Many Australians have limited knowledge and inaccurate beliefs about depression, and stigma often attaches to people who have suffered from depression.1 These factors have important consequences for prevention, early intervention, and treatment of depression; they can lead to delays in help-seeking, hinder acceptance of evidence-based mental healthcare, and mean that depressed people do not receive appropriate support from others in the community. Furthermore, preventive programs for depression are only possible where there is community support for action.
One aim of beyondblue: the national depression initiative is to promote community awareness and understanding of depression, which we refer to here as "depression literacy". In this article, we examine how this aim is best achieved, using evidence from depression literacy campaigns in other countries and principles derived from health promotion campaigns in other areas of healthcare.
Australia is not the first country to attempt to improve depression literacy. Internationally, four campaigns have been conducted and reported in the peer-review literature. The Defeat Depression Campaign was conducted across the United Kingdom from 1992 to 1996.2,3 Also in the UK, the Changing Minds Campaign, which aims to reduce stigma associated with mental health problems, began in 1998 and finishes in 2003.4 In the United States, the National Institute of Mental Health Depression Awareness, Recognition and Treatment Program, established in 1988, supports various community-based depression initiatives.5 Since 1990, the US National Depression Screening Day has been conducted annually.6 These initiatives are summarised in Box 1.
There is limited information from these campaigns to assist in developing an effective Australian depression literacy campaign, as these programs have not been fully evaluated. Only the Defeat Depression Campaign has been evaluated to assess whether it resulted in desired changes in the community's understanding of depression, its causes and treatments: 3 improvements of less than 10% were reported in the public's awareness of depression as a medical condition and the value of antidepressant drugs as suitable treatment for depression; 75% of people surveyed still saw medication as inappropriate. The effectiveness of community education components of the other initiatives remains unknown.
Although there is limited evidence on how to improve depression literacy, there is extensive experience in health promotion in other areas, such as heart disease and asthma. A strategy widely used to plan health promotion campaigns is the PRECEDE model.7 This model provides a framework for systematically addressing factors that affect health-related behaviours. The model's creators argue that development of effective health promotion initiatives around a particular health problem needs to deal sequentially with questions of:
whether individuals perceive desired health actions as affecting their quality of life, and, if so, how;
how behavioural, lifestyle and environmental factors contribute to choices to adopt those health actions;
how various predisposing, enabling, and reinforcing factors affect those behaviours, lifestyles and environments; and
how health education initiatives take account of and adjust predisposing, reinforcing and enabling factors to encourage individuals to take up desired health actions.7
Health policy initiatives may also be needed to improve factors that enable individuals to adopt such changes.7
The PRECEDE model as applied to improving depression literacy is illustrated in Box 2. Although the diagram's causal flow is left to right, health promotion planning goes from right (with the health promotion program goals) to left (with educational strategies and policy changes needed to achieve this).
The next step is to specify the personal behaviours (and behaviours of significant others) that can affect these outcomes. Reviewing relevant publications, we have found evidence that the following personal behaviours are related to better outcomes.
Changing modifiable risk factors. Most risk factors for depression are not readily modifiable by the individual. However, prolonged anxiety is a major risk factor for depression.8 This can be reduced by cognitive-behavioural techniques.9
Help-seeking. There is evidence that delayed help-seeking leads to persistence of depression,10 and that lack of treatment increases risk of recurrence.11
Presenting symptoms as depression-related. GPs are more likely to recognise depression if the patient self-labels as depressed and consults specifically for psychological symptoms.12,13 Although GP recognition of depression alone may not improve patient outcomes,14 it is necessary for effective medical intervention action.
Adherence to treatment. Patients adhering to prescribed treatments tend to have better outcomes.15
Using effective self-help. Self-help treatments are commonly used for depression,16 but only some have empirical support as effective.17
Further, behaviours of significant others may be helpful (eg, if the family is supportive and not critical, this can assist recovery and reduce risk of relapse).18 Depressed people are more likely to seek help if relatives or friends suggest it.1
In the PRECEDE framework, health education is not targeted at the behaviours leading to better outcomes, but at the factors that predispose to, reinforce and enable these behaviours.
Predisposing factors include knowledge, beliefs and attitudes relating to the motivation to act. Relevant factors for depression are:
Knowledge of depression symptoms. If depressed people are to correctly self-label and present to GPs as depressed, they need knowledge of depressive symptoms. Many people in the community cannot correctly recognise depression.1,19
Knowledge of modifiable risk factors. People need knowledge of risk factors to modify their personal risk. The Australian public believes that the social environment contributes to depression.1 Knowledge of the association of prolonged anxiety with depression has not been assessed.
Belief in professional help-seeking. Forty per cent of people with a depressive disorder do not seek professional help.20 To seek help, they must believe that seeking help is useful, and know a source of help. Many Australians cannot name a source of help they would use if they developed depression.1,19
Knowledge and attitudes towards healthcare professionals and depression treatments. To get effective help, the public must believe that healthcare professionals can help with depression, and that their treatments are effective. The Australian public has favourable attitudes towards GPs treating depression, but rates psychiatrists and psychologists less highly.1 Many members of the public have negative attitudes towards antidepressants, while viewing psychological treatments more positively.1,19 There is evidence that people are more likely to use and adhere to depression treatments that they believe are helpful.16,21
Knowledge of and attitudes to effective self-help. Self-help requires knowledge of which actions are likely to be effective. When Australians were asked to rate various interventions for likely helpfulness for depression, self-help interventions rated highest.1,19 However, evidence indicates that only some of these interventions (eg, exercise) are effective.17
Reinforcing factors determine whether the person receives positive (or negative) feedback and social support for their action. Important reinforcing factors for action on depression are:
Societal attitudes to depression. People may be reluctant to take action because they believe they will be stigmatised. These beliefs can affect the willingness of depressed people to seek help,22 and their treatment adherence.23
Significant others' knowledge and attitudes to help-seeking and treatments. Family and friends' willingness to encourage help-seeking will be limited by their own knowledge and attitudes towards professional help and treatments available.1
Enabling factors are the environmental conditions that facilitate performance of an action. Relevant factors for depression are:
Availability of information. Promotion of depression literacy requires the availability of high quality information. Although considerable information is available, its accessibility and quality may be limited, as recently shown with depression websites.24
Availability of effective interventions. Encouraging depressed people to seek help and use effective treatments is only worthwhile if the treatments are available and affordable. Some treatments (eg, psychological therapies) are not always available from the healthcare system or are too expensive.25
We have argued that previous depression literacy initiatives provide limited information on effective education strategies. Theoretical models can provide guidance on how people change their health attitudes and behaviours. Many of these models have not been applied in mental health, but can be extrapolated to depression literacy. Relevant models are summarised in Box 3. From these models and related research, we can derive the following strategies.
People differ in their readiness to change, and messages must vary to allow for this. Those ready to act (eg, seek help) need specific messages about what they can do, whereas those not ready to act need to become aware of the issue's importance.26
For people not ready to act, "experiential" approaches to encouraging change are best. These might include providing information about the high prevalence and disease burden of depression, and describing the benefits of taking action.26
People ready to act require "behavioural" approaches. These might include information on help-seeking pathways or teaching effective self-help approaches.26
People who are depressed are more likely to act if they see their symptoms as posing a threat, and have strategies to reduce that threat. For example, messages could emphasise disability caused by depression, possibility of suicide, and increased risk to physical health. Behaviours such as help-seeking and treatment compliance should be presented in a way that makes clear how they can reduce these threats.27
Action is more likely if its perceived costs are small. (People interpret "costs" to include factors such as perceived stigma and treatment side effects, as well as financial costs.) Messages can aim to reduce these perceptions of costs (eg, perceptions that antidepressant medication is addictive).27
Depression information is more likely to produce long term change in attitudes if it induces people to relate the information to other knowledge they have and to their past experiences.28 For example, an advertisement might ask the listener to think of someone they know who has experienced depression, and what they did to help. It could then present some simple action that could help in the future. This would be more effective than presenting the action without relating it to the audience's personal experience.
Communications about depression that rely primarily on associations with people who are seen as famous or attractive are less likely to produce long term change in attitudes.28 However, such communication may be useful where the target audience has little interest in, or previous knowledge of, depression.
Messages about depression treatments should appeal to various belief systems about treatment: medical, psychological, and lifestyle.29 Messages focusing solely on the helpfulness of medication, for example, may be ignored by people with strong lifestyle belief systems.
Depression information is more likely to be effective if it is tailored to the unique interests and needs of particular individuals.30 Information for middle-aged businessmen (themselves at low risk) might focus on the impact on their employees and lost productivity, or risks to family members.
Stigma can be tackled through various strategies, including education, social protest (ie, suppression of negative attitudes and behaviours towards depression) and promoting contact with people who have experienced depression. Contact appears to be the most effective.31 Education may have only a limited effect because stereotypes are resistant to change. With social protest, there is a danger of a rebound effect.
The effect of contact is maximised when participants have equal status, there is frequent contact with people who mildly disconfirm stereotypes, and there are real-world opportunities to interact, rather than contrived situations.31 A public meeting involving a person talking about his or her experience of depression is more likely to have a positive effect if it is sponsored by a well-regarded organisation and the person is not so exceptional as to be seen as atypical of people who have experienced depression.
According to the PRECEDE model, policy changes must support efforts to improve depression literacy. Much has already been achieved in Australia in this regard. The National Action Plan for Depression includes as objectives the raising of depression literacy and the reduction of stigma and discrimination.32
The Commonwealth, State and Territory governments have supported the implementation of the action plan by establishing beyondblue. To ensure that progress is realised, the effectiveness of initiatives developed through this action plan need to be evaluated thoroughly, although the non-laboratory setting of health-promotion programs can make such evaluations difficult.
The establishment of beyondblue has given the opportunity to make major gains in Australians' depression literacy, and we need to use this opportunity well. The principles derived from other areas of health promotion should provide a more rational basis for action than existed previously. However, these principles have not been specifically evaluated for depression literacy and require rigorous testing, for both short term effects on knowledge and attitudes, and longer-term effects on health behaviours and depression outcomes. Any gains in depression literacy would be expected to produce benefits for prevention, early intervention, treatment, and family support for people with depression.
1: Previous campaigns to improve depression literacy
Name |
Where |
When |
Community-based goals |
Main strategies for achieving community change |
Changes achieved |
||||||
Defeat Depression Campaign2,3 |
UK |
1992–1996 |
Reduce stigma, improve recognition and management of depression |
Public education through various media; Defeat Depression Action Week |
Improvements in attitudes of between 5% and 10% |
||||||
Changing Minds Campaign4 |
UK |
1998–2003 |
Reduce stigma, improve understanding of depression |
Public education through Web; collaboration with key groups |
Not evaluated to date |
||||||
Depression, Awareness, Recognition and Treatment Campaign5 |
US |
1988, ongoing |
Increase acceptance and knowledge of depression symptoms and treatment |
Public education through written and electronic media |
Not evaluated to date |
||||||
National Depression Screening Day6 |
US |
1991, ongoing |
Encourage screening for depressive disorder |
Public education through written and electronic media |
Partly evaluated, but changes in attitudes not assessed |
||||||
2: Application of the PRECEDE model of health promotion planning to depression literacy
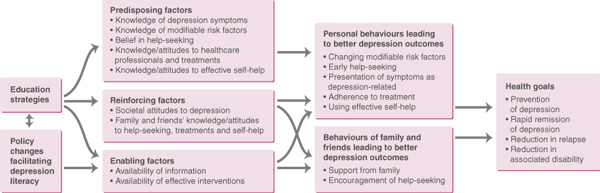
The causal flow is from left to right, but planning starts at the right and works left.
3: Models of attitude and behavioural change which can be applied to improving depression literacy
Name |
First published |
Description |
|||||||||
Health Beliefs Model27 |
1974 |
Individuals' readiness to take action to avoid disease requires recognition of susceptibility, potential severity, benefits of action. |
|||||||||
Elaboration Likelihood Model28 |
1986 |
Persuasion by central route (ie, careful consideration of issue), or peripheral route (influenced by peripheral cues [eg, attractiveness of presenter]). Central route produces more lasting attitude change. |
|||||||||
Transtheoretical Model/Stages of Change26 |
1983 |
Five stages of change: precontemplation, contemplation, preparation, action, and maintenance. Different types of interventions needed for individuals at each stage of change. |
|||||||||
- Ruth A Parslow1
- Anthony F Jorm2
- Centre for Mental Health Research, Australian National University, Canberra, ACT.
- 1. Jorm AF, Korten AE, Jacomb PA, et al. "Mental health literacy": a survey of the public's ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust 1997; 166: 182-186.
- 2. Paykel ES, Priest RG. Recognition and management of depression in general practice: consensus statement. BMJ 1992; 305: 1198-1202.
- 3. Paykel ES, Hart D, Priest RG. Changes in public attitudes to depression during the Defeat Depression Campaign. Br J Psychiatry 1998; 173: 519-522.
- 4. Crisp AH, Gelder MG, Rix S, et al. Stigmatisation of people with mental illnesses. Br J Psychiatry 2000; 177: 4-7.
- 5. Regier DA, Hirschfield RMA, Goodwin FK, et al. The NIMH Depression Awareness, Recognition, and Treatment Program: structure, aims and scientific basis. Am J Psychiatry 1988; 145: 1351-1357.
- 6. Jacobs DG. National Depression Screening Day: educating the public, reaching those in need of treatment, and broadening professional understanding. Harv Rev Psychiatry 1995; 3: 156-159.
- 7. Green LW, Kreuter MW. Health promotion planning. An educational and ecological approach. 3rd ed. Mountain View: Mayfield Publishing Company, 1999.
- 8. Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annu Rev Psychol 1998; 49: 377-412.
- 9. Nathan PE, Gorman JM. A guide to treatments that work. New York: Oxford University Press, 1998.
- 10. Scott J, Eccleston D, Boys R. Can we predict the persistence of depression? Br J Psychiatry 1992; 161: 633-637.
- 11. Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 1992; 149: 999-1010.
- 12. Bowers J, Jorm AF, Henderson S, Harris P. General practitioners' detection of depression and dementia in elderly patients. Med J Aust 1990; 153: 192-196.
- 13. Hickie IB, Davenport TA, Scott EM, et al. Unmet need for recognition of common mental disorders in Australian general practice. Med J Aust 2001; 175 Suppl Jul 16: S18-S24.
- 14. Simon GE, Goldberg D, Tiemens BG, Ustun TB. Outcomes of recognized and unrecognized depression in an international primary care study. Gen Hosp Psychiatry 1999; 21: 97-105.
- 15. Melfi CA, Chawla AJ, Croghan TW, et al. The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Arch Gen Psychiatry 1998; 55: 1128-1132.
- 16. Jorm AF, Christensen H, Medway J, et al. Public belief systems about the helpfulness of interventions for depression: associations with history of depression and professional help-seeking. Soc Psychiatry Psychiatr Epidemiol 2000; 35: 211-219.
- 17. Jorm AF, Christensen H, Griffiths KM, Rodgers B. Effectiveness of complementary and self-help treatments for depression. Med J Aust 2002; 176 Suppl May 20: S84-S86. <eMJA full text>
- 18. Hooley JM, Teasdale JD. Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. J Abnorm Psychol 1989; 98: 229-235.
- 19. Highet NJ, Hickie IB, Davenport TA. Monitoring awareness of and attitudes to depression in Australia. Med J Aust 2002; 176 Suppl May 20: S63-S68. <eMJA full text>
- 20. Parslow RA, Jorm AF. Who uses mental health services in Australia? An analysis of data from the National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2000; 34: 997-1008.
- 21. Churchill R, Khaira M, Gretton V, et al. Treating depression in general practice: factors affecting patients' treatment preferences. Br J Gen Pract 2000; 50: 905-906.
- 22. Sims A. The scar that is more than skin deep: the stigma of depression. Br J Gen Pract 1993; 43: 30-31.
- 23. Sirey JA, Bruce ML, Alexopoulos GS, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry 2001; 158: 479-481.
- 24. Griffiths KM, Christensen H. Quality of web based information on treatment of depression: cross sectional survey. BMJ 2000; 321: 1511-1515.
- 25. Andrews G, Issakidis C, Carter G. Shortfall in mental health service utilisation. Br J Psychiatry 2001; 179: 417-425.
- 26. Velicer WF, Prochaska JO, Fava JL, et al. Smoking cessation and stress management: application of the transtheoretical model of behavior change. Homeostasis 1998; 38: 216-233.
- 27. Becker MH. The Health Belief Model and Personal Health Behaviours. Thorofare, NJ: Charles B Slack Inc, 1974.
- 28. Petty RE, Cacioppo JT, Strathman AJ, Priester JR. To think or not to think: exploring two routes to persuasion. In: Shavitt S, Brock TC, editors. Persuasion. Psychological insights and perspectives. Boston: Allyn and Bacon, 1994.
- 29. Jorm AF, Korten AE, Rodgers B, et al. Belief systems of the general public concerning the appropriate treatments for mental disorders. Soc Psychiatry Psychiatr Epidemiol 1997; 32: 468-473.
- 30. Sorensen G, Emmons K, Hunt MK, Johnston D. Implications of the results of community intervention trials. Annu Rev Public Health 1998; 19: 379-416.
- 31. Corrigan PW, River LP, Lundin RK, et al. Three strategies for changing attributions about severe mental illness. Schizophr Bull 2001; 27: 187-195.
- 32. Commonwealth Department of Health and Aged Care. National Action Plan for Depression. Canberra: Mental Health and Special Programs Branch, 2001.





Abstract
Community awareness and understanding of depression ("depression literacy") underpins successful implementation of prevention, early intervention and treatment programs. Improving depression literacy is a major goal of beyondblue: the national depression initiative.
Although other countries have previously attempted to address this issue, there is little evidence to indicate that those attempts have achieved their aims.
Work in other areas of health promotion, such as the widely used PRECEDE model, offers a useful framework from which to develop effective depression literacy initiatives in Australia. This model proposes that effective health promotion strategies should focus not on health actions per se, but on the knowledge and attitudes that encourage or impede individuals from taking such actions.
We identify the goals of an effective depression literacy campaign and a range of educational strategies for achieving change in each of these areas. Applying these strategies may give a stronger basis for improving depression literacy than previous initiatives.