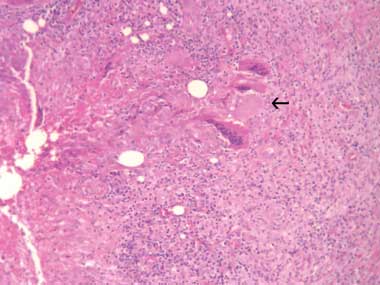
A 31-year-old woman presented with a tender left axillary mass. There was no history of concurrent fevers, sweats or recent illness. She was born in Australia and had not travelled overseas recently. Examination showed a left axillary mass measuring 5 cm in diameter. There was no other lymphadenopathy, no hepatosplenomegaly, nor any breast masses. Aspiration produced 10 mL of purulent fluid. Polymorphs were seen on microscopy but no Mycobacterium spp or other organisms were grown on culture. Histological sections of an excisional biopsy showed nodules of epithelioid histiocytes and giant cells with central necrosis in fibrous stroma, consistent with necrotic granulomatous lymphadenitis (Box, A).
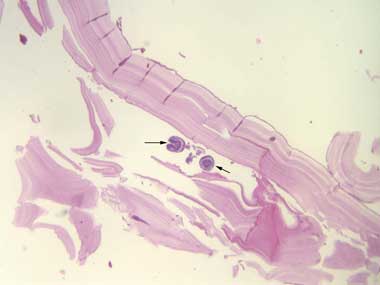
After 6 months of methotrexate treatment the mass recurred. Histological sections from a repeat excisional biopsy revealed the fibrous capsule of a hydatid cyst and multiple scolices. The capsule contained a patchy mixed inflammatory infiltrate and granulomatous reaction with giant cells (Box, B). Hydatid serological testing (by indirect haemagglutination) was positive at a titre of 1 : 640. The presumed exposure was from time spent about 25 years earlier on a farm in rural New South Wales where offal was fed to working dogs.
Three months after commencement of albendazole therapy, the lesion was significantly reduced in size.1
Primary axillary hydatid disease is rare, with only nine previous case reports in the literature.2,3 The causes of granulomatous lymphadenitis can be classified as infective or non-infective, and among these causes, tuberculosis is the most common aetiological agent.4 We believe this to be the first case of axillary hydatid disease presenting as necrotising granulomatous lymphadenitis. Hydatid disease should be considered in the differential diagnosis of granulomatous lymphadenitis.
- 1. World Health Organization. Guidelines for treatment of cystic and alveolar echinococcosis in humans. WHO Informal Working Group on Echinococcosis. Bull World Health Organ 1996; 74: 231-242.
- 2. Losanoff J, Richman B, Jones J. Primary hydatid cyst of the axilla. ANZ J Surg 2004; 74: 393-394.
- 3. Guven G, Simsek H, Cakir B, et al. A hydatid cyst presenting as an axillary mass. Am J Med 2004; 117: 363-364.
- 4. Zumla A, James DG. Granulomatous infections: etiology and classification. Clin Infect Dis 1996; 23: 146-158.





We would like to thank Dr Chris Chow, Department of Histology, Liverpool Hospital, for his assistance in obtaining the histopathological slides for our case.
None identified.