A man who had been taking prescribed methadone for many years presented with a desquamating rash (predominantly affecting the hands and feet) complicated by cellulitis of the right leg. There have now been multiple reports of a similar rash among methadone users in Sydney. The cause remains unknown.
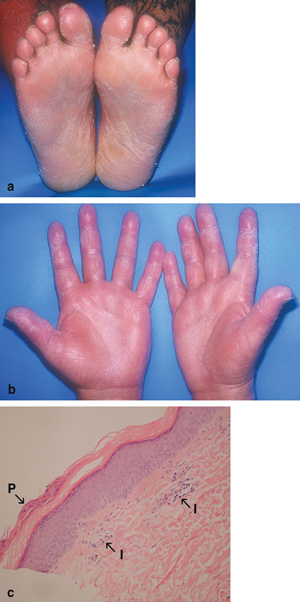
On physical examination, the patient was haemodynamically stable and looked well. His temperature was 37.2°C. There was erythema, tenderness and warmth below the right knee, consistent with cellulitis. There was desquamation of the skin of both his lower legs, soles of feet (Box, a) and palms and fingers (Box, b), as well as non-pitting oedema of the feet and hands. There was hyperkeratosis of the soles, with xerosis and an erythematous maculopapular rash of the arms. The skin condition did not appear typical of disorders causing hyperkeratosis and desquamation, which usually do not present concurrently. He had no mucosal ulceration. Differential diagnoses included the early phase of an exfoliative erythroderma, psoriasis triggered by infection, early pityriasis rubra pilaris, bacterial toxin-mediated exfoliation, viral exanthem, sarcoidosis and syphilis.
Skin biopsy of the red macules on his left arm (Box, c) and the right-leg biopsy revealed non-specific histological changes, suggestive of chronic dermatitis. Periodic acid–Schiff staining for fungi was negative.
This case raises the alert to a possible adverse reaction to a methadone preparation. The cause may be methadone itself, another component of the preparation, or a contaminant. Previously reported cutaneous reactions to methadone include angioedema, facial oedema, flushing, pruritus, purpura, rash and urticaria.1 To our knowledge, no cases have been reported of a desquamating rash associated with methadone or other opioids.
The cause of the reaction remains unknown, and is possibly even an illicit drug available on the street. However, as all affected patients appear to have been taking methadone, this is perhaps the most likely agent. Marijuana has been reported, albeit rarely, to cause allergic reactions, and occasionally becomes contaminated with biological or chemical substances that might cause a reaction.2 -4 However, in that situation, one would expect cases to be more widely distributed outside the methadone-using population. In addition, at least one client with this rash from the local methadone clinic had a negative urine test for cannabinoids (Mary Anne Ford, as above, personal communication).
- 1. Litt J, Pawlak WA. Methadone. In: Litt J, Pawlak WA. Drug eruption reference manual. New York: Parthenon Publishing Group, 1997: 271.
- 2. Liskow B, Liss JL, Parker CW. Allergy to marihuana. Ann Intern Med 1971; 75: 571-573.
- 3. Kagen SL. Aspergillus: an inhalable contaminant of marihuana. N Engl J Med 1981; 304: 483-484.
- 4. Taylor DN, Wachmuth IK, Yung-Hui S, et al. Salmonellosis associated with marijuana. N Engl J Med 1982; 306: 1249-1253.





We acknowledge the assistance of the Bayside Clinic, Sydney, NSW, and Dr Kim Tran, Department of Anatomical Pathology, St George Hospital, Sydney, NSW.
None identified.