Amiodarone is used in the management of cardiac dysrhythmias. Accumulation of amiodarone in the thyroid gland may result in thyroid dysfunction, either hypothyroidism or thyrotoxicosis.1
Amiodarone-associated thyrotoxicosis (AAT) occurs in about 3% of patients.2 In some patients, cessation of amiodarone is not practical, as it may be the only effective anti-arrhythmic agent. Furthermore, cessation of amiodarone may be followed by a rebound rise in tri-iodothyronine, which worsens the thyrotoxic state.3,4 Even when amiodarone can be discontinued, AAT can take up to nine months to resolve. Medical management may be ineffective and can result in complications, or sometimes death.5
In these very difficult situations, surgery has an important role. In the past it was thought that the risk of thyroid storm and the risks associated with anaesthesia would preclude surgery. However, recent experience has demonstrated that surgery may be performed safely and successfully, as illustrated in the case reports summarised in Box 1.
The patients all had severe cardiac disease and AAT refractory to medical treatment, yet general anaesthesia and total thyroidectomy were successful and uncomplicated in each case. All patients recovered rapidly and remain well and euthyroid on thyroxine replacement therapy. Patient 1 had a large multinodular goitre and the other four had normal-sized or slightly enlarged thyroid glands at the time of surgery. The histological findings in all cases showed a similar destructive thyroiditis (Box 2).
Up to 1996 only 20 cases of AAT treated by surgery had been reported.3,4,6-10 However, in the past few years, a further 29 cases have been documented.5,11,12 Including the five cases described here, there have been 54 cases, of which 19 (35%) have been in Australia. Even allowing for possible publication bias, the results are exceptionally good, with no surgical mortality reported.
It is standard practice to render thyrotoxic patients euthyroid preoperatively. This is not possible in AAT, yet postoperative thyroid storm appears to be an extremely rare event. Most patients are suitable for general anaesthesia, and local anaesthesia would probably be more stressful. There is discussion among anaesthetists as to the choice of anaesthetic agents, with some advocating total intravenous anaesthesia11,13 and others favouring inhalation anaesthesia.12
All authors agree that the medical management of patients with AAT is problematical and difficult.1,14 Apart from the doubtful success of medical treatment,5 it can be associated with prolonged illness and additional complications such as occurred in two of our patients, who had serious infections related to prednisone-induced immunosuppression that delayed the curative surgery. Thyroidectomy is the only treatment that reliably allows the continued use of amiodarone.15
Clinical decisions about apparent "unfitness for surgery" have sometimes been made without consulting an appropriate anaesthetist or endocrine surgeon. Despite the obvious difficulties with management of patients with AAT, anaesthesia and surgery may be performed safely and successfully. Consideration should be given to referring the patient for early surgery, particularly in cases where it would be advantageous to continue the amiodarone therapy and before complications of immunosuppression due to prednisone therapy have occurred. Lessons for practice are listed in Box 3.
2: Photomicrograph of thyroid in Patient 5
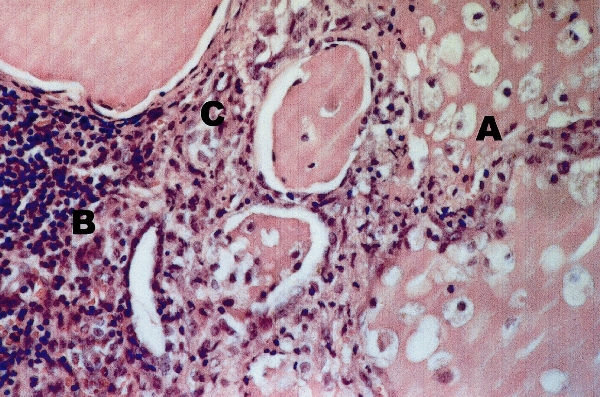
A: Destruction of follicles, with loss of follicular epithelial cells and macrophages in the colloid.
B: Marked inflammatory cell infiltration.
C: Fibroblasts creating fibrous tissue.
Haematoxylin and eosin stain; original magnification x 350. Courtesy of Queensland Medical Laboratory.
Amiodarone (an iodine-containing drug used for the treatment of cardiac arrhythmias) may cause a destructive thyroiditis, resulting in long-lasting thyrotoxicosis refractory to medical management.
Total thyroidectomy under general anaesthesia may be performed safely and successfully in patients with amiodarone-associated thyrotoxicosis.
- 1. Newman CM, Price A, Davies DW, et al. Amiodarone and the thyroid: a practical guide to the management of thyroid dysfunction induced by amiodarone treatment. Heart 1998; 79: 121-127.
- 2. Smyrk TC, Goellner JR, Brennan MD, Carney JA. Pathology of the thyroid in amiodarone-induced thyrotoxicosis. Am J Surg Pathol 1987; 11: 197-204.
- 3. Brennan MD, van Heerden JA, Carney JA. Amiodarone-associated thyrotoxicosis (AAT). Experience with surgical management. Surgery 1987; 102: 1062-1067.
- 4. Farwell AP, Abend SL, Huang SK, et al. Thyroidectomy for amiodarone-induced thyrotoxicosis. JAMA 1990; 263: 1526-1528.
- 5. Claxton S, Sinha SN, Donovan S, et al. Refractory amiodarone-associated thyrotoxicosis: an indication for thyroidectomy. Aust N Z J Surg 2000; 70: 174-178.
- 6. Samanta A, Jones GR, Burden AC, Barrie WW. Thoracic inlet compression due to amiodarone induced goitre. Postgrad Med J 1985; 61: 249-250.
- 7. Mehra A, Widerhorn J, Lopresti J, Rahimtoola SH. Amiodarone-induced hyperthyroidism: thyroidectomy under local anesthesia. Am Heart J 1991; 122: 1160-1161.
- 8. Mulligan DC, McHenry CR, Kinney W, Esselstyn CB Jr. Amiodarone-induced thyrotoxicosis: clinical presentation and expanded indications for thyroidectomy. Surgery 1993; 114: 1114-1119.
- 9. Painvin I, Dupuis JM, Victor J, et al. [Value of thyroidectomy in amiodarone-induced hyperthyroidism. Apropos of 3 cases.] Arch Mal Coeur Vaiss 1996; 89: 445-449.
- 10. Le Cosquer P, Guerin-Robardey AM, Ossart M. Amiodarone-induced thyrotoxicosis cured by thyroidectomy. Ann Fr Anesth Reanim 1996; 15: 1092-1094.
- 11. Hamoir E, Meurisse M, Defechereux T, et al. Surgical management of amiodarone-associated thyrotoxicosis: too risky or too effective? World J Surg 1998; 22: 537-543.
- 12. Sutherland J, Robinson B, Delbridge L. Anaesthesia for amiodarone-induced thyrotoxicosis: a case review. Anaesth Intensive Care 2001; 29: 24-29.
- 13. Gough IR, Meyer-Witting M. Surgery and anaesthesia for amiodarone-associated thyrotoxicosis. Aust N Z J Surg 2000; 70: 155-156.
- 14. Bartalena L, Brogioni S, Grasso L, et al. Treatment of amiodarone-induced thyrotoxicosis, a difficult challenge: results of a prospective study. J Clin Endocrinol Metab 1996; 81: 2930-2933.
- 15. Harjai KJ, Licata AA. Effects of amiodarone on thyroid function. Ann Intern Med 1997; 126: 63-71.





None declared.