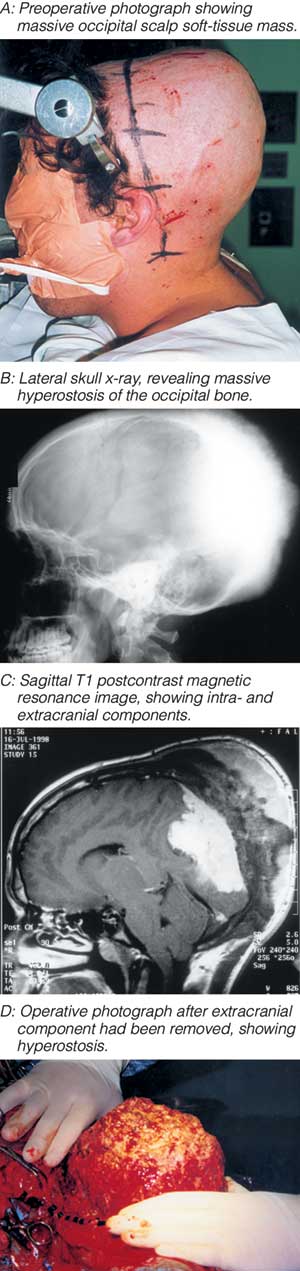
X-rays, computed tomography and magnetic resonance imaging further delineated the anatomy of the lesion (Box, B,C). Volume estimation1 yielded a total volume of 1094 cm3, making this one of the largest meningiomas ever reported.
The patient was given high-dose corticosteroids, and surgical excision was undertaken in two stages. At the first operation, the extracranial component and most of the hyperostotic bone were removed (Box, D). A week later, the remainder of the tumour was removed and the involved (and occluded) superior sagittal sinus resected. The postoperative period was complicated by a cerebrospinal fluid (CSF) leak and meningitis, requiring replacement of the artificial dural graft with fascia lata and CSF diversion with a lumbar drain.
Histopathological examination of the tissue revealed a meningothelial meningioma with no atypical features. As a Simpson grade II removal (complete resection of macroscopic tumour with diathermy of the dural origin)2 had been achieved, no adjuvant treatment was given.
Six months later, an acrylic cranioplasty was performed, and at 2-year follow-up the patient was well. His visual acuity had returned to 6/36 and his visual fields had expanded.
Meningiomas account for about 20% of all intracranial tumours3 and, as slow-growing tumours that display benign behaviour, can escape notice.
Hyperostosis is often palpable through the scalp, but this patient had an unusually large extracranial volume of tumour (more commonly associated with malignant meningiomas,4 which often lack a significant intracranial component).
Complete surgical excision of meningiomas has been shown to offer the best long-term outcome compared with subtotal excision with or without radiotherapy.5 However, even with optimum surgical excision, recurrence rates of up to 20% can be expected over a 20-year period.6
- Rodney S Allan1
- Peter J Spittaler2
- Lindsay J Rowe3
- 1 Department of Neurosurgery, Westmead Hospital, Westmead, NSW.
- 2 John Hunter Hospital, New Lambton, NSW.
- 1. Siemens statistical package. Somatom Plus 4 computed tomography scanner. Munich, Germany: Siemens Medical Solutions, 1998.
- 2. Simpson D. The recurrence of intracranial meningioma after surgical treatment. J Neurol Neurosurg Psychiatry 1957; 20: 22-39.
- 3. Longstreth WT Jr, Dennis LK, McGuire VM, et al. Epidemiology of intracranial meningioma. Cancer 1993; 72: 639-648.
- 4. Younis G, Sawaya R. Intracranial osteolytic malignant meningiomas appearing as extracranial soft-tissue masses. Neurosurgery 1992; 30: 932-935.
- 5. Condra KS, Buatti JM, Mendenhall WM, et al. Benign meningiomas: primary treatment selection affects survival. Int J Radiat Oncol Biol Phys 1997; 39: 427-436.
- 6. McCarthy BJ, Davis FG, Freels S, et al. Factors associated with survival in patients with meningioma. J Neurosurg 1998; 88: 831-839.