Currently, there is an increased awareness of the use of chemical, biological and radiological agents, both in terrorist attacks and in daily industrial accidents. So far, Australia has lagged behind the United States and Israel in preparation for actual terrorist events.
Secondary contamination has forced the closure of at least three emergency departments recently (Dr Jane Canestra, Clinical Director, Emergency Department, Frankston Hospital, personal communication),1,2 posing a significant danger to staff and a loss of a community asset. For example, Ballarat Health Services had an incident where a patient was not decontaminated before being treated in the emergency department; this resulted in the closure of the emergency department for 20 hours.2 Having a chemical–biological–radiological (CBR) response ought to prevent such occurrences.
There is clearly a need for all healthcare facilities to develop a CBR response. Most healthcare facilities, both in Australia and in other countries, are not adequately prepared to manage mass CBR casualties.3,4 The Australasian College for Emergency Medicine also does not have guidelines for decontamination or CBR response.
For most hospital staff, chemical incidents present an obscure and even frightening situation.5 Most emergency departments are not prepared for the decontamination of toxic substances, and do not have a decontamination facility, have an inappropriately placed one,6 or have a rudimentary one which would quickly be overwhelmed in the event of mass casualties.4,7
In this article, we show how an emergency department in a tertiary referral centre implemented a CBR response. We also wish to heighten the awareness of CBR response among the medical community.
An emergency department is a protected area and the prevention of secondary contamination of staff and the department must be guaranteed. With activation of the External Disaster Plan, all entry and exit points should be secured and all movement through the emergency department and hospital must be regulated. Clear labelling of "contaminated" and "clean" areas is needed when a CBR response has been activated.
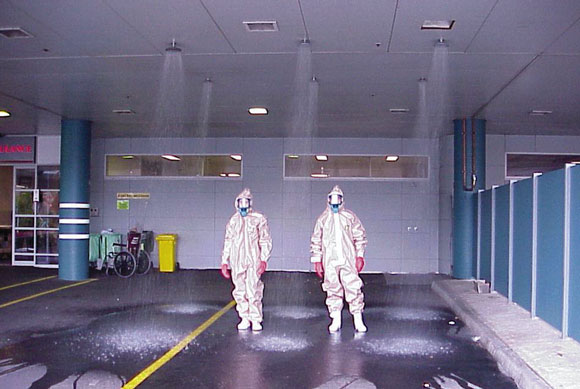
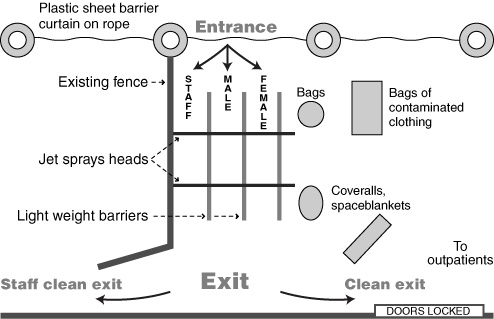
All patients presenting after a CBR incident require decontamination. In the ambulance bay outside our department, there is a cubicle with one shower head, which would be used in the event of a single or very small number of patients. A further three rows of two shower heads were installed in the ceiling of two of the four ambulance bays. These three lines allow mass casualties, as well as trolleys and equipment, to be decontaminated quickly, efficiently and in an orderly fashion (see Box 1 and Box 2).
For decontamination, all patients are required to shower initially with their clothes on, then remove their clothing, step forward to the next shower head and shower while gently cleansing with soap. They then move forward to dry themselves and put on a clean disposable suit within the "clean" zone. The principle is to move at all times towards the "clean" zone. Staff put the patients' belongings in clean bags, and these and the patients are labelled with identical numbers. The bags of belongings are then placed in the contaminated clothing bin.
All showers have temperature regulation to prevent hypothermia and provide patient comfort.
Having the shower heads in the ceiling of the ambulance bay allows decontamination to be carried out under cover. The ceiling is also fitted with a sprinkler system, which is isolated from the rest of the department and can be used if the showers prove inadequate.
Once patients are decontaminated, they are allowed into the hospital. Depending on their triage category, they will either go into the emergency department or via a clearly demarcated route to the outpatient department. A separate route was established for staff to go to their "base" area for rotation while on duty using their personal protective equipment.
The regulation of movement of ambulances through the area is very important to prevent congestion. Ambulances carrying patients will arrive through a one-way entrance, stop at the drop-off point, and move away in one direction, ensuring smooth traffic flow.
Our emergency department has a ventilation system that is isolated from the rest of the hospital. It also has two negative-pressure rooms, which are used for patients continuing to "offgas". The air in these rooms is replaced six times per minute, and vented directly into the atmosphere. When large numbers of patients are involved, they are treated outside.
In the event of an external disaster, the hospital would go on ambulance bypass and "walk in" patients would be incorporated into the External Disaster Plan.
Ordinary hospital gowns, goggles and latex gloves are inadequate for a CBR response, as they provide only minimal protection.8
Personal protective equipment (PPE), comprising plastic overalls, facemasks with filter, work boots and gloves, was obtained for staff protection (Box 3). No one PPE is adequate to protect staff from all agents.7 The PPE we selected is a non-encapsulating suit, butyl and nitrile gloves with a facemask and filter, and cost $500 a set. The PPEs conform to Australian standards, and protect the respiratory tract, face, eyes, body, hands and feet in a hospital environment where the chemical vapour concentration will not be high.12-11
Disposable coveralls, linen and portable screens were obtained for patient privacy and comfort during the decontamination process.
Plastic bags were obtained for contaminated patient clothing, as well as large containers for their storage. This is very important for forensic purposes and the preservation of evidence.
Plastic sheeting is also required for lining surfaces during a radiological event, and Geiger counters are available to test patients' radiation level after decontamination, before they enter the emergency department. The Radiation Safety Officer will be called in to help with the management of patients in a radiological incident.
Portable personnel barriers were organised for crowd control, which is an important aspect of a disaster response.
Extra medications were obtained for the emergency department and the hospital during periods of potential problems (eg, the World Economic Forum and the Olympics). The medications stockpiled at our hospital included atropine, pralidoxime, ciprofloxacin and doxycycline. This was considered justifiable because of their long half-life, use within the hospital and low cost. Because of the US experience in 1998 showing that large amounts of antibiotics can be taken inappropriately by the "worried well",12 our stockpiles are kept at a secure place and can only be released with authorisation from the Director of Infectious Diseases, Director of Emergency Services or Director of Pharmacy.
The total cost for the PPEs, showers and other equipment was less than $20 000.
The personnel required for the CBR response include medical, nursing, security, clerical, orderlies, patient care assistants and other staff, depending on the type of threat (eg, Radiation Safety Officer, Infectious Diseases Unit).
The actual composition of staff and numbers required need careful planning, as numerous shifts and rotations may be required for a prolonged response. The initial response requires a senior doctor, a senior nurse, a clerk and a security officer to be in the contaminated zone (wearing PPE). Later, more staff members, especially security staff, will be needed in PPEs in the contaminated zone.
There are numerous exclusion criteria as well as monitoring aspects that must be strictly adhered to for use of the PPEs.13 The exclusion criteria include upper respiratory tract infection, vomiting or diarrhoea within the previous 72 hours.13 We estimate that 20% of our staff would be excluded at any time. Subject to ambient temperature, individuals can spend about 30 minutes in the suit; a nurse is delegated to monitor early signs of heat illness (such as malaise, nausea, dizziness and headache) and ensure regular rotation of staff members. It is very important that a register of trained, available staff is organised and an on-call roster established.
An extensive education and training program was organised for all staff, with retraining initially after six months and then annually. A comprehensive manual with photos of every step involved in putting on and taking off the PPE was developed. It has been suggested that instruction of the hospital plan be carried out on a yearly basis for hospitals in areas of minimal threat.3
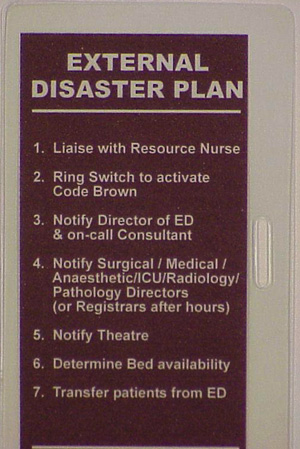
Credit-card-sized cards detailing the External Disaster Plan protocol were distributed to all staff and were attached to their identity badges to facilitate and heighten the awareness of the activation of the disaster plan (see Box 4). Posters of the CBR response protocol were also displayed in appropriate areas.
Practice scenarios were run involving all staff members. These exercises highlighted various logistical aspects of the CBR response that required modification. The only way to acquire such knowledge and experience is to conduct frequent and comprehensive practice drills.4,14
There was close liaison with the Infectious Diseases Unit during planning of the CBR response. A booklet and posters reviewing the common biological agents, their signs and symptoms, infectivity, level of isolation and treatment was produced, and is located in the emergency department.
The provision of a safe workplace is of the utmost importance. Given the nature of a CBR event, a specific planned response as part of the External Disaster Plan should be mandatory in all hospitals. Appropriate PPE should be available in all hospitals, and staff should be able to choose not to participate.
Failure to provide employees with adequate training and protective equipment can result in unnecessary exposures to toxins and violation of occupational health and safety regulations, and result in potential litigation.7,15,16
A surveillance system was implemented to record daily emergency department presentations of various diagnoses, with emphasis on respiratory symptoms, rashes and fever (Box 5). This is reviewed daily by the Director of Emergency Services, the Emergency Physician in Charge of External Disasters, and the Director of Infectious Diseases. Any deviation from the normal daily pattern would be noted and followed up immediately.
It is hoped that similar surveillance systems can be established in all emergency departments in Australia and the data transmitted on a daily basis to a surveillance coordination centre.17
Currently, there is a lack of understanding and preparation for a CBR incident among emergency departments in Australia, and in other countries.18 Even the simple event of a patient contaminated with capsicum spray requires rigorous decontamination to prevent prolonged secondary contamination of emergency departments.
Our recommendations are similar to systems in the US and Israel,3,7,17 but much less intensive, as the threat of a terrorist attack here is perceived to be much lower.
The concept that the emergency department and the hospital is a community asset that requires protection, and no patient is to be allowed within these areas until after decontamination, must be understood.13 Not surprisingly, unprotected staff members may rush to the aid of contaminated patients and become patients themselves — leading to an exacerbation of the problem.19,20 A well-understood response plan and adequate training should avoid this problem.
The belief that patients will arrive at emergency departments already decontaminated also needs to be challenged. Studies have shown that, in the event of a disaster situation, most patients will present to the local hospital by private transport.21,22 Hence, it is very important that all hospitals have an adequate decontamination facility that can quickly and efficiently decontaminate stretcher patients as well as mass casualties.
Hospitals should have a CBR response set out as part of their External Disaster Plan, and should have appropriate PPE. Failure to do so could lead to legal challenges for not providing a safe workplace if a staff member becomes secondarily contaminated.
4: Card summarising the External Disaster Plan protocol, distributed to all staff to be attached to identity badges
5: Diagnoses included in the daily biohazard census
ICD-10 code |
Description |
J00 |
Cold, common |
J019 |
Sinusitis, acute, unspecified |
J020 |
Pharyngitis, acute streptoccal (including sore throat) |
J029 |
Pharyngitis |
J039 |
Tonsillitis, acute |
J040 |
Laryngitis |
J041 |
Tracheitis, acute |
J069 |
Upper respiratory tract infection, unspecified |
J111 |
Influenza, viral |
J22 |
Infection, lower respiratory tract/chest, acute |
J348 |
Nasal congestion, obstruction, discharge/rhinolith |
R05 |
Cough |
R091 |
Pleurisy |
L089 |
Skin infection |
L270 |
Rash, drug, generalised |
L271 |
Rash, drug, localised |
R21 |
Rash, non-vesicular |
R509 |
Fever/pyrexia of unknown origin |
- Gim A Tan1
- Mark C B Fitzgerald2
- Emergency and Trauma Centre, The Alfred Hospital, Melbourne, VIC.
None identified
- 1. Nocera A, Levitin H, Hilton J. Dangerous bodies: a case of fatal aluminium phosphide poisoning. Med J Aust 2000; 173: 133-135.
- 2. Dangerous chemicals force ward closures. The Ballarat Courier 2000; 25 September: 3-4.
- 3. Tur-Kappa I, Lev E, Hendler I, et al. Preparing hospitals for toxicological mass casualties events. Crit Care Med 1999; 27: 1004-1008.
- 4. Totenhofer RI, Kierce M. It's a disaster: Emergency departments' preparation for a chemical incident or disaster. Accid Emerg Nurs 1999; 7: 141-147.
- 5. Mukerjee M. Toxins abounding. Sci Am 1995; 272: 15-16.
- 6. Rodgers J. A chemical gas incident in London: how well prepared are London A&E departments to deal effectively with such an event? Accid Emerg Nurs 1998; 6: 82-86.
- 7. Cox R. Decontamination and management of hazardous materials exposure victims in the emergency department. Ann Emerg Med 1994; 23: 761-770.
- 8. Wheeler H. Major incident planning, particularly those including chemicals. Emerg Nurs 1998; 6: 12-16.
- 9. Standards SAA HB9-1994. Occupational personal protection. 2nd ed. Sydney: Standards Australia, 1994.
- 10. Standard AS 3765.1-1990. Clothing for protection against hazardous chemicals. Part 1: Protection against general or specific chemicals. Sydney: Standards Australia, 1990.
- 11. Standard AS/NZS 1715: 1994. Selection, use and maintenance of respiratory protective devices. Sydney: Standards Australia, 1994.
- 12. Inglesby T, Henderson D, Bartlett J, et al. Anthrax as biological weapon. Medical and public health management. JAMA 1999; 281: 1735-1745.
- 13. Australian Emergency Manuals Series. Part 3: Emergency management practice. Volume 2: Specific issues. Manual 3: Health aspects of chemical, biological and radiological hazards. Canberra: Emergency Management Australia, 2000.
- 14. Waekerle J. Disaster planning and response. N Engl J Med 1991; 324: 815-821.
- 15. National Model Regulations for the Control of Workplace Hazardous Substances [NOHSC: 1005(1994)]. Canberra: National Occupational Health and Safety Commission, 1994. Available at <http://www.nohsc.gov.au/OHSInformation/NOHSCPublications/#3>.
- 16. National Code of Practice for the Control of Workplace Hazardous Substances [NOHSC: 2007(1994)]. Canberra: National Occupational Health and Safety Commission, 1994. Available at <http://www.nohsc.gov.au/OHSInformation/NOHSCPublications/#5>.
- 17. Sharp T, Brennan R, Keim M, et al. Medical preparedness for a terrorist incident involving chemical or biological agents during the 1996 Atlanta Olympic games. Ann Emerg Med 1998; 32: 214-223.
- 18. Rodgers J. Chemical incident planning: a review of the literature. Accid Emerg Nurs 1998; 6: 155-159.
- 19. Nozaki H, Hori S, Shinozawa Y, et al. Secondary exposure of medical staff to sarin vapour in the emergency room. Intensive Care Med 1995; 21: 1032-1035.
- 20. Okudera H, Morita H, Iwashita T, et al. Unexpected nerve gas exposure in the City of Matsumoto: report of rescue activity in the first sarin gas terrorism. Am J Emerg Med 1997; 15: 527-528.
- 21. Okumura T, Nobukatsu T, Ishimatsu S, et al. Report on 640 victims of the Tokyo subway sarin attack. Ann Emerg Med 1996; 28: 129-135.
- 22. Levitin H, Siegelson H. Hazardous materials. Disaster medical planning and response. Emerg Med Clin North Am 1996; 14: 327-348.






Abstract
Chemical, biological and radiological (CBR) incidents have the potential to shut down emergency departments that do not have an adequate CBR response. Secondary contamination also poses a threat to the safety and wellbeing of staff and other patients.
On activation of a CBR response, "clean" and "contaminated" areas should be clearly marked, and all patients decontaminated before being allowed into the emergency department or outpatients department.
Personal protective equipment (PPE) is needed for all staff. Staff using PPE must be monitored for signs of heat illness.
Stocks of coveralls, bags for contaminated clothes, plastic sheeting for radiological incidents, barriers for crowd control, and selected drugs should be obtained.
Staff required include medical, nursing, security, clerical, orderlies, patient care assistants and other staff, depending on the type of threat. An on-call roster that allows regular rotation of staff is needed.
All hospital personnel should understand the response plan, and recognise that the emergency department and hospital is a community asset that requires protection.