Constipation in childhood can be successfully managed with behavioural modification and prolonged courses of laxatives
Constipation and soiling are common in children. Parental anxiety just before children commence primary school may be the impetus for seeking medical advice. Here, I will focus on the normal acquisition of control of bowel function and the therapeutic approaches for children with constipation. Further information on evidence-based management of constipation in infants and children can be found in a recently published position statement from the North American Society for Pediatric Gastroenterology and Nutrition.1
Meconium is passed within the first 24 hours in about 87% of infants and within 48 hours by 99%;2 this is not influenced by whether the infant is receiving breastmilk or formula.2 Subsequently, however, the method of feeding has a significant impact on stool frequency, colour and consistency. Breast-fed infants pass softer, uniformly yellow stools up to five times a day. This is more frequent than in bottle-fed infants. However, breast-fed infants may occasionally have no bowel actions for 3 days or more, which is rare in bottle-fed infants. Within the first few weeks of life, 64% of breast-fed, but only 30% of bottle-fed, infants are having more than three bowel actions a day.2,3 Stool frequency reduces progressively with age, so that by 16 weeks of age both breast-fed and bottle-fed infants are passing on average two stools a day.4 Weaning, which in most children occurs between 4 and 6 months of age, results in a firmer stool.4
Defecation is a complex process involving a coordinated activity of the abdominal and pelvic musculature (straining) and relaxation of anal sphincters. It is triggered by achieving a threshold distension of the rectum with stool. Once continence has been achieved, defecation can be inhibited by voluntary contraction of the external sphincter. Box 1 summarises the basic principles of toilet training. Boys take slightly longer to toilet train than girls, but complete bowel control is achieved at a mean age of 37 months.5 By pre-school age, 96% of children on a low-fibre diet have a bowel action within the range of three times a day to every alternative day.3,6
Definitions of constipation vary in childhood (as they do in adults), but there is general acceptance that it is abnormal to have a stool frequency of less than three times per week, hard painful defecation, periodic passage of very large amounts of stool at least once every 7–30 days, or a palpable abdominal or rectal mass on physical examination.7 Faecal soiling occurring at least once a week and persisting beyond the age of toilet training can also indicate constipation. Soiling may occur with or without associated faecal retention.
Constipation in childhood is common, with reported prevalence ranging from 0.3% to 28%,8,9 but it is much more frequent when dietary fibre intake is restricted.10 Faecal soiling occurs in 1%–3% of children aged 4–7 years.9 At school age, more boys than girls (ratio, 3 : 1) have constipation.11 This is usually functional (ie, without objective evidence of a pathological condition). About 80% of children with functional constipation will be successfully treated within 5 years.7 Success is less likely when constipation first presents before the age of 12 months, or in children with associated faecal soiling.7
A significant proportion (30%–50%) of children will relapse after being successfully treated for constipation (with or without soiling),7,12 and there is evidence that they do not improve on reaching puberty.7 About 3% of adults report fewer than three bowel movements a week;13 up to 20% of women consider themselves to be constipated; and 10%–20% of men and women regularly use laxatives.13 Faecal incontinence affects up to 8% of adults.14
As in adult practice, the aetiology of constipation and soiling in childhood is multifactorial.15 Painful defecation has been proposed as the primary precipitant of functional faecal retention in early childhood,8,16 although the cause of these painful bowel actions is not clear. Functional faecal retention is characterised by voluntary withholding of stool. Childhood constipation appears to be a significant problem in some Western communities, leading to speculation about the roles of diminished fibre intake and reduced exercise. There is certainly evidence that hard bowel movements may precede stool toileting refusal,5 perhaps leading to a self-perpetuating cycle. Subsequent rectal dilatation is then associated with impaired rectal sensation and motor function.17 Faecal soiling is likely to occur during spontaneous relaxation of the sphincters precipitated by rectal distension.18
In older children, difficulty in evacuating stool may be associated with abnormal contraction of the anal sphincters and pelvic floor during attempted defecation (anismus), which may develop from earlier voluntary withholding behaviour. Slowed colonic transit as a cause of constipation in childhood is also well recognised, as is the association of low fibre intake with hard, infrequent stools. Although extreme restrictions of physical activity and reduced fluid intake can be associated with constipation, these are not usually important factors in most children with constipation.
It has recently been recognised that one of the manifestations of the spectrum of cow’s milk protein allergy in early childhood is constipation.19 Children typically first present in the second or third year. Constipation may be associated with a history of anal fissure, abdominal pain or irritability, although it may also occur in the context of more typical allergic features.20
Finally, anorectal malformations and neurological dysfunction may cause constipation with or without soiling, but are relatively infrequent in paediatric practice compared with functional faecal retention.
Constipation in the first week of life, presenting as delayed passage of meconium beyond the first 48 hours, suggests either an anatomical obstruction, such as anal atresia or stenosis, or Hirschsprung’s disease.
In the next few months, before weaning, bottle-fed infants tend to pass harder stools and may present with difficult passage of hard stools, and occasionally with a fissure. Breast-fed infants are less likely to pass hard stools, but very infrequent stools in these infants may raise parents’ concern about whether this is normal. Constipation may also first present at the time of weaning onto solids — in both breast-fed and bottle-fed infants.
Toilet training for stool may be associated with the development of withholding behaviour and functional faecal retention. Behavioural problems can lead to struggles over toilet training, and the child may start refusing to use the toilet despite being previously successfully trained. Some children are happy to pass urine in a potty but refuse to pass stool at the same time, only passing stool in a nappy. While seated on the potty or toilet, these children may lean back to clench their buttocks and prevent passage of stool. They may also exhibit withholding behaviour when ambulant, crossing their thighs or walking on tiptoe to clench their buttocks.
Up to 63% of children with constipation and faecal soiling will have a history of painful defecation beginning before 3 years of age and secondary withholding behaviour.21 Parents will typically report a child who strains at stool but can not pass more than a small amount.
Apart from the routine aspects of the physical examination, it is important to determine whether the child’s development is within normal limits for his or her age. A brief nutritional assessment is also useful.
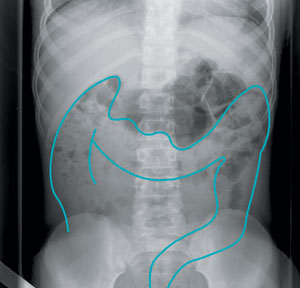
The physical examination should focus particularly on the abdomen, spine and perineum. The abdominal examination reveals whether there is a significant colonic mass. Of all children with significant constipation, about half will have palpable abdominal stool.22
A neurological examination should include the spine as well as lower limbs and the saddle area to assess whether sensation and reflexes are normal.
An anorectal examination enables exclusion of anatomical abnormalities, such as anal stenosis, as well as traumatic injury. It also allows assessment of sphincter tone and the presence of stool. (However, repeated “routine” rectal examinations are likely to add little information and may distress the child.) The presence of firm, packed stool in the rectum correlates closely with radiological evidence of faecal retention,23 with sensitivity and positive predictive values exceeding 90%.23
An abdominal x-ray is only likely to be useful if no significant faecal retention is found on rectal examination.24 There can be considerable interobserver variation among radiologists in scoring x-rays for faecal retention.23 Agreement is more likely with a large amount of retained faeces.
Barium studies are of little or no value in most children with constipation, as they do not add any further information.
Anorectal manometry provides an understanding of the pathophysiological abnormalities underlying the child’s constipation. However, it is only available in a few specialised centres. About 95% of children with functional constipation will have an abnormality on manometric examination (eg, impaired sensation to rectal distension, abnormal contraction of the external anal sphincter and pelvic-floor muscles during straining for defecation, or inability to defecate the rectal balloon — Box 2).22
Measurement of colonic transit by radioisotope or radio-opaque marker is useful to differentiate slow-transit constipation from anismus,25 but is of little practical use in most children with functional constipation.
Blood tests are of limited value, but are useful to confirm that thyroid function and calcium levels are normal. Stool microscopy is of little or no value.
In children between 1 and 4 years of age, a history of allergy, anal fissure or abdominal discomfort20 may suggest allergy to cow’s milk protein, justifying a 2-week trial of restriction of cow’s milk protein.
It is important to spend time at the initial consultation with both child and parents in order to explain that constipation and faecal soiling are common and are likely to improve with age and simple therapies. The easiest way to explain soiling is to emphasise the loss of conscious awareness of the need to defecate that comes with chronic rectal distension with faeces. Episodes of faecal incontinence are likely to be due to involuntary relaxation of the sphincters triggered again by rectal distension. This emphasis on the importance of “keeping the rectum empty” is likely to alleviate blame, and improve cooperation and compliance.26
Children who present with significant faecal retention should have a “clean-out” of the colon.26 Softening agents and stimulant laxatives, taken orally, are usually preferred, although there may be some advantage in the concurrent use of enemas. A regimen for disimpaction is given in Box 4.
Infants who develop constipation before toilet training are best treated with a softener such as lactulose (5–15 mL once daily). Liquid paraffin should be avoided in infants under the age of 6 months, as well as in those with frequent regurgitation, or when there is concern about aspiration. Hypertonic phosphate enema preparations should be avoided in children because of the risk of significant electrolyte disturbance.26
The crucial aspect of long-term maintenance therapy is establishing a regular toileting regimen, generally about two to three times a day for 5–10 minutes at a time after meals, with the child being praised for complying.
It is important to ensure appropriate toileting posture and comfortable foot support with the feet flat.
Behaviour modification can be documented in a toileting diary, which is used to record toileting frequency (usually with a tick), successful passage of stool in the toilet and soiling-free days (with a star), daily medications, and episodes of soiling. Stool reimpaction is less likely to occur if stools are being passed daily.26
Most parents ask about diet, and there is evidence that increasing dietary fibre increases the frequency of bowel actions in children.27 If dietary fibre is deficient, then this should be optimised. There is little evidence to support the use of fibre in excess of recommended intakes in children. Dietary changes are unlikely to be helpful if the main mechanism of constipation is withholding behaviour.
Laxatives are used to help children produce a soft, regular stool, and provide additional benefit compared with behavioural therapy alone.28 They are most useful when children are unable to comply with a regular toileting regimen. A combination of a stool softener (eg, paraffin or lactulose) with a stimulant laxative (eg, Senokot or bisacodyl) is often more successful than either used alone.
Referral of a child for specialist advice should be considered if the symptoms of constipation do not respond to treatment in general practice after 3–6 months; there is frequent soiling and distress; the GP is in doubt about the cause of the symptoms; or the condition is interfering with the child’s schooling or social relationships.30 Significant behavioural abnormalities may merit referral for psychological help, although this is best initiated by a paediatrician. Issues that may need to be addressed include parental distress, low self-esteem in the child, and poor adherence to therapeutic regimens. While referral for psychological assistance may be unnecessary, the psychosocial aspects of every child’s problem should be considered.30
Long-term follow-up studies have established that there is a high relapse rate in children after initially satisfactory therapeutic responses.7 Long-term relapse is more frequent in children under 4 years at onset of symptoms and in whom there is a history of faecal soiling associated with constipation. Maintenance therapy and follow-up should probably be continued for at least 6–24 months. The initial review should be after about 1–2 weeks, then at monthly, and eventually 3-monthly, intervals. It is important to review the toileting diary at each appointment and provide appropriate encouragement. While there is often considerable parental anxiety about the long-term use of laxatives, there is no evidence that secondary colonic inertia is likely to occur in children. A trial of weaning from the use of laxatives should be attempted at 6-monthly intervals.22
Evidence-based practice tips
A combination of behavioural therapy and laxatives is more effective than behavioural therapy used alone (II).28
There is considerable interobserver variation in the interpretation of abdominal x-rays investigating faecal retention (III-2).23
Behavioural modification therapy is effective (III-3).31
Biofeedback therapy, compared with controls, produces no lasting benefit in children with anismus (I).32
Symptoms persist beyond puberty in about 30% of children with constipation and soiling (III-3).7,12
Levels of evidence (I–IV) are derived from the National Health and Medical Research Council’s system for assessing evidence.33
- 1. Baker SS, Liptak GS, Colletti RB, et al. Constipation in infants and children: evaluation and treatment. A medical position statement of the North American Society for Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr 1999; 29: 612-626.
- 2. Griffin A, Beattie RM. Normal bowel habit during the first 6 weeks in healthy, term infants. Ambulatory Child Health 2001; 7: 23-26.
- 3. Tham EB, Nathan R, Davidson GP, Moore DJ. Bowel habits of healthy Australian children aged 0–2 years. J Paediatr Child Health 1996; 32: 504-507.
- 4. Weaver LT, Ewing G, Taylor LC. The bowel habit of milk-fed infants. J Pediatr Gastroenterol Nutr 1988; 7: 568-571.
- 5. Blum NJ, Taubman B, Nemeth N. During toilet training, constipation occurs before stool toileting refusal. Pediatrics 2004; 113: e520-e522.
- 6. Weaver LT, Steiner H. The bowel habit of young children. Arch Dis Childhood 1984; 59: 649-652.
- 7. van Ginkel R, Reitsma JB, Buller HA, et al. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology 2003; 125: 357-363.
- 8. Borowitz SM, Cox DJ, Tam A, et al. Precipitants of constipation during early childhood. J Am Board Family Pract 2003; 16: 213-218.
- 9. Loening-Baucke V. Encopresis and soiling. Pediatr Clin North Am 1996; 43: 279-298.
- 10. Araujo Sant’Anna AM, Calcado AC. Constipation in school-aged children at public schools in Rio de Janeiro, Brazil. J Pediatr Gastroenterol Nutr 1999; 29: 190-193.
- 11. Bellman M. Studies on encopresis. Acta Paediatr Scand 1966; Suppl 170.
- 12. Loening-Baucke V. Constipation in early childhood: patient characteristics, treatment, and longterm follow up. Gut 1993; 34: 1400-1404.
- 13. Walter S, Hallbook O, Gotthard R, et al. A population-based study on bowel habits in a Swedish community: prevalence of faecal incontinence and constipation. Scand J Gastroenterol 2002; 37: 911-916.
- 14. Lynch AC, Dobbs BR, Keating J, Frizelle FA. The prevalence of faecal incontinence and constipation in a general New Zealand population; a postal survey. N Z Med J 2001; 114: 474-477.
- 15. Di Lorenzo C, Benninga MA. Pathophysiology of pediatric fecal incontinence. Gastroenterology 2004; 126 (1 Suppl 1): S33-S40.
- 16. Rasquin-Weber A, Hyman PE, Cucchiara S, et al. Childhood functional gastrointestinal disorders. Gut 1999; 45 Suppl 2: II60-II68.
- 17. Loening-Baucke VA, Cruikshank BM. Abnormal defecation dynamics in chronically constipated children with encopresis. J Pediatr 1986; 108: 562-566.
- 18. Sun WM, Read NW, Miner PB, et al. The role of transient internal sphincter relaxation in faecal incontinence? Int J Colorectal Dis 1990; 5: 31-36.
- 19. Iacono G, Carroccio A, Cavataio F, et al. Chronic constipation as a symptom of cow milk allergy. J Pediatr 1995; 126: 34-39.
- 20. Iacono G. Intolerance of cow’s milk and chronic constipation in children. N Engl J Med 1998; 339: 1100-1104.
- 21. Partin JC, Hamill SK, Fischel JE, Partin JS. Painful defecation and fecal soiling in children. Pediatrics 1992; 89: 1007-1009.
- 22. Loening-Baucke V. Chronic constipation in children. Gastroenterology 1993; 105: 1557-1564.
- 23. Rockney RM, McQuade WH, Days AL. The plain abdominal roentgenogram in the management of encopresis. Arch Pediatr Adolesc Med 1995; 149: 623-627.
- 24. Lewis G, Rudolph CD. Practical approach to defecation disorders in children. Pediatr Ann 1997; 26: 260-268.
- 25. Gutierrez C, Marco A, Nogales A, Tebar R. Total and segmental colonic transit time and anorectal manometry in children with chronic idiopathic constipation. J Pediatr Gastroenterol Nutr 2002; 35: 31-38.
- 26. Felt B, Wise CG, Olson A, et al. Guideline for the management of pediatric idiopathic constipation and soiling. Multidisciplinary team from the University of Michigan Medical Center in Ann Arbor. Arch Pediatr Adolesc Med 1999; 153: 380-385.
- 27. Hillemeier C. An overview of the effects of dietary fiber on gastrointestinal transit. Pediatrics 1995; 96: 997-999.
- 28. Nolan T, Debelle G, Oberklaid F, Coffey C. Randomised trial of laxatives in treatment of childhood encopresis. Lancet 1991; 338: 523-527.
- 29. Nolan T, Catto-Smith T, Coffey C, Wells J. Randomised controlled trial of biofeedback training in persistent encopresis with anismus. Arch Dis Child 1998; 79: 131-135.
- 30. Managing constipation in children. Australian Prescriber 2002; 25: 85-87. Available at: www.australianprescriber.com/index.php?content=/magazines/vol25no4/constipation.htm# (accessed Dec 2004).
- 31. Lowery SP, Srour JW, Whitehead WE, Schuster MM. Habit training as treatment of encopresis secondary to chronic constipation. J Pediatr Gastroenterol Nutr 1985; 4: 397-401.
- 32. Loening-Baucke V. Biofeedback training in children with functional constipation. A critical review. Dig Dis Sci 1996; 41: 65-71.
- 33. National Health and Medical Research Council. How to use the evidence: assessment and application of scientific evidence. Handbook series on preparing clinical practice guidelines. Table 1.3: Designation of levels of evidence. Canberra: NHMRC, February 2000: 8. Available at: www.health.gov.au/nhmrc/publications/pdf/cp69.pdf (accessed Sep 2004).





Abstract
Constipation is common in children, with prevalences ranging from 0.3% up to 28%. In most children, constipation is functional (ie, without objective evidence of a pathological condition). Painful defecation has been proposed as the primary precipitant of functional faecal retention in early childhood.
Faecal soiling is often secondary to constipation, and may occur during spontaneous relaxation of the sphincters precipitated by rectal distension.
Management in general practice combines behavioural modification techniques with prolonged courses of laxatives. Treatment is usually successful, but may take up to 6–12 months.
Significant numbers of children with initially good responses to therapy for constipation relapse in the long term. Long-term relapse is more frequent in children under 4 years at onset of symptoms and in whom there is a history of faecal soiling associated with constipation.