A 30-year-old woman with a history of bipolar disorder presented after ingestion of 4 g of carbamazepine and 40 mg of alprazolam in a suicide attempt. She became increasingly drowsy and eventually required intubation and mechanical ventilation.
The patient received a total of 350 g of activated charcoal via a nasogastric tube over 25 hours. She experienced some charcoal-stained vomiting, but made an otherwise unremarkable recovery and was discharged home.
The patient was hospitalised again 3 days later complaining of constant sharp abdominal pain, diagnosed on culture as a urinary tract infection. Over the next 4 days, she experienced multiple bouts of nausea, charcoal vomits and colicky central abdominal pain.
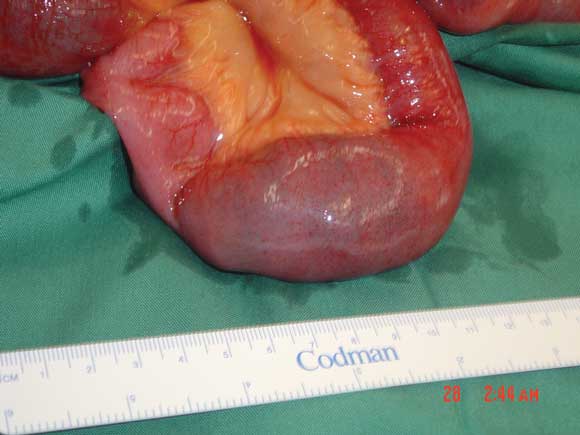
A Gastrografin meal (Schering Pty Ltd, Sydney) and follow-through showed complete small bowel obstruction (Box 1). Subsequent laparotomy revealed a 2.5 × 5 cm bezoar in the distal small bowel, about 60 cm from the ileocaecal valve (Box 2). The bezoar was manually fragmented and passed through the ileocaecal valve into the caecum. The patient recovered well after the operation, and was discharged with psychiatric follow-up.
Charcoal bezoars are a rare complication of activated charcoal administration. They have been associated with treatments for intoxication with carbamazepine,1 amitriptyline,2 theophylline,3 benzodiazepines and barbiturates.4,5 The parasympatholytic effects of the drugs can precipitate or contribute to paralytic ileus, allowing charcoal to accumulate (potentially with remnants of undigested tablets) and form bezoars. Additional factors that influence bowel obstruction secondary to charcoal administration include the dose and timing of activated charcoal therapy, patient age and comorbidities, and previous intra-abdominal surgery.
Gastrointestinal complications should be considered whenever activated charcoal is administered. Prompt recognition and treatment at the first sign of ileus or obstruction may prevent bowel necrosis and subsequent perforation/peritonitis. Charcoal-stained vomiting, abdominal distension and ongoing pain should raise the suspicion of mechanical obstruction. We would advocate Gastrografin follow-through as both a diagnostic and potentially therapeutic tool in incomplete obstruction. However, complete obstruction may signal the need for early laparotomy.
- Justin C Y Chan1
- Chaminda Saranasuriya2
- Bruce P Waxman3
- Department of Surgery, Monash Medical Centre, Dandenong Hospital, Dandenong, VIC.
- 1. Watson WA, Cremer KF, Chapman JA. Gastrointestinal obstruction associated with multiple-dose activated charcoal. J Emerg Med 1986; 4: 401-407.
- 2. Ray MJ, Radin DR, Condie JD, Halls JM. Charcoal bezoar. Small-bowel obstruction secondary to amitriptyline overdose therapy. Dig Dis Sci 1988; 33: 106-107.
- 3. Goulbourne KB, Cisek JE. Small-bowel obstruction secondary to activated charcoal and adhesions. Ann Emerg Med 1994; 24: 108-110.
- 4. Atkinson SW, Young Y, Trotter GA. Treatment with activated charcoal complicated by gastrointestinal obstruction requiring surgery. BMJ 1992; 305: 563.
- 5. Merriman T, Stokes K. Small bowel obstruction secondary to administration of activated charcoal. Aust N Z J Surg 1995; 65: 288-289.