Clinical record
A 35-year-old man presented to the emergency department complaining of right visual blurring and discomfort overnight. Over the previous 2 years, similar episodes had occurred, mostly at night or in dim lighting, affecting one eye at a time and resolving spontaneously each time. The patient was not using any type of medication at the time when the episodes began to occur. Although infrequent initially, these episodes had increased to two or three times a week after mirtazapine, a tetracyclic antidepressant, had been prescribed for depression and anxiety 5 months previously. Symptoms persisted despite treatment being changed to sertraline, a selective serotonin reuptake inhibitor (SSRI). Ten days before presentation, the sertraline was replaced by venlafaxine 75 mg once a day. Symptoms were occurring about every other day. There was no other significant ocular or family history. Spectacle correction revealed compound hypermetropic astigmatism (right eye, +1.00 + 1.50 × 75° left eye, +1.75 + 2.25 × 110°). On presentation, the patient’s visual acuity was 6/24, improving, with a pinhole before the eye, to 6/9 (right eye) and 6/6 (left eye). The right pupil was fixed and mid-dilated and the cornea was mildly oedematous. Both anterior chambers were axially shallow, with forward displacement of the iris–lens diaphragm (ie, the plane formed by the iris and the anterior surface of the lens at the pupil). Intraocular pressures were 69 mmHg (right eye) and 62 mmHg (left eye) (intraocular pressure > 21 mmHg is generally considered as being elevated). Gonioscopy revealed bilateral completely closed angles. The patient was given intravenous mannitol 100 g over 40 minutes, oral acetazolamide 500 mg, topical timolol 0.5%, apraclonidine 1% and pilocarpine 2%. Intraocular pressures fell to 13 mmHg and 5 mmHg in the right and left eyes, respectively. Gonioscopically, the angles could now be opened with indentation of the cornea; however, the anterior chambers remained shallow. Bilateral laser peripheral iridotomies were performed on the day of presentation (left eye) and on the next day (right eye) to eliminate pupil block. Post-iridotomy gonioscopy showed no change in the angle configuration or anterior chamber depth. The patient was sent home with instructions to take oral acetazolamide 250 mg three times a day, topical timolol 0.5% once a day, pilocarpine 2% four times a day, and brimonidine 2% twice a day. Venlafaxine was discontinued. The patient refused alternative antidepressant medication and requested referral to a psychiatrist or psychologist for counselling. On Day 4 after the patient presented with acute angle closure, ultrasound biomicroscopy showed bilateral supraciliary effusions and anterior chamber shallowing (Box 1). Manifest refraction (ie, manual subjective measurement of refractive error) at this time revealed a myopic shift of about 3 dioptres in each eye. Over several weeks, medications to lower intraocular pressure were withdrawn one by one. Follow-up ultrasound biomicroscopy showed gradual resolution of the supraciliary effusion, which was complete some 5 weeks after the acute attack. The anterior chambers deepened slightly and the patient’s usual hypermetropic refraction returned. Gonioscopy at this time still showed easily occludable angles. Bilateral laser peripheral iridoplasties were performed to reduce the risk of future angle closure. |
Venlafaxine is described as a safe and effective antidepressant that is chemically distinct from other antidepressants.1 It is a non-selective inhibitor of the reuptake of serotonin, norepinephrine and dopamine and has no anticholinergic activity in vitro. Because of their relative lack of anticholinergic effects, venlafaxine and similarly acting selective serotonin reuptake inhibitors (SSRIs) are preferred over tri- and tetracyclic antidepressants for patients who are at risk of angle closure. We report the case of a young patient taking venlafaxine who developed simultaneous bilateral acute angle closure secondary to supraciliary effusions.
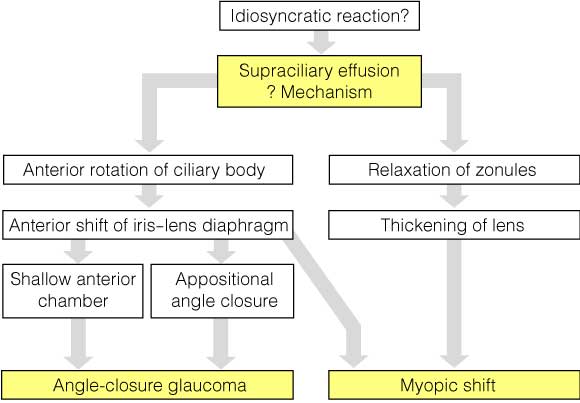
Angle closure and/or acute transient myopia possibly caused by supraciliary effusion has been reported for many drugs, including sulfonamides, tetracycline and some diuretics.2 Supraciliary effusions causing secondary angle closure in patients taking topiramate3-5 and sulfonamides6 have been documented by ultrasound biomicroscopy by various authors. The postulated mechanisms by which supraciliary effusions produce angle-closure glaucoma and transient myopia are illustrated in Box 2.
There have been reports in the literature of angle closure or increased intraocular pressure in patients taking venlafaxine8,9 or SSRIs.5,10-15 We found one previous report of bilateral acute angle-closure glaucoma in a patient taking venlafaxine8 and one report of raised intraocular pressure in two known glaucoma patients with narrow angles taking venlafaxine.9 Eleven cases of raised intraocular pressure in patients taking SSRIs have been reported to the Australian Adverse Drug Reactions Advisory Committee.10 However, the mechanisms for the raised intraocular pressure in these cases are not mentioned.
To our knowledge, ours is the first reported case of acute angle closure in a patient taking venlafaxine in which the presence of a supraciliary effusion precipitating the secondary angle closure has been identified by ultrasonography.
Furthermore, our patient was taking only venlafaxine at the time of presentation. The patient in the abovementioned case of acute angle closure8 had taken four other medications immediately before starting or during treatment with venlafaxine. There is a case report of secondary angle closure due to supraciliary effusions in a patient taking topiramate who was also taking venlafaxine, but the authors attributed the effusions to the topiramate.4 It is possible that the mirtazapine and sertraline taken previously by our patient contributed to his condition, as did his underlying hypermetropic status.
It may be that the weak anticholinergic or mydriatic effects of serotonergic drugs are sufficient to precipitate angle closure by a mechanism similar to that of the cyclic antidepressants.6,8 The serotonergic effects of these drugs may also have a role in angle closure.11,14,16 Serotonin and serotonin receptors have been found in the human ciliary body, and serotonin, its agonists and antagonists do affect intraocular pressure.17 The supraciliary effusions documented here are evidence of the serotonergic effects of venlafaxine causing angle closure, although the precise cause for the effusions is unknown.
1 Ultrasound biomicroscopy images, Day 4 after the patient presented with acute angle closure
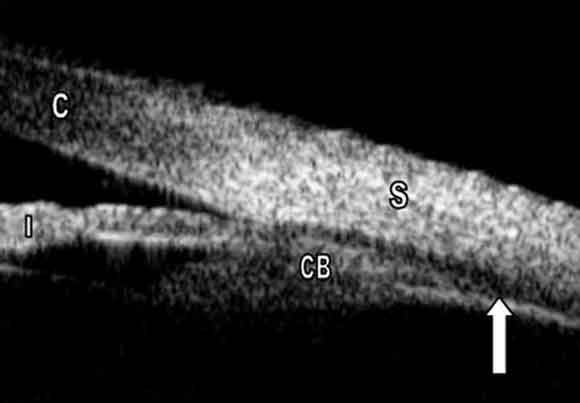
A: Supraciliary effusion, right eye (arrow). (C = cornea; CB = ciliary body; I = iris; S = sclera.)
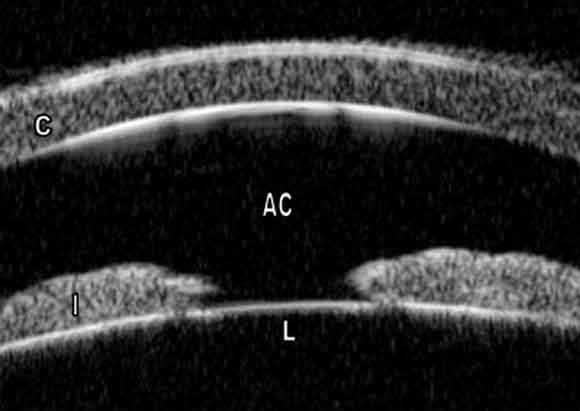
B: Shallow anterior chamber, left eye. The large area of iris–lens apposition indicates forward displacement of the lens. Pupil block has already been relieved by peripheral iridotomy (not shown). (AC = anterior chamber; C = cornea; I = iris; L = lens.)
- 1. Grebb JA. Venlafaxine. In: Kaplan HI, Sadock BJ, editors. Comprehensive textbook of psychiatry. 6th ed. Baltimore, Maryland: Williams and Wilkins,1995: 2120-2121.
- 2. Grant WM, Schuman JS. Toxicology of the eye. 4th ed. Springfield, Ill: Charles C Thomas, 1993.
- 3. Medeiros FA, Zhang XY, Bernd AS, Weinreb RN. Angle-closure glaucoma associated with ciliary body detachment in patients using topiramate. Arch Ophthalmol 2003; 121: 282-284.
- 4. Sankar PS, Pasquale LR, Grosskreutz CL. Uveal effusion and secondary angle-closure glaucoma associated with topiramate use. Arch Ophthalmol 2001; 119: 1210-1211.
- 5. Rhee DJ, Goldberg MJ, Parrish RK. Bilateral angle-closure glaucoma and ciliary body swelling from topiramate. Arch Ophthalmol 2001; 119: 1721-1723.
- 6. Postel EA, Assalian A, Epstein DL. Drug-induced transient myopia and angle-closure glaucoma associated with supraciliary choroidal effusion. Am J Ophthalmol 1996; 122: 110-112.
- 7. Craig JE, Ong TJ, Louis DL, Wells JM. Mechanism of topiramate-induced acute-onset myopia and angle closure glaucoma. Am J Ophthalmol 2004; 137: 193-195.
- 8. Ng B, Sanbrook GMC, Malouf AJ, Agarwal SA. Venlafaxine and bilateral acute angle closure glaucoma [letter]. Med J Aust 2002; 176: 241. <MJA full text>
- 9. Aragona M, Inghilleri M. Increased intraocular pressure in two patients with narrow angle glaucoma treated with venlafaxine [abstract]. Clin Neuropharmacol 1998; 21: 130-131.
- 10. Adverse Drug Reactions Advisory Committee. SSRIs and increased intraocular pressure. Aust Adverse Drug React Bull 2001; 20: 3.
- 11. Lewis CF, DeQuardo JR, DuBose C, Tandon R. Acute angle-closure glaucoma and paroxetine [letter]. J Clin Psychiatry 1997; 58: 123-124.
- 12. Kirwan JF, Subak-Sharpe I, Teimory M. Bilateral acute angle closure glaucoma after administration of paroxetine [letter]. Br J Ophthalmol 1997; 81: 252.
- 13. Eke T, Bates AK, Carr S. Acute angle closure glaucoma associated with paroxetine. BMJ 1997; 314: 1387.
- 14. Browning AC, Reck AC, Chisolm IH, Nischal KK. Acute angle closure glaucoma presenting in a young patient after administration of paroxetine [letter]. Eye 2000; 14(Pt 3A): 406-408.
- 15. Bennett HG, Wyllie AM. Paroxetine and acute angle-closure glaucoma [letter]. Eye 1999; 13(Pt 5): 691-692.
- 16. Eke T, Carr S. Acute glaucoma, chronic glaucoma, and serotoninergic drugs [letter]. Br J Ophthalmol 1998; 82: 976.
- 17. Costagliola C, Parmeggiani F, Sebastiani A. SSRIs and intraocular pressure modifications. Evidence, therapeutic implications and possible mechanisms [review]. CNS Drugs 2004; 18: 475-484.





We thank Dr John Grigg for the ultrasound biomicroscopy images.