Medical education is undergoing significant change, with curriculum redevelopment and the introduction of new teaching methods, including enhancement with computer-based programs and increasingly sophisticated task trainers and simulators. Leading the change in new teaching techniques is simulation technology.1-3 Simulators themselves are costly, as is maintaining appropriately trained staff in a realistic clinical environment, with appropriate audiovisual support. Governments, universities and professional medical, nursing and paramedical colleges and societies are likely to acquire such sophisticated training capabilities only through a collaborative approach. In this article we describe the development and operation of a purpose-built medical simulation and skills centre known as “CASMS”, the Centre for Anaesthesia Skills and Medical Simulation, at the Clinical Training and Education Centre (CTEC), University of Western Australia.
CASMS began with one adult anaesthesia simulator and some disused operating equipment in a vacated nursing school building. It was staffed by a core group of six anaesthetists and one registered nurse on secondment from Royal Perth Hospital. This first simulation suite was used for more than a year while a new simulation and skills facility was built. The new building was a major structural addition to the Department of Anatomy and Human Biology at the University of Western Australia. The simulation centre is located on the first floor and a state-of-the-art surgical workshop and lecture room are located on the ground floor. This multidisciplinary medical training facility (CTEC) was officially opened on 1 April 2000.
CASMS contains three complete and independent simulation suites, a skills area, a conference room and an administration area (Box 1). Each suite comprises a simulation room, which can be presented and equipped as an operating theatre, emergency department resuscitation area, recovery room, endoscopy suite, medical practitioner’s office, or any other area as the training need requires. An adjoining control room allows course leaders to observe participants, control events, manipulate mannequins remotely, and communicate to role-playing training staff in the simulation room via wireless headsets. An adjacent “debriefing” room is used for tutorials, discussions and formal debriefing sessions after each scenario.
A simulation and skills centre may contain as many pieces of hospital equipment, medical training simulators, mannequins, and training aids as the facility can afford. Box 2 contains a list of some high-cost equipment and training aids used in courses and workshops offered by CASMS. The high-fidelity anaesthesia simulator has been a very flexible training device. It can easily simulate more than 35 medical and anaesthesia crises (eg, bronchospasm, pneumothorax, malignant hyperthermia, pericardial tamponade, aspiration, and all cardiac arrhythmias). It is now reserved for selected operating theatre scenarios and the Laerdal SimMan is used for most resuscitation courses for medical students, nurses and trainee doctors. Miscellaneous equipment (such as a fog machine to simulate hospital fires or chemical agent dispersion, and a moulage kit to simulate various wounds) has been acquired to increase the variety and authenticity of scenarios.
The courses offered and their target groups are wide-ranging. Courses were initially configured for trainee and consultant anaesthetists, but were quickly tailored to suit the requirements of other acute-care medical and nursing staff. Examples of courses offered include crisis management (for anaesthetists, anaesthesia technicians and critical care nurses), refresher courses in industrial emergencies for industrial paramedics, cardiac defibrillation (for registered nurses), and urinary catheterisation (for medical students). The numbers of courses and participants have grown from 69 courses offered in 2000, involving 471 participants, to 170 courses in 2002, involving 1711 participants.
The simulation centre is ideally designed for any type of training that requires a hospital environment (operating theatre, emergency department, intensive care unit) or a general medical or dental practice. The courtyard area adjacent to CASMS and a service stairway to the air-conditioning plant in the CASMS building have also been used for prehospital or industrial (eg, off-shore oil rig) scenarios for paramedics.
The scenario-based training was pioneered by Gaba and colleagues at Stanford University.4 This novel style of medical training was well known in aviation and other high-risk industries that involved complex work environments requiring active decision-making. After a period of familiarisation with the simulator and discussion of strategies for managing medical crises, participants take turns at experiencing a medical crisis in an environment that matches their workplace. The scenarios are usually audiotaped and videotaped in real time. Segments of the crisis are replayed where appropriate during facilitator-managed debriefing sessions. An example of a medical crisis during a routine dental procedure (from a “Medical emergencies during dental practice” course) is shown in Box 3.
There is increasing awareness of the need for improved patient safety among the general public and medical defence organisations. Simulation centres play a valuable role in providing a safe environment for training without risk to the patient.5 The ability of simulation centres to repeatedly present rare and unusual cases to participants is also valuable, at a time when inpatient numbers are declining and fewer real “cases” are available for students and junior staff to experience.
However, for simulation centres to maintain high standards and to continue improving the quality of training available, access to a simulation centre must be increased for the wider medical and nursing community. Scenario-based training requires a dedicated area that appears no different from the clinical domain that it represents. Medical and audiovisual equipment demands are such that it makes sense to build a dedicated clinical area that is flexible enough to be modified according to the setting, and is well-equipped for inconspicuous videotaping of clinical events. At least one separate area for small-group teaching and post-event discussion is also required. Debriefing sessions are essential in scenario-based training, and are regarded as the most difficult role for instructors. Training in debriefing techniques should be acquired before undertaking scenario-based training.
Sufficient funds to construct several simulation suites in a centre allows for more efficient use of resources. Ideally, surgical skills centres would be collocated with medical simulation centres to foster interdisciplinary courses, and to share support services and lecture rooms. The use of web-based learning materials to be completed before attending the centre also leads to more efficient use of the simulator centre.
Worldwide, there are over 150 centres with high-fidelity simulators and more than a third of medical schools in the United States have at least one simulator. In Mainz, Germany, a shared medical and aviation simulation centre has been established. In Australasia, simulation and/or medical skills centres operate cooperatively and share expertise and even instructors. Currently, the centres are: Southern Health Simulation and Skills Training Centre (Monash Medical Centre, Melbourne); St Vincent’s Simulation Centre (St Vincent’s Hospital, Melbourne); Sydney Medical Simulation Centre (Royal North Shore Hospital, Sydney); National Patient Simulation Training Centre (Capital Coast Health, Wellington, New Zealand); and Flinders Clinical Skills and Simulation Unit (Flinders University, Adelaide). New simulation centres are planned for Brisbane (Queensland) and Auckland (New Zealand).
Flexibility of educational style is important, and the input of a dedicated medical educationalist is of great benefit. Gaba’s scenario-based training methods are only suitable for some courses, and assessment of individual and group performance during simulator-based medical emergencies is complex.6,7 Other methods, such as problem-based learning, may be particularly appropriate for medical students,8,9 and outcomes-based learning should be considered as a method of guiding the content of courses and assessment of participants. Continuing development of simulation-specific assessment tools and evaluation of courses are vital.
Remediation for professionals with specific needs is also an area that should be further considered by simulation centres. Simulation centres are ideal for fully assessing individual need in a safe environment and for providing learning opportunities to remedy specific problems.10,11
In conclusion, medical simulation centres have a significant contribution to make at all levels of training for healthcare professionals. Despite large start-up and maintenance costs, the increasing need for such collaborative skills centres will ensure their continued success in the Australian healthcare system.
1: Floor plan and images of the Centre for Anaesthesia Skills and Medical Simulation (CASMS), University of Western Australia
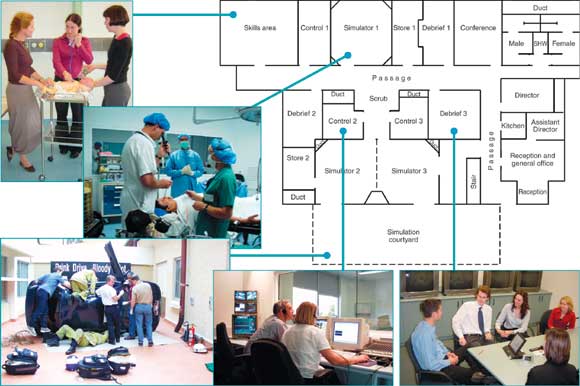
(Architectural drawing copyright, John Flower Architect Pty Ltd)
2: High-cost equipment used at the Centre for Anaesthesia Skills and Medical Simulation, University of Western Australia
Equipment |
Approximate cost ($) |
||||||||||
MedSim high-fidelity anaesthesia simulator (adult simulator with drug recognition and responses, physiological data output, preprogrammed crises) |
$250 000 |
||||||||||
Laerdal SimMan (a medium-fidelity simulator, numerous cardiorespiratory features) |
$85 000 |
||||||||||
Laerdal MPL Crash Kelly (a robust adult mannequin, useful for basic life support and pre-hospital training) |
$5 200 |
||||||||||
Laerdal Airway Management Trainer (bag-mask ventilation, tracheal intubation) |
$2 700 |
||||||||||
Laerdal MPL Megacode Kid with multi sounds (paediatric CPR trainer) |
$13 600 |
||||||||||
Laerdal ALS baby trainer with Heartsim 200 simulator (paediatric arrhythmia trainer) |
$4 400 |
||||||||||
Laerdal Little Anne (basic life support trainer) |
$1 250* |
||||||||||
Datex Ohmeda AS/3 anaesthesia machine |
$67 000 |
||||||||||
Datex Engstrom AS/3 patient monitor, including anaesthetic agent and gas analyser |
$45 000 |
||||||||||
Datex Engstrom CS/3 patient monitor |
$36 000 |
||||||||||
Drager Evita 4 ventilator (ICU ventilator) |
$27 500 |
||||||||||
Drager Oxylog 2000 (a patient transport ventilator) |
$14 500 |
||||||||||
Hewlett Packard Codemaster 100 defibrillator |
$11 000 |
||||||||||
Phillips Heartstream FR4 defibrillator |
$4 000 |
||||||||||
Olympus fibreoptic bronchoscope, monitor, light source and camera control unit |
$36 700 |
||||||||||
* Cost for 5. CPR = cardiopulmonary resuscitation. |
|||||||||||
3: Dental scenario: a cardiac event during a routine dental procedure
 Setting: A 55-year-old man with known heart disease undergoes a prolonged dental procedure. The patient complains of chest discomfort and the dental nurse notices that the patient has been sweating and now appears grey. He is then unresponsive, pulseless and apnoeic. The dentist and nurse start cardiopulmonary resuscitation (CPR) after a pocket mask is found in a drawer. They call for help from the receptionist. An ambulance is not called. The scenario is stopped when the instructor detects effective ventilation and cardiac compressions. Debriefing: The facilitator (F) asks the dentist (D) to describe to the group (observing via videolink from a nearby room) what happened and what he was thinking. Laerdal SimMan adult simulator in a dental chair → |
|||||||||||
F: “Let’s go over what just happened.” |
D: “The patient crashed on me.” |
||||||||||
F: “When did you first realise you had a crisis?” |
D: “When he didn’t answer the nurse’s question.” |
||||||||||
F: “What type of emergency was it?” |
D: “A cardiac emergency.” |
||||||||||
F: “What clues were you given that something like this might happen?” |
D: “He had a history of heart disease and the procedure was long and stressful. Apparently he was sweating a lot, but I didn’t realise that”. |
||||||||||
F: “Were you prepared for this?” |
D: “I am a bit shaky on my CPR skills and you never hear of patients having an arrest in the chair, do you? We are not really prepared for this sort of thing anyway. I don’t even know if our receptionist could do much to help out if something like this happens.” |
||||||||||
A segment of the scenario (patient stops breathing) is replayed. |
|||||||||||
F: “What do we learn from this?” |
D: “There was a long delay before we did anything. I was distracted with the job and then I couldn’t believe this was really happening. I guess we didn’t know where our emergency gear is kept. We don’t have much gear anyway. We should have called for an ambulance.” |
||||||||||
F: “How could we improve our ability to handle medical emergencies?” |
D: “Have a ‘resus’ kit in clear view, make sure our staff get some training, and organise a system in our practice to follow when this happens”. |
||||||||||
A discussion follows on emergency equipment needed for dental practices and staff training. |
|||||||||||
- Richard H Riley1
- Amanda M Grauze2
- Neil H Trewhella3
- Claire Chinnery4
- Ross A Horley5
- 1 Centre for Anaesthesia Skills and Medical Simulation (CASMS), Clinical Training and Education Centre (CTEC), University of Western Australia, Perth, WA.
- 2 Medic Vision Ltd, South Perth, WA.
Ross Horley is the Director of Medic Vision Ltd, a specialist audiovisual engineering company.
- 1. Issenberg SB, McGaghie WC, Hart IR, et al. Simulation technology for health care professional skills training and assessment. JAMA 1999; 282: 861-866.
- 2. Watterson L, Flanagan B, Donovan B, Robinson B. Anaesthetic simulators: training for the broader health-care profession. Aust N Z J Surg 2000; 70: 735-737.
- 3. Riley R. The use of simulators in medicine. In: Keneally J, editor. Australian anaesthesia. Melbourne: ANZCA, 2000.
- 4. Howard SK, Gaba DM, Fish KJ, et al. Anesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviat Space Environ Med 1992; 63: 763-770.
- 5. Gaba DM. Anaesthesiology as a model for patient safety in health care. BMJ 2000; 320: 785-788.
- 6. Schwid HA, Rooke GA, Carline J, et al. Evaluation of anesthesia residents using mannequin-based simulation. Anesthesiology 2002; 97: 1434-1444.
- 7. Kapur PA, Steadman RH. Patient simulator competency testing: ready for take off? Anesthes Analges 1998; 86: 1157-1159.
- 8. Rendas A, Pinto PR, Gamboa T. A computer simulation designed for problem-based learning. Med Educ 1999; 33: 47-54.
- 9. Tome J, Fletcher J. Virtual PBL: full-scale human simulation technology. Acad Med 1996; 71: 523.
- 10. Rosenblatt MA, Abrams KJ. New York State Society of Anesthesiologists, inc; Committee on Continuing Medical Education and Remediation; Remediation Sub-Committee. The use of a human patient simulator in the evaluation of and development of a remedial prescription for an anesthesiologist with lapsed medical skills. Anesthes Analges 2002; 94: 149-153.
- 11. Hanna E, Premi J, Turnbull J. Results of remedial continuing medical education in dyscompetent physicians. Acad Med 2000; 75: 174-176.





Abstract
Medical simulation is a relatively new teaching modality suitable for medical education at all levels, although its long-term benefits have not yet been validated.
Simulation allows the participant to practise diagnosis, medical management and behavioural approaches in the care of acutely ill patients in a controlled environment.
Simulators have achieved widespread acceptance in the fields of anaesthesia, intensive care and emergency medicine. More recently, team training for pre-hospital and within-hospital multidisciplinary medical response teams has become popular.
The increasing number and diversity of courses at “CASMS” parallels the evolution of simulation centres into regional clinical skills centres elsewhere. Such centres are likely to become a cost-effective means of achieving greater consistency in medical skill acquisition and may improve patient outcomes after medical crises.