Stroke is the third-greatest single cause of death in Australia, after ischaemic heart disease and cancer.1 Each year, more than 40 000 Australians suffer a stroke;2 a third of these people will die within a year,3,4 and half will be disabled.5 The incidence of stroke increases with age, approximately doubling with each decade of life.4 Given the ageing of the Australian population, the number of strokes occurring is likely to dramatically increase unless stroke incidence can be reduced.
Substantial advances in acute stroke management have occurred in recent years, including the use of aspirin, increased access to stroke units and, for selected patients, thrombolysis with tissue plasminogen activator.6 However, the most effective method of reducing the burden of stroke is prevention.7,8 There are two approaches to prevention: the "high-risk" approach, in which individuals with high absolute risk of stroke are identified and interventions initiated, and the "population" approach, in which levels of risk factors are reduced in the population.
Important risk factors for stroke are increasing age, hypertension, smoking, diabetes, hypercholesterolaemia, atrial fibrillation and prior stroke or transient ischaemic attack (TIA). Other factors include family history, male sex, excessive alcohol intake, prothrombotic factors, socioeconomic status and possibly physical inactivity, obesity, infection and stress.9 The prevalence of these risk factors in a typical general practice population is unknown. Our study was primarily designed to obtain this information, to facilitate both the high-risk and population approaches to stroke prevention.
Our aims were to assess among patients consulting general practitioners in Australia (1) the prevalence of important stroke risk factors, and (2) the type and extent of use of pharmacotherapies to modify risk factors.
We conducted a multicentre, observational study of patients attending general practices in Australia.
The study was undertaken during 2000 in Queensland, New South Wales, South Australia, Victoria, Tasmania and the Australian Capital Territory. Western Australia and the Northern Territory were not included for logistical reasons (GPs from WA had participated in an earlier feasibility study). All registered GPs (18 066) were sent a letter seeking expression of interest in the study. Of these, 1850 replied and were eligible for participation. The study area was divided into 22 regions, each serviced by about 600 GPs. From each region, 18 doctors were randomly selected from the 1850 eligible (396 in total). If a doctor was unavailable or refused participation, the geographically closest GP was approached. This process ensured that rural and urban practices and a representative range of socioeconomic settings were included.
Each GP approached 50 consecutive patients aged 30 years or older to participate in the study. Demographic data only were recorded on patients who refused consent.
Management of patients with risk factors was left to the GPs' discretion.
Risk-factor and demographic information was obtained through a four-page questionnaire. The GPs completed the questionnaires for participating patients during the standard consultation for which the patient had attended the clinic.
Hypertension was defined as a past history of hypertension or a current presentation with blood pressure ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic. Each patient's most recent blood pressure measurement was recorded. Hypercholesterolaemia was defined as a past history or current presentation with a total fasting cholesterol level ≥ 5.5 mmol/L. Diabetes was defined as a past history or a current presentation with a fasting blood glucose level ≥ 7.0 mmol/L. Atrial fibrillation was defined as a past history or a current presentation with atrial fibrillation confirmed on electrocardiography.
Current smoking status and history of stroke or TIA within the past 12 months was also recorded.
The classes of medications taken to treat specific risk factors were recorded. For patients taking cardiovascular agents, the GP was asked to specify whether hypertension, congestive cardiac failure or ischaemic heart disease was being treated.
Data were entered into SPSS10 for analysis. Proportions of patients with risk factors and receiving medications were calculated. Differences in age and sex distribution between participating and non-participating patients were examined using Student's t test and χ2 analysis, respectively.
The Quality Assurance Unit of the Royal Australian College of General Practitioners approved the study. Participation earned Clinical Audit and Continuing Medical Education points. Informed consent was obtained from each patient before the interview was conducted.
Of the 396 GPs included in the study, 321 (81%) returned data on 50 patients. Of these, 120 doctors were practising in NSW, 92 in Victoria, 59 in Queensland, 27 in SA, 18 in Tasmania and 5 in the ACT. Two hundred and thirty-one GPs were from metropolitan and 90 from rural areas. Twelve doctors provided data on some patients but did not complete the study.
Overall, 16 148 patients were approached. Of these, 1398 (9%) refused participation or their doctor withdrew them. Thus, 14 750 patients (91%) were included. Some data on individual risk factors or medication use were missing; the tables include the number of patients for whom data were available.
Box 1 summarises the age and sex distribution of patients approached for the study. The mean age of male patients was 58 years (range, 30–99 years) and of female patients 57 years (range, 30–99 years). Patients of both sexes were evenly distributed across age groups. There was no significant difference in age between patients included in the study and those who refused to participate (mean, 57.2 v 56.5 years; P = 0.13); however, there was a higher proportion of men in the participating group (P < 0.001).
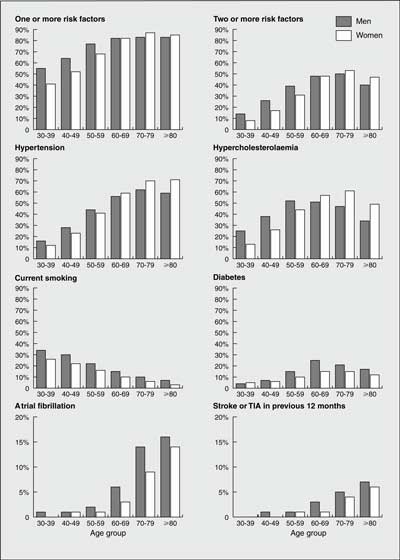
Seventy per cent of patients (74% of men; 67% of women) had one or more risk factors and 34% (37% of men; 33% of women) had two or more. Overall prevalence of risk factors increased with age. The prevalence of individual risk factors is given in Box 2 and the prevalence by age groups in Box 3. Hypertension and hypercholesterolaemia were most common. Within the past 12 months, 2% of patients had suffered a stroke or TIA; however, 3% had any history of stroke and 4% had any history of TIA.
Medication use for treating stroke risk factors is summarised in Box 4. Cardiovascular therapies (defined as treatment for hypertension, cardiac failure or ischaemic heart disease) were most common, followed by antiplatelet agents and lipid-lowering agents. Men had slightly higher rates of use for all classes of medication.
Cardiovascular medication use for patients with hypertension, cardiac failure and ischaemic heart disease is shown in Box 5. Overall, 67% of patients with hypertension were being treated with antihypertensive medication. Of these, 70% had blood pressure recordings above the range recommended in published guidelines (40% had mild hypertension, 22% had moderate hypertension, and 8% had severe hypertension).12 Five per cent of patients had a history of heart failure and, of these, 73% were taking cardiovascular agents, most commonly diuretics. Eleven per cent of subjects had a history of ischaemic heart disease and, of these, 48% were receiving treatment, most with β-blockers or calcium-channel blockers. The pattern of cardiovascular medication use was similar for men and women.
Our study has yielded unique data on the prevalence of stroke risk factors in an Australian general practice population. The data were obtained from general practices that were spread throughout Australia, including metropolitan and rural communities and a range of socioeconomic settings. Thus, the information obtained is likely to be representative of most Australian general practice environments.
Nevertheless, there is likely to be selection bias in the study. Ethnic origin of patients was not recorded; therefore, we cannot be sure our sample is representative of all ethnic groups. As no doctors were from the Northern Territory, people of Aboriginal populations are found in capital cities covered by the study. The age and sex structure of the general population differs from that of the sample. Whether the high proportion of women in the study is due to women being more likely to attend GPs or to chance is uncertain. Of patients aged over 80 years, 10% were taking warfarin, a higher rate than would be expected in the general population. Our definition of hypertension as a past history or a single recording of greater than 140/90 mmHg may include patients who do not have persistent hypertension. This may partly explain why the prevalence of hypertension in our study is higher than in a previous Australian survey13 (although the previous sample consisted of people between 20 and 69 years of age, therefore excluding the age groups with the highest rates of hypertension). The prevalence of hypertension in our study is similar to other published figures.14 The prevalences of hypercholesterolaemia,13 atrial fibrillation,15 diabetes16 and smoking13 are similar to those previously reported.
About 86% of adults in Australia consult a GP at least once a year (Carolynn Fredericks, Department of Health and Ageing, personal communication). Therefore, GPs can play an important role in stroke prevention by opportunistic case-finding of patients with stroke risk factors. The National Health and Medical Research Committee (NHMRC) guidelines on stroke prevention recommend routine screening of all patients over 45 years of age and younger patients who have risk factors.17 This can be achieved at little additional cost to the community if conducted during routine consultations. Systematic screening for risk factors during routine consultations would enable identification of patients at high risk of stroke, particularly those with multiple risk factors. Of course, people who do not attend general practices may have different prevalence of risk factors than those who do, and will not benefit from case-finding by GPs.
Most of the stroke risk factors increased in prevalence with age. Hypercholesterolaemia and diabetes were more common with increasing age, but less prevalent in the oldest age groups. Age is an independent risk factor for stroke9 and this, together with the risk-factor prevalence profiles, explains the exponential increase in stroke risk with age. Importantly, hypertension, hypercholesterolaemia and smoking had a prevalence of more than 10% in men and women aged 30–39 years. This suggests that screening for risk factors in any patient aged over 30 years is worthwhile, so that risk-factor modification may begin before the onset of symptomatic atherosclerosis. In contrast, atrial fibrillation had a very low prevalence below the age of 60 years and it is older patients who require screening for this.
Some of our results are perplexing, such as 10% of patients receiving diuretics for treatment of ischaemic heart disease. Lower proportions of women were receiving each type of pharmacotherapy than men. Although intriguing, reasons for this were not addressed in the study. Surprisingly, TIA had a higher prevalence than stroke. Possible explanations include chance, post-stroke dependency, or misclassification (TIA is difficult to differentiate from minor stroke or non-vascular causes).
The high prevalence of stroke risk factors suggests that many patients could benefit from interventions to prevent stroke. Antihypertensive agents for hypertension,18 antiplatelet agents in people with prior stroke or TIA,19 warfarin for atrial fibrillation20 and the use of statins for hypercholesterolaemia in patients with evidence of coronary artery disease21 are effective in reducing stroke incidence. The evidence in observational studies for the reduction of stroke incidence with cessation of smoking is overwhelming.22 Hypertension may be modified by reducing salt intake,23 and obesity9 and lack of physical exercise9 have been associated with increased risk of stroke. However, whether lifestyle advice delivered by GPs is effective in reducing stroke risk is unproven.
Medical diagnosis and intervention does not necessarily imply adequate control of stroke risk factors. Of patients receiving medications for hypertension, 30% had blood pressures recorded in the moderate to severely hypertensive range. Stroke is associated with undertreated hypertension,24 so ongoing medical supervision is required to ensure therapy is adequate.
Substantial numbers of patients in our study with a history of hypertension, cardiac failure and ischaemic heart disease were not receiving cardiovascular medication. Although reasons for non-treatment (such as contraindication, poor compliance, or stable disease) were not addressed, it is likely that some of these patients are being denied potentially beneficial therapy.
Overall, our study offers unique Australian data on the prevalence of stroke risk factors in a population highly relevant to GPs. The high prevalence of stroke risk factors in patients attending Australian general practice clinics suggests that GPs are ideally placed to undertake opportunistic risk-factor management. The Avoid Stroke as Soon as Possible (ASAP) audit provides baseline data against which progress in risk factor management can be measured.
1: Age and sex distribution of participants and non-participants
|
Participants |
Non-participants |
Australian population11 |
||||||||
Age group (years) |
|||||||||||
30–39 |
2 197 (15%) |
258 (19%) |
26% |
||||||||
40–49 |
2 792 (19%) |
264 (20%) |
25% |
||||||||
50–59 |
3 036 (21%) |
234 (18%) |
20% |
||||||||
60–69 |
2 699 (19%) |
203 (15%) |
13% |
||||||||
70–79 |
2 717 (19%) |
231 (17%) |
10% |
||||||||
≥ 80 |
1 086 (7%) |
144 (11%) |
5% |
||||||||
Not specified |
223 |
64 |
|||||||||
Total |
14 750 (100%) |
1398 (100%) |
100% |
||||||||
Sex |
|||||||||||
Male |
5 989 (41%) |
491 (36%) |
49% |
||||||||
Female |
8 646 (59%) |
877 (64%) |
50% |
||||||||
Not specified |
115 |
30 |
|||||||||
Total |
14 750 (100%) |
1398 (100%) |
100% |
||||||||
2: Stroke risk factor prevalence among patients aged 30 years and older consulting general practitioners*
Total |
Men |
Women |
|||||||||||||
n† |
Percentage with risk factor (95% CI) |
n† |
Percentage with risk factor (95% CI) |
n† |
Percentage with risk factor (95% CI) |
||||||||||
Hypertension |
14 280 |
44% (43%–45%) |
5839 |
45% (43%–46%) |
8441 |
43% (42%–44%) |
|||||||||
Hypercholesterolaemia |
12 516 |
43% (42%–44%) |
5186 |
44% (43%–45%) |
7330 |
42% (41%–44%) |
|||||||||
Current smoking |
14 297 |
17% (16%–18%) |
5851 |
20% (19%–21%) |
8446 |
15% (14%–16%) |
|||||||||
Diabetes |
13 767 |
12% (12%–13%) |
5607 |
16% (15%–16%) |
8160 |
10% (10%–11%) |
|||||||||
Atrial fibrillation |
14 194 |
4% (4%–5%) |
5801 |
6% (5%–6%) |
8393 |
4% (3%–4%) |
|||||||||
Stroke/TIA‡ |
14 321 |
2% (2%–2%) |
5861 |
2% (2%–3%) |
8460 |
2% (1%–2%) |
|||||||||
* The totals exceed 100% because some patients had multiple risk factors. |
|||||||||||||||
3: Stroke risk factor prevalence, by age group and sex, in patients aged 30 years and older consulting general practitioners
4: Pharmacotherapy use, by age group, in patients aged 30 years and older consulting general practitioners
Age group (years) |
Cardiovascular agent† |
Oral hypoglycaemic agent |
|||||||||
n* |
% (95% CI) |
n* |
% (95% CI) |
||||||||
30–39 |
2 134 |
7% (6%–8%) |
2 182 |
1% (1%–1%) |
|||||||
40–49 |
2 730 |
17% (16%–19%) |
2 774 |
3% (2%–4%) |
|||||||
50–59 |
2 979 |
36% (34%–37%) |
3 018 |
6% (6%–7%) |
|||||||
60–69 |
2 647 |
56% (54%–58%) |
2 684 |
11% (10%–12%) |
|||||||
70–79 |
2 663 |
69% (67%–71%) |
2 699 |
10% (9%–12%) |
|||||||
≥ 80 |
1 067 |
76% (73%–78%) |
1 076 |
9% (7%–10%) |
|||||||
Total |
14 220 | 41% (40%–42%) | 14 433 | 7% (6%–7%) | |||||||
Antiplatelet agent ‡ |
Insulin |
||||||||||
30–39 |
2 182 |
1% (1%–2%) |
2 182 |
1% (0%–1%) |
|||||||
40–49 |
2 774 |
4% (4%–5%) |
2 774 |
1% (1%–1%) |
|||||||
50–59 |
3 018 |
12% (11%–13%) |
3 018 |
2% (1%–2%) |
|||||||
60–69 |
2 684 |
27% (25%–29%) |
2 684 |
3% (2%–4%) |
|||||||
70–79 |
2 699 |
42% (40%–43%) |
2 699 |
2% (2%–3%) |
|||||||
≥ 80 |
1 076 |
48% (45%–51%) |
1 076 |
1% (1%–2%) |
|||||||
Total |
14 433 | 20% (19%–21%) | 14 433 | 2% (2%–2%) | |||||||
Lipid-lowering agent † |
Anticoagulant (warfarin) † |
||||||||||
30–39 |
2 182 |
2% (1%–3%) |
2 182 |
0% (0%–1%) |
|||||||
40–49 |
2 773 |
8% (6%–9%) |
2 774 |
1% (1%–1%) |
|||||||
50–59 |
3 017 |
17% (16%–19%) |
3 018 |
2% (2%–3%) |
|||||||
60–69 |
2 684 |
30% (29%–32%) |
2 684 |
4% (4%–5%) |
|||||||
70–79 |
2 699 |
32% (31%–34%) |
2 699 |
8% (7%–9%) |
|||||||
≥ 80 |
1 076 |
20% (18%–23%) |
1 076 |
10% (8%–11%) |
|||||||
Total |
14 431 | 19% (18%–19%) | 14 433 | 4% (3%–4%) | |||||||
* Number for whom information was available. † Angiotensin-converting inhibitor, angiotensin II blocker, β-blocker, calcium-channel blocker, diuretic. ‡ Aspirin, clopidogrel, dipyridamole. |
|||||||||||
5: Distribution of pharmaceutical use in patients with cardiovascular disease
Percentage (95% CI) of patients treated for cardiovascular disease with each drug class |
|||||||||||||||
Hypertension |
Cardiac failure |
Ischaemic heart disease |
|||||||||||||
ACE inhibitor |
47% (45%–48%) |
53% (48%–57%) |
25% (21%–28%) |
||||||||||||
Angiotensin II blocker |
19% (18%–20%) |
8% (6%–10%) |
7% (5%–9%) |
||||||||||||
β-Blocker |
21% (20%–22%) |
12% (10%–15%) |
42% (38%–45%) |
||||||||||||
Calcium-channel blocker |
36% (35%–38%) |
9% (7%–12%) |
39% (36%–43%) |
||||||||||||
Diuretic |
29% (28%–31%) |
75% (71%–78%) |
10% (8%–13%) |
||||||||||||
Other |
5% (4%–5%) |
17% (14%–20%) |
28% (25%–31%) |
||||||||||||
ACE = Angiotensin-converting enzyme. |
|||||||||||||||
Received 25 June 2001, accepted 19 November 2001
- Jonathan W Sturm1
- Geoffrey A Donnan2
- Stephen M Davis3
- John G O'Sullivan4
- Miriam E Vedadhaghi5
- 1 National Stroke Research Institute and Department of Neurology, Austin and Repatriation Medical Centre, West Heidelberg, VIC.
- 2 Department of Medicine, Melbourne University, and Department of Neurology, Royal Melbourne Hospital, Melbourne, VIC.
- 3 Blackburn Clinic, Blackburn, VIC.
- 4 Servier Laboratories, Hawthorn, VIC.
Professor John Chalmers, Professor Stephen Davis, Professor Geoffrey Donnan, Associate Professor Graham Hankey, Professor Stephen MacMahon, Dr John O'Sullivan and Professor Paddy Phillips were members of the study management committee and were involved in the study concept and design. Covance Australia Pty Ltd provided assistance with data analysis.
Servier Laboratories supported this work financially, but had no influence over the analysis or interpretation of the study results, or the decision to submit the manuscript for publication.
- 1. Mathers C, Vos T, Stevenson C. The burden of disease and injury in Australia. Canberra: Australian Institute of Health and Welfare, 1999.
- 2. Stroke Australia Task Force. National Stroke Strategy. Melbourne: National Stroke Foundation, 1997.
- 3. Anderson CS, Jamrozik KD, Broadhurst RJ, et al. Predicting survival for 1 year among different subtypes of stroke. Results from the Perth Community Stroke Study. Stroke 1994; 25: 1935-1944.
- 4. Thrift AG, Dewey HM, Macdonell RA, et al. Stroke incidence on the east coast of Australia: the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke 2000; 31: 2087-2092.
- 5. Wilkinson PR, Wolfe CD, Warburton FB, et al. A long term follow-up of stroke patients. Stroke 1997; 28: 507-512.
- 6. Davis S, Donnan G. Modern management of acute stroke. Mod Med 1999; 42: 36-43.
- 7. Gorelick PB. Stroke prevention. Arch Neurol 1995; 52: 347-355.
- 8. Sacco RL, Benjamin EJ, Broderick JP, et al. American Heart Association Prevention Conference IV: prevention and rehabilitation of stroke: risk factors. Stroke 1997; 28: 1527-1529.
- 9. Thrift AG, Gilligan AK, Donnan GA. Major risk factors and protective factors: how to improve primary prevention of cerebrovascular disease. In: Fieschi C, Fisher M, editors. Prevention of ischaemic stroke. London: Martin Dunitz Ltd, 2000; 7-26.
- 10. SPSS [computer program]. Version 6.1.3. Chicago Ill: SPSS Inc, 1995.
- 11. Australian Bureau of Statistics. Population by age and sex: Australian states and territories, June 2000. Canberra: ABS, 2001. (Catalogue no. 3201.0.)
- 12. 1999 World Health Organization – International Society of Hypertension guidelines for the management of hypertension. Guidelines subcommittee. J Hypertens 1999; 17: 151-183.
- 13. Risk Factor Prevalence Study Management Committee. Risk Factor Prevalence Study: Survey Number 3, 1989. Canberra: National Heart Foundation of Australia and Australian Institute of Health, 1990.
- 14. Goldstein LB, Adams R, Becker K, et al. Primary prevention of ischemic stroke. A statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke 2001; 32: 280-299.
- 15. Sudlow M, Thomsen R, Thwaites B, et al. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet 1998; 352: 1167-1171.
- 16. Australian Institute of Health and Welfare. Australia's Health 1994: the fourth biennial health report of the Australian Institute of Health and Welfare. Canberra: AGPS, 1994.
- 17. National Health and Medical Research Council. A guide for general practitioners prevention of stroke. Canberra: NHMRC, 1996.
- 18. Psaty BM, Smith NL, Siscovick DS, et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA 1997; 277: 739-745.
- 19. Collaborative overview of randomised trials of antiplatelet therapy — I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists' Collaboration [published erratum appears in BMJ 1994; 308: 1540]. BMJ 1994; 308: 81-106.
- 20. Barnett HJM, Eliasziw M, Meldrum HE. Drugs and surgery in the prevention of ischaemic stroke. N Engl J Med 1995; 332: 238-248.
- 21. Blauw GJ, Lagaay AM, Smelt AHM, Westendorp RGJ. Stroke, statins, and cholesterol: a meta-analysis of randomised, placebo-controlled, double-blind trials with HMG-CoA reductase inhibitors. Stroke 1997; 28: 946-950.
- 22. Shinton R, Beevers G. Meta-analysis of relation between cigarette smoking and stroke. BMJ 1989; 298: 789-794.
- 23. Law MR, Frost CD, Wald NJ. Analysis of data from trials of salt reduction. BMJ 1991; 302: 819-824.
- 24. Klungel OH, Stricker BH, Paes AH, et al. Excess stroke among hypertensive men and women attributable to undertreatment of hypertension. Stroke 1999; 30: 1312-1318.





Abstract
Objectives: To determine the prevalence of stroke risk factors in a general practice population and to identify pharmacotherapies currently used in management of stroke risk factors.
Design: Multicentre, observational study by 321 randomly selected general practitioners who each collected data on 50 consecutive patients attending their surgery.
Patients and setting: 16 148 patients aged 30 years or older attending general practices across Australia during 2000.
Outcome measures: Prevalence of hypertension, current smoking, diabetes, hypercholesterolaemia, atrial fibrillation, recent history of stroke or TIA; extent of pharmacotherapy use in risk-factor management.
Results: 70% of patients had one or more risk factors and 34% had two or more. Hypertension was the risk factor with greatest prevalence (44%), followed by hypercholesterolaemia (43%) and current smoking (17%). The prevalence of risk factors generally increased with age, except for current smoking, where a decrease with age was seen. The most common pharmacotherapies were cardiovascular agents, followed by antiplatelet agents. Two-thirds of patients with hypertension were taking cardiovascular drugs, most commonly angiotensin-converting enzyme inhibitors.
Conclusions: Stroke risk factors are highly prevalent in general practice patients and GPs are ideally placed for opportunistic case-finding. There is considerable scope for improving management of stroke risk factors. The Avoid Stroke as Soon as Possible (ASAP) general practice stroke audit provides a baseline against which progress in risk-factor management can be measured.