis. Signs differentiating conjunctivitis from keratitis are listed in Box 2.
Lessons from practice
Examination is of utmost importance in the paediatric population as less information can be gleaned from the history.
Keratitis can be mistaken for conjunctivitis in its early stages, especially when an adequate view of the globe is not obtained.
Where there is no or limited response to treatment in young infants, the working diagnosis must be reconsidered: a good rule of thumb is if the conjunctivitis does not respond within 72 hours on second-hourly antibiotic drops, either you have the wrong drug or the wrong diagnosis.
Make early referral to an ophthalmologist where there is periorbital cellulitis, or when in doubt.
Risk factors for keratitis in children include trauma, pre-existing corneal disease, prior corneal surgery, contact lens wear and systemic illness.2,3 Endophthalmitis caused by P. aeruginosa has a particularly poor visual prognosis; a case series of 28 patients reported an evisceration or enucleation rate of 64% and a final visual acuity of 5/200 or better achieved in only 7% of patients.4 In a case series of neonates, septicaemia complicated more than half of all cases of Pseudomonas keratitis, and led to death in 40%.5
The differential diagnosis in our 10-week-old patient is similar to the differential diagnosis of ophthalmia neonatorum, which is defined as severe conjunctivitis arising within 1 month after birth.6 These infections, which include Chlamydia trachomatis and Neisseria gonorrhoea, can be acquired at time of delivery, or from the nasopharyngeal passage and from carers.6 Dacryocystitis can also cause marked lid swelling.
- 1. Britt H, Miller GC, Knox S, et al. General practice activity in Australia 2004–05. General Practice Series No. 18. Canberra: AIHW, 2005. (AIHW Cat. No. GEP 18.) http://www.aihw.gov.au/publications/index.cfm/title/10189 (accessed May 2006).
- 2. Cruz OA, Sabir SM, Capo H, Afonso EC. Microbial keratitis in childhood. Ophthalmology 1993; 100: 192-196.
- 3. Vajpayee RB, Ray M, Panda A, et al. Risk factors for pediatric presumed microbial keratitis: a case–control study. Cornea 1999; 18: 565-569.
- 4. Eifrig CWG, Scott IU, Flynn HW Jr, Miller D. Endophthalmitis caused by Pseudomonas aeruginosa. Ophthalmology 2003; 110: 1714-1717.
- 5. Lohrer R, Belohradsky BH. Bacterial endophthalmitis in neonates. Eur J Pediatr 1987; 146: 354-359.
- 6. Krohn MA, Hillier SL, Bell TA, et al. The bacterial etiology of conjunctivitis in early infancy. Am J Epidemiol 1993; 138: 326-332.





None identified.