We do not suggest giving up on the training and education of health workers as a means of development. Examining why training has failed can help us design and implement better training programs, and our experience suggests that we need to refocus training on what is appropriate, use better educational methods and support training with coordinated work on other health system issues, such as policy development and introduction of essential infrastructure.
Training often fails when it targets the wrong people, or teaches the wrong content. Early attempts to reduce maternal mortality concentrated significant effort on short workshops to give traditional birth attendants some basic skills in antenatal assessment and delivery care. These failed to prevent maternal deaths. Not only was it almost always impossible to predict which women would develop life-threatening complications, but, if such a complication did ensue, "basic" delivery skills exercised in a village would be insufficient to save a life.1 However, it has proven essential to include such health workers in training programs to enable access at the most peripheral levels to the health knowledge that poor communities lack.
Getting the right "who" trained in the right "what" is crucial, and good planning, based on good science, is essential. Unfortunately, many training-needs assessments stop at simply asking senior health managers what they think their staff should know. More is required, including careful attention to matching health worker competencies with community health needs, planning training methods that are likely to be effective and sustainable, and planning to evaluate not just the training program itself but its outcomes in terms of the objectives of the health system. In addition, the resources, anxieties and environment of those who will take part should all be considered.
The traditional medical school focus on precise diagnosis and pertinent treatment is often less appropriate than a syndromic approach. For example, simply counting the respiratory rate has been found to be just as useful a sign for assessing the presence of childhood pneumonia as stethoscopic auscultation by an expert. When combined with two other signs — the presence of stridor and lower chest wall indrawing — this produces a powerful algorithm. So, with no more equipment than a watch or minute timer, a health worker can assess a child with cough, classify the presence of pneumonia with around 80% sensitivity and 90% specificity, and decide on treatment, such as antibiotic or referral.2 In a world where around a fifth of early-childhood deaths are caused by acute respiratory infections, training rural health workers in this syndromic approach has been shown to produce significant declines in mortality rates of children under five.3
Outstanding work by WHO and UNICEF, as well as individual scientists, has allowed such research to be synthesised into the Integrated Management of Childhood Illness (IMCI) approach.4 This robust tool helps health workers tackle 70% of the causes of early-childhood mortality with a syndromic approach to the five most common presenting problems: cough, diarrhoea, fever, ear problems and malnutrition. Many agencies are developing similar evidence-based strategies for health concerns in developing countries, including sexually transmitted diseases, pregnancy and childbirth, adult lung disease and HIV/AIDS.
Such approaches make sense, especially if sufficient time is spent on adaptation to the local situation.5 However, they may not always be welcomed with open arms. Syndromic approaches and special programs for resource-poor settings may be seen as demeaning or cheap if not discussed thoroughly. They may clash with established traditions of health training.
For example, for some Asian health practitioners, the most important part of their evidence base is not the faith they have in the randomised-controlled trial but the respect they hold for the authority of their teacher. Accordingly, one can spend hours discussing the science of pharmacokinetics with local doctors in an attempt to rationalise prescribing, only to have them dismiss this evidence on the basis that "it doesn't apply here".
Training often fails for the simple fact that teaching does not equate with learning. There is a particular hazard that afflicts in-service training in resource-poor settings: when the "educated" trainer forgets that the rural health workers under his tutelage are adults, often with considerable skill and experience.
Adults learn best when their own motivation is supported, their active participation is encouraged, their experience is valued and the content is relevant to their daily work.6 Thus, the focus in programs must shift from the trainer's teaching to the participant's learning. David Werner's ground-breaking work encapsulated this in its title, Helping health workers learn,7 and has been extended by others into concepts such as the "transfer of learning".8 The competency-based training approach helps to ensure that learning generates new knowledge and skills that relate to real workplace needs.9
A well-constructed, practical, participatory workshop can be an empowering means of introducing new ideas, such as having an essential drugs list, or practical skills, such as immunisation program tasks. Strategies that emphasise "learning by doing" and problem-solving are particularly useful in building competencies needed by health workers in resource-poor settings.10,11
In-service training activities of this nature take time, resources and depend greatly on the quality of the teaching. Where resources have been limited, programs have used a "cascade" approach, where central, core trainers are trained well, once, and are then expected to train others, who then train others and so on. Cascade approaches have often failed, because it proves impossible to guarantee the training quality, which is so essential to success, throughout the levels of training. A shortened cascade, where external trainers implement training in partnership with local trainers whose capacity they have developed, may be a reasonable compromise where widespread, rapid retraining is required (see Box 1).
A good participatory training program can improve health worker competencies; but very often this does not lead to improved health system performance because of a variety of "external" factors. These include formal and informal health policies, particularly policies that affect health financing for communities and cost recovery for health facilities.
Essential facilities, equipment and supplies are clearly crucial to enabling the translation of improved competencies into changed workplace practices. The private sector, personal motivation, pay (or lack of it) and career prospects are all other major influences on whether health workers can or will put learning into practice.
Our review has focused on in-service training, because that is what many development programs offer. However, pre-service and post-basic training and education are other, underused entry points with great potential for the introduction of new ideas and approaches.
Also, in many countries, it may be possible to integrate in-service training into systems that allow health workers to acquire post-basic qualifications. This has the potential to link promotion and pay motivations to the acquisition of new skills, with increased likelihood of improved health worker practice.
Several alternative strategies for health worker learning that link with other health system action are being introduced to development programs. The most effective are those that maximise learner input to content and method and are located as close as possible to the workplace and its problems. Some examples include short practical learning sessions linked to monthly reporting or "pay-day" visits; "supportive supervision" visits structured and resourced to build health worker capacity through practical help and feedback of information; "mentoring" by senior or expatriate staff or "coaching" by peers. One coaching program in Indonesia sent experienced nurses to provide peer-to-peer support in underperforming health centres. The program was associated with a 39% increase in vaccination coverage rates.13
The use of information technology for distance learning is beyond the scope of this article, but deserves consideration in situations where local resources are able to sustain it.
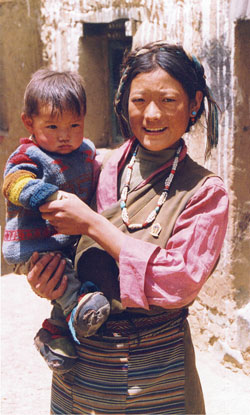
The village health clinics that Australian funds did build in Tibet were not very easy to see — they were small and mostly built from mud-brick, not at all large nor erected in concrete. Yet, we were more than satisfied with this feedback from a rural health worker:
Even better evidence of the worth of "invisible development" was found in the marked increase in the number of rural women who chose a newly trained midwife to assist their delivery in a well-equipped clinic.14 When the light is right, you can see training.
1: Immunisation in PNG: a cascade approach12
Over the past four years, the governments of Australia and Papua New Guinea (PNG) have been investing considerable resources into rehabilitation of PNG's immunisation program. Retraining the entire rural workforce in the use of new equipment, policies and procedures is an essential, but extraordinarily difficult, component of this. An Australian aid program in PNG is using a modified cascade approach for the revitalisation of immunisation services across the country.
Initially, the plan was to train a few trainers in each of PNG's 20 provinces, who would then train district-level staff, who would, in turn, then train the health workers — a classic "cascade" system. However, evidence from other health worker in-service training suggested that there would be a rapid attenuation in quality and quantity of training and was likely to fail. So, the program was reshaped so that a small national team of immunisation "core trainers" worked to develop district trainers in each province. Subsequent workshops for rural health workers are using a "partnership" model — core trainers conduct training for rural staff, together with the new district trainers, until it is clear that the district trainers are comfortable conducting refresher training on their own.
2: Vaccination in PNG: linking training to policy and practicalities12
Rehabilitation of the vaccination program in PNG will be dependent on much more than training alone. Much needed to be in place before training could begin: most rural clinics have received new types of equipment for vaccine storage and injection. Vaccine distribution systems have been reinvented. Policies for when vaccines are given have been updated and a health-worker reference manual developed. Conversely, none of this revamp would be effective without practical, participatory, skills-oriented refresher training of health workers.
Although the success of the PNG training program will depend on the use of effective methodology and adequate support, its ultimate success is also dependent on a multitude of external factors, including transport infrastructure and security. These factors must also be addressed if the training program and the rehabilitation of equipment and vaccination systems are to achieve the objective of increased vaccination coverage.
- Christopher J Morgan1
- Peter W Deutschmann2
- 1 Centre for International Health, Macfarlane Burnet Institute for Medical Research and Public Health, Melbourne, VIC.
- 2 Australian International Health Institute, University of Melbourne, Parkville, VIC.
Both authors have current involvement with international development programs, including those funded by AusAID and the World Health Organization.
- 1. Maine D. What's so special about maternal mortality? In: Berer M, Sundari Ravindnan JK, editors. Safe motherhood initiatives: critical issues. Oxford: Blackwell, 1999: p175-182.
- 2. Weber MW, Mulholland EK, Jaffar S, et al. Evaluation of an algorithm for the integrated management of childhood illness in an area with seasonal malaria in the Gambia. Bull World Health Organ 1997; 75 Suppl 1: 25-32.
- 3. Sazawal S, Black RE. Meta-analysis of intervention trials on case-management of pneumonia in community settings. Lancet 1992; 340: 528-533.
- 4. World Health Organization. Integrated management of the sick child. Bull World Health Organ 1995; 73: 735-740.
- 5. World Health Organization, Department of Child and Adolescent Health and Development. IMCI Adaptation Guide. Geneva: WHO/UNICEF; 2001. Available at: http://www.who.int/child-adolescent-health/New_Publications/IMCI/IMCI_Adaptation_Guide/IMCI_Adaptation_Guide.htm (accessed 8 Nov 2002).
- 6. Pretty JN, Gujit I, Scoones I, Thompson J. A trainer's guide for participatory learning and action. London: International Institute for Environment and Development, 1995.
- 7. Werner D, Bower W. Helping health workers learn. Berkeley, Calif: Hesperian Foundation, 1995.
- 8. INTRAH, PRIME II Project and JHPIEGO. Transfer of learning, a guide for strengthening the performance of health care workers. Chapel Hill, NC: University of North Carolina, 2002. Available at: http://www.intrah.org/tol (accessed 8 Nov 2002).
- 9. Sullivan RS. The competency-based approach to training. Baltimore, Md: JHPIEGO, 1995. Available at: http://www.reproline.jhu.edu/english/6read/6training/cbt/sp601web.pdf (accessed 8 Nov 2002).
- 10. Chambers R. Participatory workshops: a sourcebook of 21 sets of ideas and activities. London: Earthscan, 2002.
- 11. World Health Organization, Department of Child and Adolescent Health and Development. IMCI Planning Guide. Geneva: WHO/UNICEF, 1999. Available at: http://www.who.int/child-adolescent-health/New_Publications/IMCI/IMCI_Planning_Guide/IMCI_PlanningGuide1.pdf (accessed 8 Nov 2002).
- 12. AusAID, Papua New Guinea National Department of Health. Papua New Guinea women's and children's health project. 1998–2003. Canberra: AusAID (Final report not yet available).
- 13. Robinson SJ, Burkhalter BR, Rasmussen B, Sugiono R. Low-cost on-the-job peer training of nurses improved immunization coverage in Indonesia. Bull World Health Organ 2001; 79: 150-158.
- 14. Tibet primary health care and water supply project, a China-Australia development cooperation project. Project Completion Workshop. Canberra: AusAID, 2000.







Abstract
Training and education of health workers remains an indispensable part of good health development in resource-poor settings.
Many past training programs have failed to achieve significant gains in health outcomes because of poor selection of participants, inadequate methodology, and/or the influence of external factors in the health system or social environment.
The solutions lie in better planning of "who" and "what" should be trained; effective methods based on adult learning principles; alternative methods that maximise learner input and locate training as close as possible to the workplace and its problems; appropriate inclusion of the community; and coordination with other health system interventions.