Although cutaneous leishmaniasis is occasionally seen in Australia in overseas travellers and migrants, visceral leishmaniasis has been reported rarely and only in people who were immunocompromised. We describe an 18-year-old immunocompetent man who presented with pancytopenia and a 2-week history of fever and lethargy a year after visiting the Greek Islands. Visceral leishmaniasis was diagnosed after a bone marrow biopsy showed protozoa, and the patient responded well to treatment with liposomal amphotericin. To our knowledge, this is the first case of visceral leishmaniasis in an immunocompetent patient in Australia.
An 18-year-old man of Greek parentage presented with a 2-week history of dry cough, diarrhoea, lethargy, anorexia and fever. He had a past history of cutaneous vasculitis of uncertain aetiology and acne vulgaris. He was not taking any regular medication.
On examination, the patient’s temperature was 37.5°C, but no other abnormalities were evident. Investigations (Box 1) showed that he had pancytopenia, raised erythrocyte sedimentation rate and hypergammaglobulinaemia. The raised rheumatoid factor and anti-dsDNA levels were thought to be most likely related to inflammation.
Treatment was begun with intravenous ceftazidime and gentamicin because of the febrile neutropenia. A bone marrow biopsy performed on Day 2 to investigate the cause of the pancytopenia showed cellular bone marrow with relative erythroid hyperplasia. Multiple blood cultures gave negative results. As the fever persisted, roxithromycin was added to the regimen on Day 4, and vancomycin on Day 8. Serological testing was negative for multiple infections, including HIV infection, but positive for parvovirus B19 IgM, although negative for IgG, on Days 1 and 9.
The provisional diagnosis was parvovirus-related pancytopenia. The patient was discharged without antibiotic therapy 12 days after admission, as he felt well, although he still had a fever.
A month after discharge, the pancytopenia persisted. Repeated parvovirus B19 serological testing was negative for both IgM and IgG. A second bone marrow biopsy at this time revealed occasional macrophages containing amastigotes (the resting intracellular stage of leishmaniae, formerly known as Leishman–Donovan bodies; Box 2). Review of the first bone marrow biopsy specimen failed to show any protozoa.
Further questioning revealed that the patient had visited Greece for a 5-week holiday a year before presentation. A diagnosis was made of visceral leishmaniasis, probably acquired through sandfly bites. The patient was treated with liposomal amphotericin B, 250 mg daily for 4 consecutive days and then weekly for 2 weeks. The diagnosis was confirmed when promastigotes (the motile form of the organism) were successfully cultured. Leishmaniasis is not notifiable in Australia.
The patient’s blood count returned to normal 2 months after starting treatment with amphotericin. He remained well 2 years after ceasing treatment.
This case illustrates an unusual cause of pancytopenia in Australia. It is important to consider leishmaniasis as a differential diagnosis when the patient has a relevant travel history, as in this case. The diagnosis was not made on the first bone marrow biopsy, as smears from bone marrow usually contain few organisms, and have a sensitivity of 80%–85%.1
The major clinical syndromes caused by the genus Leishmania are cutaneous, mucosal and visceral leishmaniasis. Leishmaniasis is transmitted by Phlebotomus or Lutzomyia sandflies and infects dogs and foxes as well as humans. Numerous cases of cutaneous leishmaniasis have been reported in Australia,2,3 but to our knowledge only three cases of visceral leishmaniasis — one in a renal transplant patient4 and two in patients with HIV infection.5 Visceral leishmaniasis occurs in the Mediterranean region, northern Africa, the Middle East and central Asia, China and parts of South America.6
The differentiation of species causing leishmaniasis is complex and is performed only in reference laboratories. Visceral leishmaniasis is caused by Leishmania donovani, L. infantum or L. chagasi. L. infantum is the common species in the Mediterranean littoral and probably the cause of our patient’s infection.
The incubation period of visceral leishmaniasis is usually 2–8 months. Many infections are subclinical, but the classic presentation is with fever, weight loss, hepatosplenomegaly, pancytopenia and hypergammaglobulinaemia.
The definitive diagnosis depends on demonstrating either amastigotes in tissue or promastigotes in culture. Splenic puncture is the most sensitive means of obtaining a diagnosis, but biopsy of the bone marrow and liver is almost as good. In immunosuppressed individuals, promastigotes can sometimes be cultured from the buffy layer of centrifuged blood, and amastigotes can be seen in macrophages in biopsy specimens from various tissues. Testing for antileishmanial antibodies is not generally available and may be difficult to interpret.
Pentavalent antimony compounds have been used to treat leishmaniasis for decades, but often have severe side effects, and resistance is developing.7 The aminoglycoside aminosidine (also known as paromomycin) is also effective when used either alone or in combination with an antimonial compound.7 Amphotericin can achieve 98% long-term cure in both antimonial-unresponsive and previously untreated patients.7 Lipid formulations of amphotericin are the most active antileishmanial agents.8
Although leishmaniasis is rare in Australia, it needs to be considered as a possible differential diagnosis of pancytopenia, remembering that the disease can present up to several years after return from an affected area. If untreated, visceral leishmaniasis is potentially fatal.
1 Investigations in a patient with visceral leishmaniasis
Investigation |
Result |
Reference range |
|||||||||||||
Haemoglobin level (g/L) |
82 |
135–175 |
|||||||||||||
Total white cell count (cells/L) |
2.2 × 109 |
4–11 × 109 |
|||||||||||||
Neutrophil count (cells/L) |
0.8 × 109 |
2.0–7.5 × 109 |
|||||||||||||
Platelet count (cells/L) |
106 × 109 |
150–400 × 109 |
|||||||||||||
Erythrocyte sedimentation rate (mm/h) |
120 |
0–15 |
|||||||||||||
Antinuclear antibody titre |
1/160 |
< 1/160 |
|||||||||||||
Anti-dsDNA level (IU/mL) |
10 |
< 8 |
|||||||||||||
Rheumatoid factor level (kIU/L) |
240 |
< 20 |
|||||||||||||
IgG level (g/L) |
19.1 |
6.5–16.0 |
|||||||||||||
IgA level (g/L) |
4.3 |
0.6–4.0 |
|||||||||||||
2 Bone marrow biopsy in visceral leishmaniasis
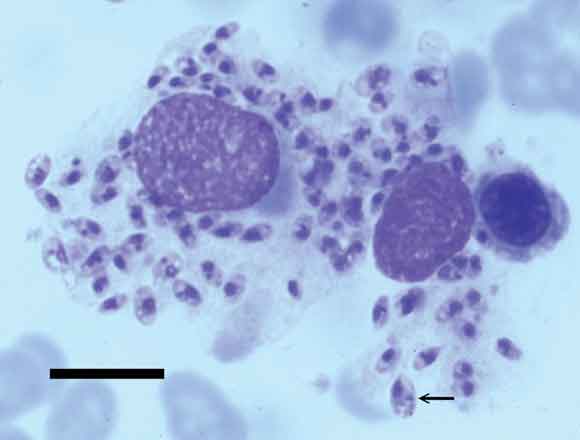
Light micrograph of bone marrow, showing macrophages containing amastigotes characteristic of Leishmania spp. Amastigotes are the non-flagellated intracellular stage of the protozoan, formerly known as Leishman–Donovan bodies. They appear as spherical or oval organisms 2–6 μm in length that contain two darker-staining organelles — a nucleus and a kinetoplast (arrow). The latter is a distinct region of the mitochondria containing mitochondrial DNA. (Giemsa stain; scale bar = 10 μm.)
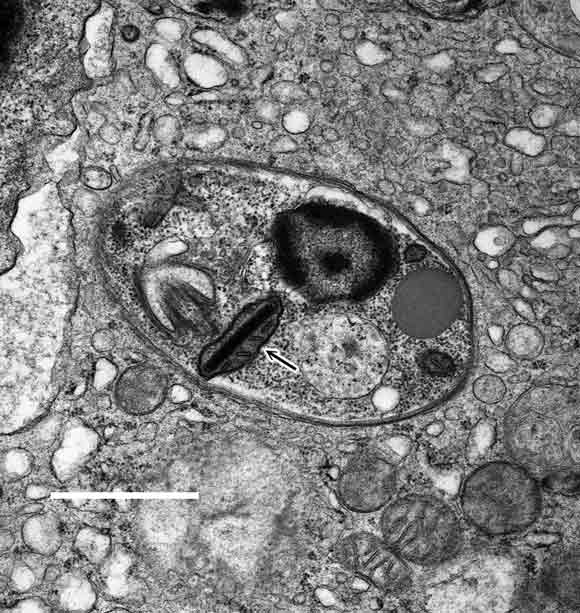
Transmission electron micrograph of bone marrow, showing an amastigote with a kinetoplast characteristic of Leishmania spp. (arrow). (Scale bar = 1 μm.)
- 1. Magill AJ. Leishmaniasis. In: Strickland GT, editor. Hunter's tropical medicine and emerging infectious diseases. 8th ed. Philadelphia, Pa: WB Saunders, 2000: 665-687.
- 2. Maguire GP, Bastian I, Arianayagam S, et al. New World cutaneous leishmaniasis imported into Australia. Pathology 1998; 30: 73-76.
- 3. Jones HI. Cutaneous leishmaniasis in Western Australia. Med J Aust 1979; 2: 495-496.
- 4. Ma DD, Concannon AJ, Hayes J. Fatal leishmaniasis in renal transplant patient. Lancet 1979; 2: 311-312.
- 5. Matthew G, Marriott D, Cooper D. Visceral leishmaniasis in HIV infected patients. A report of the first two Australian cases [abstract]. Annu Conf Australas Soc HIV Med 1996; 45: 14-17.
- 6. Bryceson ADM. Leishmaniasis. In: Cook GC, editor. Manson’s tropical diseases. 20th ed. London: WB Saunders, 1996: 1213-1245.
- 7. Rosenthal E, Marty P. Recent understanding in the treatment of visceral leishmaniasis. J Postgrad Med 2003; 49: 61-68.
- 8. Minodier P, Retornaz K, Horelt A, et al. Liposomal amphotericin B in the treatment of visceral leishmaniasis in immunocompetent patients. Fundam Clin Pharmacol 2003; 17: 183-188.





None identified