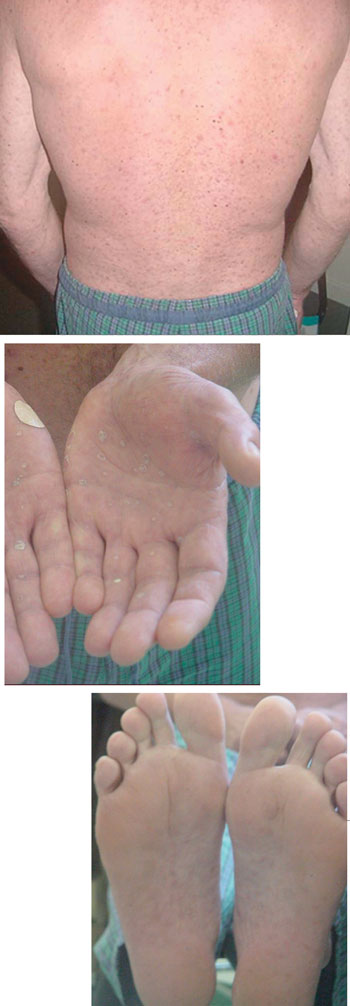
Classic presentation of secondary syphilis: macular, symmetrical rash on the back, palms, and soles. (NB: These photographs are not of the patient reported, who did not have a rash on his hands. However, the rashes he had on his back and feet were very similar to those shown.)
In this patient, syphilis was unmasked by the Jarisch–Herxheimer reaction after ceftriaxone therapy for rectal gonorrhoea. The Jarisch–Herxheimer reaction is a self-limiting febrile reaction occurring 4–8 hours after penicillin treatment in 95% of early (primary and secondary) syphilis cases. The pathogenesis is unknown although lysis of the spirochaete, releasing endotoxin, probably contributes to the systemic illness. As the patient had no laboratory confirmation of syphilis at the time of presentation, we made this diagnosis based on (i) the acute onset and systemic nature of the symptoms of fever, malaise, chills, rigors, myalgia, and headache, occurring 6 hours after ceftriaxone injection; and (ii) the complete resolution of symptoms within 24 hours — all characteristic features of this reaction.
Secondary syphilis occurs as the spirochaete disseminates from the site of infection (chancre) via blood and lymph nodes. A characteristic symmetrical macular rash (often on palms and soles) occurs 4–10 weeks after the appearance of the chancre. Less common symptoms include malaise, myalgia, pharyngitis, headache, lymphadenopathy, condylomata lata (which may mimic genital warts), oropharyngeal snail-track ulcers and, rarely, generalised pruritis. However, the diagnosis of secondary syphilis in this patient was clinical and based on (i) the Jarisch–Herxheimer reaction; and (ii) the appearance of the characteristic body and plantar rash (see Box), which intensified during treatment and desquamated before disappearing with successful treatment. Primary syphilis was excluded as there were no chancres.
Because the systemic symptoms of the Jarisch–Herxheimer reaction and those of secondary syphilis are similar and overlap, delineating where the former "ends" and where the latter "starts" is not always clear-cut. The symptoms of secondary syphilis may increase during the Jarisch–Herxheimer reaction.
The recommended treatment for early syphilis is 1 g procaine penicillin intramuscularly for 10 days.1 In our patient, the attending physician decided on a longer course and higher dose because the patient's HIV viral load was > 100 000 copies/mL and the CD4 count (350 × 106/L) was low.
The efficacy of ceftriaxone in primary and secondary syphilis is comparable with that of intramuscular penicillin,2,3 and ceftriaxone is used in treating penicillin-allergic patients in the United States4 and Europe.5 One case of Jarisch–Herxheimer reaction after ceftriaxone therapy for primary syphilis has been reported;6 however, to the best of our knowledge, this adverse reaction to ceftriaxone has not previously been reported in Australia.
The incidence of syphilis is increasing among homosexually active men in some large cities overseas (eg, Los Angeles).7 In south-eastern Sydney in 2002, 20 of the 119 notifications of syphilis received to August were classified as new infectious cases, compared with a total of 19 infectious syphilis cases notified for the whole of 2001.8
Local guidelines for sexual health testing have been established in response to concurrent gonorrhoea and hepatitis A epidemics in south-eastern Sydney.9 Screening for sexually transmitted infections is recommended at least annually among homosexually active men.
All patients receiving intramuscular antibiotic treatment for early syphilis should be forewarned about the Jarisch–Herxheimer reaction. Without this reaction, syphilis may have been missed in this patient, had he not returned for serological tests a week later, as prearranged. Ideally, in this high-risk, symptomatic patient, serological tests for syphilis should also have been done at his initial presentation.
In conclusion, the main lesson from this case is the need for full screening for sexually transmitted infections in all high-risk patients presenting with anogenital symptoms.
- Derek J Chan1
- Harry M Michelmore2
- Julian Gold3
- Department of HIV Medicine, Albion Street Centre, Sydney, NSW.
- 1. The Venereology Society of Victoria and The Australasian College of Sexual Health Physicians. National management guidelines for sexually transmissible infections. Melbourne: The Venereology Society of Victoria, 2002.
- 2. Marra GM, Boutin P, McArthur JC, et al. A pilot study evaluating ceftriaxone and penicillin G as treatment agents for neurosyphilis in human immunodeficiency virus-infected individuals. Clin Infect Dis 2000; 30: 540-544.
- 3. Dowell ME, Ross PG, Musher DM, et al. Response of latent syphilis or neurosyphilis to ceftriaxone therapy in persons infected with human inmmunodeficiency virus. Am J Med 1992; 93: 481-488.
- 4. Gilbert DN, Moellering RC Jr, Sande MA. The Sanford guide to antimicrobial therapy 2001. 31st ed. Hyde Park, Vt: Antimicrobial Therapy Inc, 2001.
- 5. Goh BT, van Voorst Vader PC; European Branch of the International Union against Sexually Transmitted Infections and the European Office of the World Health Organization. European guideline for the management of syphilis. Int J STD AIDS 2001; 12 Suppl 3: S14-S26.
- 6. Bader U. Atypical manifestation of primary syphilis. Am J Med 2000; 108: 521-522.
- 7. Chen JL, Kodagoda D, Lawrence MA, et al. Rapid public health interventions in response to an outbreak of syphilis in Los Angeles. Sex Transm Dis 2002; 29: 277-284.
- 8. South Eastern Sydney Public Health Unit. Public Health Update, August-September 2002; 9(4): 2.
- 9. Sexually Transmissible Infections in Gay Men Action Group (STIGMA). Sexually transmitted infection testing guidelines for men who have sex with men, 2002. Available at: www.sesahs.nsw.gov.au/publichealth/infectiousdiseases/STIguidelines.htm (accessed Mar 2003).




