non-classic presentation of dentofacial pain;
lack of coordinated after-hours dental care;
poor patient education;
patients’ perception of their GP as the primary coordinator of integrated and total care; and
financial considerations: unlike dental consultations, visits to a GP are free where bulk-billing is available.
Glossary
Caries: tooth decay, a condition in which the bone becomes softened, discoloured and porous.
Dentofacial pain: pain arising in the vicinity of the teeth and face.
Occlusal trauma: trauma caused by contact between upper and lower teeth.
Operculum: the flap of gum tissue covering an impacted wisdom tooth.
Dentofacial pain is the reason for a significant proportion of patient presentations to health care professionals. In one study, the US National Institute of Dental and Craniofacial Research reported that an estimated 39 million people (about 22% of the US population aged 18 years or older) had experienced one of five types of orofacial pain more than once during the previous 6 months. Among this cohort, there were 22 million toothaches.1
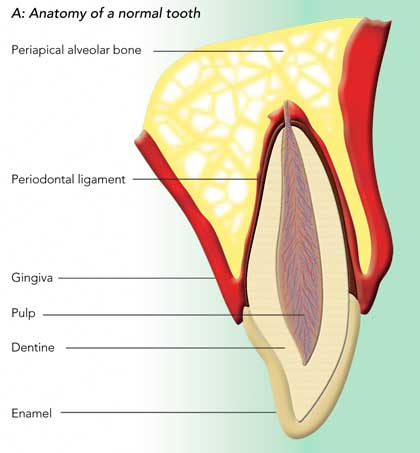
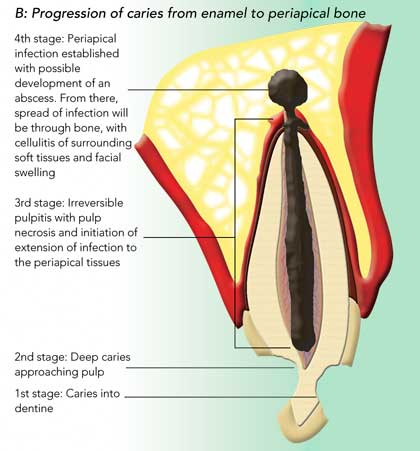
The anatomy of a normal tooth is shown in Box 1, A. Caries extending from enamel into dentine usually causes some sensitivity and pain. The dentine consists of fine tubules that contain cellular processes and afferent nerve fibres surrounded by dentinal fluid. The “hydrodynamic theory” proposes that the fluid moves back and forth to stretch, compress, and excite the nerves in the pulp (the highly vascularised and innervated connective tissue in the central cavity of the tooth). For pain to be felt, the dentine must be excited by a noxious stimulus, either hot or cold, sweet or sour, or touch. The pain is best described as a sensation of sudden shock and is sharp in nature. It is never spontaneous in onset.2
As carious lesions progress, the pulp will eventually become inflamed. It has been postulated that pulpitis leads to increased intrapulp tissue pressure that irritates the sensory nerves of the pulp and causes pain.3 Early in the course of events, this inflammation is reversible and could be thought of as an exaggerated form of dentinal pain. Pain is felt in response to a stimulus (most commonly, cold), and the pain is mild to moderate.4
When the pulp is affected by caries, histological findings are moderate to severe inflammation and some areas of necrosis. Patients present with moderate to severe pain, and 90% report a history of pain before the present pain episode. The pain, in this case, may be triggered by a stimulus (commonly, heat) or arise spontaneously. This stage is identified as irreversible pulpitis, and endodontic treatment or extraction is indicated for the tooth.5
If the inflammatory process or infection is allowed to proceed, the pulp will accumulate more necrotic foci and infection will spread to the apical tissues. The initial pathological response is apical periodontitis (Box 1, B), which is associated with an acute form of periradicular pain that can be excruciating and sometimes lasts for days. The tooth is exquisitely painful to touch, and even contacting the tooth during mouth closure may bring a flood of tears. The pain has been described as constant (24 hours a day), gnawing, throbbing and pounding. Eventually, the patient may gain relief, only to bite on the tooth while eating or sleeping and start the pain cycle once more. Some patients beg to have the tooth extracted, but even if their wish is acceded to, pain may continue for another 48 hours owing to osteitis.4 Spread of infection into periapical tissues forms a localised infection or an abscess (Box 2, Case 1). This can spread to the bony periosteum and cause cellulitis or abscess of soft tissues of the face or neck, with potential life-threatening consequences through possible airway compromise or intracranial spread of infection.
Although caries is the most common cause of pulpitis and periapical spread of infection, there are other conditions that cause dentofacial pain. The most common are occlusal trauma, tooth fractures and cracks. Some infections are iatrogenic. GPs should be aware of caries as a cause of dental pain, but they should also be aware that not all carious lesions appear as cavities in teeth, particularly in this era of water fluoridation (Box 2, Case 2). Sometimes caries will show simply as an area of greyish discolouration or may only be visible on x-ray (Box 3).
Other causes of pain that are often missed by the GP are pericoronitis and alveolar osteitis (dry socket). The typical complaint of the patient with pericoronitis is severe, radiating pain in the back of the mouth and the inability to comfortably open or close the jaw. Not only is it painful to close against the inflamed operculum behind the erupting mandibular molar, but the pain of muscle trismus limits opening of the jaw as well. The soft tissues around the erupting molar are painful to touch, especially during eating (Box 4, Case 3).12
Dry socket, also known as acute alveolar osteitis, is an inflammatory condition of a dental extraction socket, occurring within 2–4 days of a tooth extraction (Box 4, Case 4). It is characterised by a severe, persistent throbbing pain from an extraction socket, which is usually empty but may contain a disintegrated blood clot and/or food debris. The bony walls of the socket are denuded and exquisitely sensitive to even gentle probing. Halitosis is invariably present. The condition probably arises from a complex interaction between surgical trauma, local bacterial infection and various systemic factors.13 Common risk factors are extraction of mandibular (but not maxillary) teeth (particularly lower third molars), poor oral hygiene, and smoking (especially if more than 20 cigarettes are smoked per day).14 Less common reasons for dentofacial pain include trigeminal neuralgia, atypical odontalgia and referred pain from temporomandibular disorders, salivary glands, sinuses and, rarely, the heart. Such unusual pains and presentations require specialist referral.
The main clinical points we have made in this article are summarised in the algorithm in Box 5.
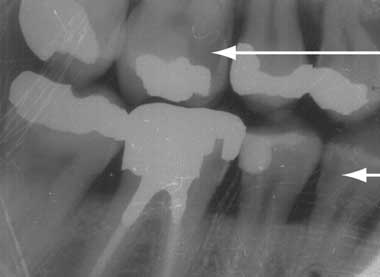
2 Pain arising from dental caries*

Periapical intraoral x-ray of left upper molar: a radiolucent area (arrow), denoting periapical abscess formation, is seen adjacent to one of the roots of the first upper molar, which is heavily restored and has a root canal filling.
Case 1: Progressive facial swelling
Ideal management: Progressive facial swelling secondary to oral infection requires aggressive antibiotic therapy and urgent definitive management of the underlying lesion. Patients should be started on combination amoxycillin + metronidazole or clindamycin6 and referred immediately (if possible) to the nearest tertiary hospital — preferably one with an oral and maxillofacial surgery unit.
Case 2: Diagnosis overlooked because of intact enamel
* These are fictional cases based on typical patient scenarios.
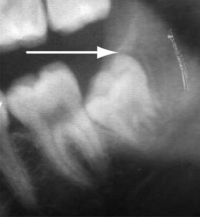
3 Intraoral bitewing x-ray showing crowns of molar and premolar teeth on the right side
Areas of radiolucency (arrows) denote carious lesions. Neither the caries in the upper first molar (beneath an amalgam filling) nor that in the lower first premolar (on the surface adjacent to the next tooth) will be visible clinically.
4 Sources of dentofacial pain other than dental caries*
Case 3: Misdiagnosed pericoronitis
Segment of an orthopantomogram showing an impacted wisdom tooth: a radiolucent area (arrow) is seen behind an impacted right lower wisdom tooth from a patient with pericoronitis.
Ideal management: Pericoronitis should be treated by irrigation of the pericoronal space with a sterile solution such as saline or 0.12% chlorhexidine. Broad spectrum antibiotics should be given if there are systemic symptoms.7,8 The patient should be referred to an oral and maxillofacial surgeon/dentist for surgical extraction of the tooth.
Case 4: Localised pain recurring after an extraction
Ideal management: A patient experiencing pain after tooth extraction should be prescribed an analgesic, preferably a non-steroidal anti-inflammatory drug, and referred back to the operating dentist. The GP should examine the extraction socket for debris and irrigate it with sterile saline or 0.12% chlorhexidine.9-11 The dentist should also give local anaesthetic and/or apply a light packing with an obtundant and a non-irritating antiseptic material.
* These are fictional cases based on typical patient scenarios.
- Mohammed H Mansour1
- Stephen C Cox2
- 1 Oral Surgery, Townsville Hospital, Townsville, QLD.
- 2 Oral Surgery, Westmead Hospital, Sydney, NSW.
None identified.
- 1. Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc 1993; 124: 115-121.
- 2. Trowbridge HO, Franks M, Korostoff E, Emling R. Sensory response to thermal stimulation in human teeth. J Endod 1980; 6: 405-412.
- 3. Kim S. Neurovascular interactions in the dental pulp in health and inflammation. J Endod 1990; 16: 48-53.
- 4. Ingle JI, Click DH. In: Ingle JI, Bakland LK, editors. Endodontics. 5th ed. London: BC Decker Inc, 2002: 259-286.
- 5. Bender IB. Pulpal pain diagnosis — a review. J Endod 2000; 26: 175-179.
- 6. Therapeutic guidelines: antibiotic. 12th ed. Melbourne: Therapeutic Guidelines Limited, 2003: 138.
- 7. Blakey GH, White RP Jr, Offenbacher S, et al. Clinical/biological outcomes of treatment for pericoronitis. J Oral Maxillofac Surg 1996; 54: 1150-1160.
- 8. British Association of Oral and Maxillofacial Surgeons. Validated guidelines in oral and maxillofacial surgery. Management of pericoronitis. Available at: http://www.baoms.org.uk (accessed May 2006).
- 9. Larsen PE. The effect of chlorhexidine rinse on the incidence of alveolar osteitis following the surgical removal of impacted mandibular third molars. J Oral Maxillofac Surg 1991; 49: 932-937.
- 10. Ragno JR Jr, Szkutnik AJ. Evaluation of 0.12% chlorhexidine rinse on the prevention of alveolar osteitis. Oral Surg Oral Med Oral Pathol 1991; 72: 524-526.
- 11. British Association of Oral and Maxillofacial Surgeons. Validated guidelines in oral and maxillofacial surgery. Management and prevention of dry socket. Available at: http://www.baoms.org.uk (accessed May 2006).
- 12. Worrall SF, Riden K, Haskell R, Corrigan AM. UK National Third Molar project: the initial report. Br J Oral Maxillofac Surg 1998; 36: 14-18.
- 13. Vezeau PJ. Dental extraction wound management: medicating post extraction sockets. J Oral Maxillofac Surg 2000; 58: 531-537.
- 14. Garibaldi JA, Greenlaw J, Choi J, Fotovatjah M. Treatment of post-operative pain. J Calif Dent Assoc 1995; 23: 71-72, 74.





Abstract
Dentofacial pain is a common presentation in general practice, and more than 50% of cases arise from dentally related pathology.
In a carious tooth, pain that is site-specific, severe and spontaneous usually denotes extension of caries into the tooth pulp.
Caries does not always appear as a cavity in the tooth, but may lie beneath intact enamel or on surfaces between teeth.
Examination of tooth pain should include firm percussion (eg, with a tongue depressor). Tenderness on percussion denotes progression of infection into the subdental tissue.
Pain occurring 24–48 hours after a tooth extraction is commonly caused by superficial osteitis in the exposed alveolar bone. Examination will reveal the absence of a blood clot in the extraction socket and severe tenderness on local palpation.
Severe pain related to impacted wisdom teeth is frequently caused by pericoronitis, an infection in the gingival tissues surrounding the tooth. The surrounding gingiva is erythematous and tender to palpation.
Localised facial swellings of dental origin require immediate referral to a dentist. Progressive facial swelling requires aggressive antibiotic therapy and referral to hospital for definitive management.