The known Pain is the most common reason for emergency department presentations, but is often inadequately managed. Acupuncture is widely used in community settings, but only rarely in emergency departments.
The new Acupuncture was equivalent and non-inferior to pharmacotherapy in providing analgesia for patients with back pain and ankle sprain. There was no difference between groups in adverse events, acceptability or health resource use, but pain was not managed optimally by either acupuncture or pharmacotherapy, nor by their combination.
The implications Acupuncture is safe, acceptable and has an analgesic effect comparable with that of pharmacotherapy, but none of the therapeutic strategies used provided optimal analgesia within one hour of presentation.
Pain is the most common reason for emergency department (ED) presentations and is often inadequately managed.1-3 EDs are complex environments in which patients seek relief from undiagnosed pain, and clinicians must make timely decisions on the basis of limited information. This situation poses treatment challenges, and raises ethical and logistic problems for designing clinical trials that meet the pragmatic needs of patients and ED staff while also maintaining scientific rigour.4
Acupuncture is widely used by medical practitioners and other clinicians to relieve pain in community practice settings.5 Acupuncture can provide analgesia for chronic musculoskeletal pain and headache,6-9 and its use is covered by therapeutic guidelines for acute pain.10,11 However, there have been few clinical trials of acupuncture for treating acute pain, and few EDs offer it for pain relief.12-14 Two randomised controlled trials of acupuncture in ED settings have been published: one reported greater pain reduction with acupuncture together with standard therapy than with standard therapy alone,15 while the other reported significant neurological and functional recovery in patients with acute spinal cord injuries.16 A further study found that it reduced dental pain in patients waiting for emergency dental care.17 These studies, however, are insufficient for recommending that acupuncture be adopted in the ED, and they did not provide information on the length of stay or the applicability and acceptability of acupuncture.
Our study aimed to determine whether acupuncture is effective, safe, acceptable and feasible for patients presenting to the ED with low back pain, migraine or acute ankle injuries. The primary aim was to determine whether acupuncture alone or as an adjunct to pharmacotherapy is at least as effective as pharmacotherapy in providing clinically significant pain relief within an hour of presentation. The secondary aim was to determine whether acupuncture alone or as an adjunct improves functionality, is safe and acceptable to patients, and reduces health resource use.
Methods
Study design and setting
The study was a pragmatic, multicentre, single blinded, randomised, controlled trial comparing the effects of acupuncture, pharmacotherapy, and combined acupuncture and pharmacotherapy for treating patients presenting to EDs with ankle sprain, migraine or lower back pain. It was undertaken in four large tertiary hospitals in Melbourne — two public EDs (the Northern Hospital and the Alfred Hospital Emergency and Trauma Centre) and two private EDs (the Epworth and Cabrini Hospitals) — between January 2010 and December 2011. The full protocol of the trial has been reported previously.18
Selection of participants
Patients were included if they presented to the ED when an acupuncturist was present, and were at least 18 years old, required analgesia for acute low back pain, migraine or acute ankle injuries, and had a pain score of at least 4 on a 10-point verbal numerical rating scale (VNRS).19 Patients were excluded if the treating physician felt inclusion was inappropriate because of the signs of illness, or if the patient:
-
had a temperature above 37.7°C;
-
had experienced major trauma;
-
used anticoagulation medication or had a mechanical heart valve;
-
had skin infections precluding the use of certain acupuncture points;
-
refused or was unable to provide consent;
-
had used any form of analgesia in the 60 minutes before presenting to the ED; or
-
had presented to an ED for the same condition more than four times in the previous 3 months.
Randomisation and masking
Block randomisation employed a computerised randomisation sequence that stratified for each condition and site. Participants were not blinded to their treatment allocation. Single blinding was maintained by blinding assessors to treatment allocation, and acupuncturists to pharmacotherapy use.
Interventions
Acupuncture alone
Acupuncture was provided by either a registered Chinese medicine practitioner or an ED physician with medical acupuncture qualifications. Treatment protocols (online Appendix), determined by a panel of specialist acupuncturists, provided predetermined points for each condition, as well as additional points for individualising treatment.18
Pharmacotherapy alone
Pharmacotherapy was administered according to a standardised protocol based on the relevant national guidelines of the National Institute of Clinical Studies and the National Health and Medical Research Council.11,20,21 This protocol included first and second line drugs, as well as rescue medication administered at the discretion of the treating physicians, regardless of group allocation (Box 1).
Combined treatment
Combined therapy included both acupuncture and pharmacotherapy, with acupuncture administered 15 minutes before or after pharmacotherapy to maintain blinding of the acupuncturist.
Specific treatments
All ankle injury patients received rest, ice, compression and elevation regardless of their treatment allocation; migraine patients received intravenous fluids at the discretion of the treating physician. Rescue therapy, including parenteral opiates, was provided to patients with inadequate pain relief after one hour (T1), or earlier if the treating physician deemed it necessary.
Measurements
Pain was assessed at the delivery of the intervention (T0) by hospital nursing or allied health staff blind to treatment allocation, and then hourly (T1, T2 etc.) until discharge. It was assessed 36–60 hours after discharge by a blinded researcher from a different site via telephone. Data were recorded on a handwritten case record form, and entered (double data entry) into a secure online database.
The primary outcome measures were pain at T1 as measured on the VNRS (0 = no pain; 10 = worst pain imaginable) and recorded by blinded assessors.19 Clinically relevant pain relief was defined as achieving a VNRS score below 4, and statistically relevant pain relief as a reduction in VNRS score of greater than 2 units. Cross-sectional, between-group comparisons were deemed significant if there was a difference of at least 1.5 VNRS units. Secondary outcome measures included:
-
functionality for each condition at T48 as measured by the Oswestry Low Back Disability Questionnaire,22 the 24-hour Migraine Quality of Life questionnaire,23 or the Patient’s Global Assessment of Ankle Injury Scale;24
-
adverse events, rated from 0 (no impairment) to 10 (intolerable);
-
rescue medication use;
-
acceptability of treatment, recorded at T1, on leaving the ED, and at T48, based on ratings of satisfaction and willingness to repeat similar management in future;
-
health resource use, recorded at T48, including length of stay in the ED, length of stay in the hospital, admission rate, re-presentation rate, requirement for other health care professional advice, and additional analgesia or pharmacotherapy after initial presentation.
Statistical analysis
Power and sample size
The sample size calculation was based on testing of equivalence between the acupuncture only and pharmacotherapy only groups, and the testing of non-inferiority of acupuncture plus pharmacotherapy to pharmacotherapy only, overall and for each condition individually. A sample size of 505 participants was calculated to achieve 80% power (a = 0.05) after adjusting for an attrition rate of no more than 10%.
Analysis
The data were analysed by an independent, blinded statistician. Descriptive statistics for categorical variables are reported as numbers and percentages; continuous variables are reported as means with standards deviations (SDs) or medians with interquartile ranges (IQRs), and were compared in Pearson ?2 or Kruskal–Wallis equality of populations rank tests as appropriate. In intention-to-treat (ITT) analyses, the primary outcome measure (pain score at T1) was considered to be equivalent for the acupuncture only and pharmacotherapy only groups if the upper and lower confidence intervals of the between-group difference was less than 1.5 VNRS units. Non-inferiority between groups was also tested, and defined as the appropriate one-sided confidence interval of the group difference being no greater than 1.5 VNRS units at T1. Based on a = 0.05 for a two-sided equivalence test and 0.025 for a one-sided non-inferiority test, and adjusted for undertaking six tests, 99.2% and 99.6% confidence intervals for equivalence and non-inferiority testing respectively were calculated. The analyses were repeated as per protocol (PP) analyses when any patient in the acupuncture only group also received rescue pharmacotherapy, and was therefore considered to be in the acupuncture plus pharmacotherapy group. All analyses were conducted in Stata 13.1 (StataCorp).
Ethics approval
Ethics approval was provided by the Human Research Ethics Committees of RMIT University (reference, 12/09), the Northern Hospital (reference, CC16/09), the Alfred Hospital (reference, 21/10), the Cabrini Institute (reference, 01-11-04-11) and the Epworth Hospital (reference, 44409).
Results
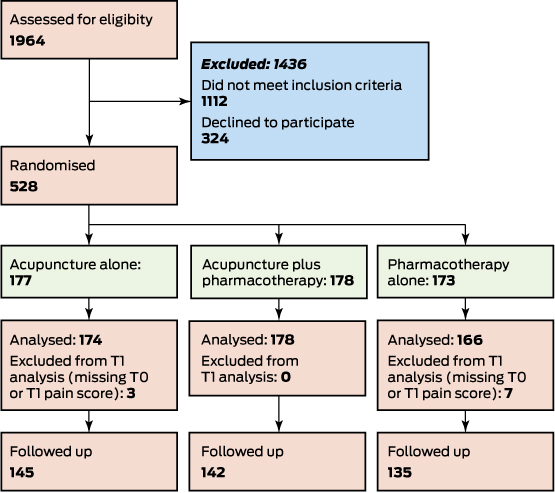
A total of 1964 patients were assessed between January 2010 and December 2011, of whom 528 were recruited (mean age, 41.0 years; SD, 15.1 years); 47.4% were women. The proportions of patients with each condition at each of the four study sites were similar; in total, 270 participants (51%) presented with low back pain, 92 (17%) with migraine, and 166 (31%) with ankle sprain. Patients were distributed equally across the three intervention arms, and there were no differences in pain scores or demographic characteristics between the groups at baseline (Box 2, Box 3).
The low back pain and ankle sprain groups, but not the migraine group, were powered at 80% for both equivalence and non-inferiority testing (based on recruitment numbers). Equivalence and non-inferiority of treatment groups was found overall and for the low back pain and ankle sprain groups in both ITT and PP analyses, except in the PP equivalence testing of the ankle sprain group. For the migraine group, neither the ITT nor the PP analyses indicated equivalence, nor did the ITT analysis indicate non-inferiority (Box 4, Box 5). Sensitivity analysis, which excluded those who received rescue therapy from the PP analysis, yielded similar results.
Between T0 and T1, the overall pain score decreased by a mean 2.1 VNRS units (SD, 2.3) to a mean T1 score of 6.4 units (SD, 2.7), with no statistically significant differences between treatment groups (Box 6). Overall, 16% of patients had clinically relevant pain relief and 36.9% statistically relevant pain relief at T1, with no statistically significant differences between the three groups (Box 6). There were no significant differences between the groups in the frequency of adverse events, acceptability, or health resource use (Box 6). At T1, 47% of the acupuncture only group, 49% of the combined group, and 57% of the pharmacotherapy only group stated they would definitely repeat their treatment. At T48, the number of patients willing to repeat acupuncture had increased, with 61% of the acupuncture only group willing to repeat their treatment, compared with 57% of the combined therapy group, and 52% of the pharmacotherapy only group (Box 6).
The two private hospitals were more likely to admit the treated patients than the two public hospitals (34.0% v 11.6%; P < 0.001). The overall admission frequencies by pain type were 2.2% for ankle sprain, 15.3% for migraine, and 21.7% for low back pain (P < 0.001).
The acupuncture only group received significantly more rescue medication therapy than the groups that received pharmacotherapy (at T1: P = 0.016; after T1: P = 0.008; Box 6). Oral opiate medication was offered as first line rescue medication to patients in the acupuncture group and parenteral opiates to the two pharmacotherapy groups. The overall mean functional disability scores decreased significantly between T0 and T48 in all groups (P < 0.001), with no significant differences between groups over time (Box 7).
Discussion
This study was the largest randomised controlled trial of acupuncture in an ED. We found that acupuncture, alone or in conjunction with pharmacotherapy, provides analgesia comparable with that achieved by pharmacotherapy for patients presenting to the ED with low back pain and ankle sprain, but not for those with migraine. Pain for many patients was not adequately managed at T1 by any of the interventions. Across the three arms, fewer than 40% of participants experienced a reduction in pain of 2 points or more (ie, statistically relevant), and at T1 more than 80% of patients had a pain rating above 4.
Although the three treatments were similarly ineffective at reducing pain at T1, most patients found their treatment acceptable at T48, about 80% of each group stating they would probably or definitely repeat their treatment. This is consistent with recent research that suggests the informational value of pain scores in ED settings is limited, and that patient satisfaction is not necessarily correlated with reduced pain scores.3 It is also notable that the proportion of participants receiving acupuncture alone who were satisfied with their treatment increased from 47% at T1 to 61% at T48, whereas the proportion of those receiving pharmacotherapy declined from 57% to 52%. The T48 figures are arguably more important than T1 measures, as they are less likely to be confounded by the time of analgesia onset and uncertainty about the length of stay, transport arrangements and other factors.
While pain reduction at T1 was similar for all three groups, patients in the acupuncture group were almost twice as likely to receive rescue analgesia. This may indicate that acupuncture was ineffective and patients sought alternative analgesia or that they were more likely to accept pharmacotherapy because they felt they had missed out on standard care, whereas patients who had already received oral opiates were reluctant to accept parenteral opiates. Patients treated with acupuncture who received rescue medication were classified as having received pharmacotherapy in the PP analysis, in which the equivalence and non-inferiority of groups were maintained, but we cannot discount the possibility that this may partly reflect the potentially self-limiting nature of the treated conditions.
As four sites participated in our study, including two large private and two large public hospitals in diverse geographic and socio-economic areas, our results should be generalisable to the broader Australian ED patient population. Our study included patients presenting with acute pain caused by different pathophysiological processes (musculoskeletal, vascular, traumatic), but our results may not apply to other painful conditions. Acupuncture may induce analgesic effects similar to those of some pharmacological agents, but it may also have additional non-specific effects, modulated by patients’ perceptions and expectations.25 As this was a pragmatic study designed for an ED environment, timing and ethical considerations prevented controlling for non-specific effects by including a placebo group.
There is a clear demand for analgesia in the ED and a multimodal approach is desirable given concerns about the use of opioids and the potential for addiction. Some Australian EDs already offer acupuncture as an alternative when trained staff are available, and the relative efficacy, acceptability and safety of acupuncture support its playing a role in non-pharmacological analgesia in acute care settings. Acupuncture may also improve patient satisfaction by providing analgesia to patients with contraindications for certain drugs, and for those who prefer acupuncture. Pain management in EDs in general must be improved. The potential role of acupuncture should also be further explored, including determining the conditions in which it is most useful and the feasibility of employing it in emergency settings, including acupuncture training for emergency physicians and allied health personnel.
Conclusion
Neither acupuncture nor standard pharmacotherapy afforded patients presenting to EDs with back pain, ankle injury or migraine clinically relevant reduction in pain within an hour. Nevertheless, patients found both treatments acceptable, and the effectiveness of acupuncture alone was comparable with that of pharmacotherapy. Our finding that acupuncture was a safe and acceptable form of acute analgesia suggests it may be useful as an adjunct to pharmacotherapy or when pharmacotherapy is unsuitable. However, as no therapy provided optimal acute analgesia, more effective options are needed.
Box 1 – Protocol for relief of pain by pharmacotherapy
|
|
Ankle sprain |
Lower back pain |
Migraine |
||||||||||||
|
|
|||||||||||||||
|
First line therapy options |
|
|
|
||||||||||||
|
Diazepam (5mg) |
|
x |
|
||||||||||||
|
Hartmann’s solution (5% dextrose, 0.9% NaCl) |
x |
x |
x |
||||||||||||
|
Metoclopramide (10–20mg iv) or prochlorperazine (12.5mg im) (if nausea and vomiting are significant) |
|
|
x |
||||||||||||
|
Paracetamol (1g) |
x |
x |
x |
||||||||||||
|
Paracetamol (500mg) with codeine (30mg) |
x |
x |
x |
||||||||||||
|
Tramadol (50–100mg) |
x |
x |
x |
||||||||||||
|
Dextropropoxyphene (32.5mg) and paracetamol (325mg) |
x |
x |
x |
||||||||||||
|
Ibuprofen (400mg), diclofenac (50mg) or indomethacin (100mg) as needed |
x |
x |
x |
||||||||||||
|
Second line therapy options (after one hour) |
|||||||||||||||
|
Morphine (2.5mg iv, boluses) |
x |
x |
x |
||||||||||||
|
Chlorpromazine (25mg in 1000mL normal saline iv) |
|
|
x |
||||||||||||
|
|
|||||||||||||||
|
im=intramuscular; iv= intravenous. |
|||||||||||||||
Box 2 – Flowchart of the selection of participants for the trial of acupuncture, alone or in combination with pharmacotherapy, for the treatment of pain in the emergency department
Box 3 – Baseline characteristics of the 528 patients randomised to treatment, by treatment group
|
|
Treatment group |
||||||||||||||
|
All patients |
Acupuncture only |
Acupuncture and pharmocotherapy |
Pharmacotherapy only |
||||||||||||
|
|
|||||||||||||||
|
Number of patients |
528 |
177 |
178 |
173 |
|||||||||||
|
Sex (women) |
250 (47%) |
85 (48%) |
83 (47%) |
82 (47%) |
|||||||||||
|
Age (years), mean (SD) |
41.0 (15.1) |
42.1 (15.8) |
40.5 (14.5) |
40.3 (15.0) |
|||||||||||
|
Pain at T0, mean (SD) |
8.5 (1.6) |
8.5 (1.6) |
8.5 (1.6) |
8.5 (1.6) |
|||||||||||
|
Hospital |
|
|
|
|
|||||||||||
|
Site 1 |
135 (26%) |
46 (26%) |
45 (25%) |
44 (25%) |
|||||||||||
|
Site 2 |
16 (3%) |
6 (3%) |
6 (3%) |
4 (2%) |
|||||||||||
|
Site 3 |
46 (9%) |
16 (9%) |
15 (8%) |
15 (9%) |
|||||||||||
|
Site 4 |
331 (63%) |
109 (62%) |
112 (63%) |
110 (64%) |
|||||||||||
|
Pain type |
|
|
|
|
|||||||||||
|
Ankle |
166 (31%) |
54 (30%) |
57 (32%) |
55 (32%) |
|||||||||||
|
Migraine |
92 (17%) |
31 (18%) |
30 (17%) |
31 (18%) |
|||||||||||
|
Low back |
270 (51%) |
92 (52%) |
91 (51%) |
87 (50%) |
|||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 4 – Equivalence testing: mean difference in pain level at T1 between acupuncture and pharmacotherapy groups, overall and by pain type. A, Intention-to-treat analysis; B, per protocol analysis
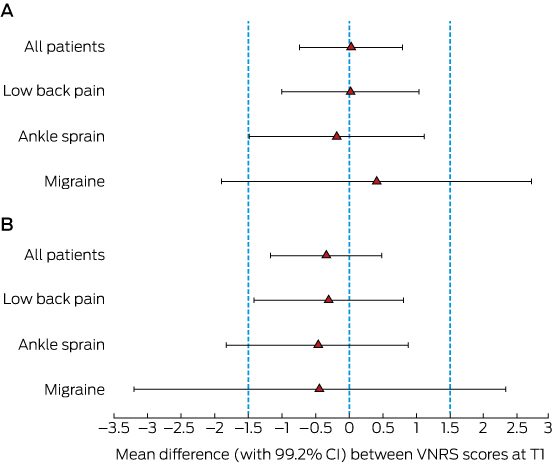
*Non-equivalence defined by 99.2% confidence interval exceeding ±1.5 verbal numerical rating scale (VNRS) units.
Box 5 – Non-inferiority testing: mean difference in pain level at T1 between treatment groups, overall and by pain type: acupuncture only v combined therapy (A, intention-to-treat analysis; B, per protocol analysis); acupuncture only v pharmacotherapy and combined therapy (C, intention-to-treat analysis; D, per protocol analysis)
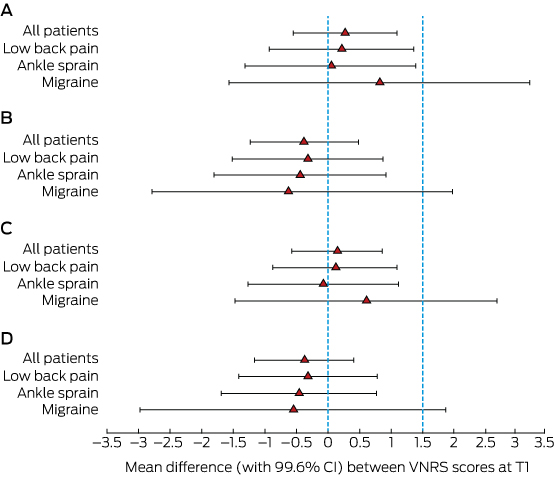
Non-inferiority defined by upper 99.6% confidence interval exceeding 1.5 on verbal numerical rating scale (VNRS).
Box 6 – Intention-to-treat analyses of pain measures, secondary outcomes, acceptability and health resource use, by treatment group*
|
|
Treatment group |
P |
|||||||||||||
|
All patients |
Acupuncture only |
Acupuncture and pharmocotherapy |
Pharmacotherapy only |
||||||||||||
|
|
|||||||||||||||
|
Pain measures |
|
|
|
|
|
||||||||||
|
Pain at one hour (N = 518) |
|
|
|
|
|
||||||||||
|
Score, mean (SD) |
6.4 (2.7) |
6.6 (2.6) |
6.3 (2.8) |
6.5 (2.7) |
0.57 |
||||||||||
|
Decrease, T0 to T1, mean (SD) |
2.1 (2.3) |
1.9 (2.3) |
2.2 (2.2) |
2.0 (2.3) |
0.29 |
||||||||||
|
Score < 4 at T1 (clinically relevant) |
81 (16%) |
23 (13%) |
30 (17%) |
28 (17%) |
0.56 |
||||||||||
|
Decrease, T0 to T1, > 2 (statistically relevant) |
191 (36.9%) |
58 (33%) |
68 (38%) |
65 (39%) |
0.49 |
||||||||||
|
Secondary outcomes |
|
|
|
|
|
||||||||||
|
Rescue therapy (N = 528) |
|
|
|
|
|
||||||||||
|
At T1 |
98 (19%) |
45 (25%) |
27 (15%) |
26 (15%) |
0.016 |
||||||||||
|
After T1 |
45 (8.5%) |
24 (14%) |
8 (4.5%) |
13 (7.5%) |
0.008 |
||||||||||
|
Functionality (see ) |
|
|
|
|
|
||||||||||
|
Any adverse events (N = 422) |
216 (51.7%) |
73 (51%) |
71 (50%) |
72 (54%) |
0.84 |
||||||||||
|
Acceptability |
|
|
|
|
|
||||||||||
|
Satisfaction survey |
|
|
|
|
|
||||||||||
|
T1, mean (SD) (N = 519) |
7.1 (2.7) |
7.1 (2.8) |
7.0 (3.0) |
7.2 (2.4) |
0.91 |
||||||||||
|
T48, mean (SD) (N = 422) |
7.6 (2.7) |
7.6 (2.7) |
7.8 (2.6) |
7.5 (2.8) |
0.86 |
||||||||||
|
Willingness to repeat |
|
|
|
|
|
||||||||||
|
T1 (N = 511) |
|
|
|
|
0.015 |
||||||||||
|
Definitely no |
18 (3.5%) |
11 (6.4%) |
6 (3.4%) |
1 (0.6%) |
|
||||||||||
|
Probably no |
46 (9.0%) |
20 (12%) |
17 (9.7%) |
9 (5.6%) |
|
||||||||||
|
Probably yes |
153 (29.9%) |
49 (28%) |
60 (34%) |
44 (27%) |
|
||||||||||
|
Definitely yes |
259 (50.7%) |
81 (47%) |
86 (49%) |
92 (57%) |
|
||||||||||
|
Unsure |
35 (6.9%) |
12 (6.9%) |
7 (4.0%) |
16 (9.9%) |
|
||||||||||
|
T48 (N = 422) |
|
|
|
|
0.64 |
||||||||||
|
Definitely no |
22 (5.3%) |
5 (3.5%) |
8 (5.7%) |
9 (6.8%) |
|
||||||||||
|
Probably no |
21 (5.0%) |
10 (6.9%) |
6 (4.3%) |
5 (3.8%) |
|
||||||||||
|
Probably yes |
101 (24.1%) |
32 (22%) |
34 (24%) |
35 (26%) |
|
||||||||||
|
Definitely yes |
237 (56.6%) |
88 (61%) |
80 (57%) |
69 (52%) |
|
||||||||||
|
Unsure |
38 (9.1%) |
10 (6.9%) |
13 (9.2%) |
15 (11%) |
|
||||||||||
|
Health resource use |
|
|
|
|
|
||||||||||
|
ED LOS (hours), median (IQR) |
3.8 (2.9–4.9) |
3.8 (2.9–4.9) |
3.7 (2.8–4.8) |
3.9 (2.7–5.3) |
0.87 |
||||||||||
|
Hospital LOS (hours), median (IQR) |
3.8 (2.8–5.7) |
3.9 (2.9–6.0) |
3.7 (2.8–5.2) |
4.0 (2.7–5.8) |
0.52 |
||||||||||
|
Admission rate (N = 422) |
60 (14%) |
27 (19%) |
13 (9.2%) |
20 (15%) |
0.07 |
||||||||||
|
Re-presentation rate (N = 422) |
13 (3.1%) |
2 (1.4%) |
6 (4.2%) |
5 (3.8%) |
0.33 |
||||||||||
|
Other health care professional (N = 422) |
108 (25.8%) |
39 (27%) |
36 (26%) |
33 (25%) |
0.93 |
||||||||||
|
Additional analgesia/pharmacotherapy (N = 422) |
343 (82.1%) |
117 (81.3%) |
116 (82.3%) |
110 (82.7%) |
0.95 |
||||||||||
|
|
|||||||||||||||
|
ED=emergency department; LOS=length of stay. |
|||||||||||||||
Box 7 – Secondary outcomes: functionality by pain type and treatment group
|
|
Treatment group |
P |
|||||||||||||
|
All patients |
Acupuncture only |
Acupuncture and pharmocotherapy |
Pharmacotherapy only |
||||||||||||
|
|
|||||||||||||||
|
Low back pain (Oswestry Low Back Disability Questionnaire) |
|||||||||||||||
|
T0, mean (SD) |
37.5 (8.6) |
36.3 (9.4) |
38.5 (8.8) |
37.8 (7.4) |
0.29 |
||||||||||
|
T48, mean (SD) |
28.2 (11.8) |
27.9 (12.7) |
27.4 (11.5) |
29.3 (11.1) |
0.52 |
||||||||||
|
Migraine (Migraine Quality of Life) |
|
|
|
|
|
||||||||||
|
T0, mean (SD) |
87.6 (13.1) |
90.6 (11.4) |
89.1 (12.9) |
83.0 (14.1) |
0.038 |
||||||||||
|
T48, mean (SD) |
48.0 (28.9) |
52.0 (28.3) |
41.5 (28.3) |
49.9 (30.4) |
0.50 |
||||||||||
|
Ankle (Ankle Injury Scale) |
|
|
|
|
|
||||||||||
|
T0, mean (SD) |
4.03 (0.85) |
4.13 (0.99) |
4.02 (0.74) |
3.95 (0.80) |
0.31 |
||||||||||
|
T48, mean (SD) |
2.96 (1.04) |
3.09 (1.00) |
2.96 (1.08) |
2.82 (1.04) |
0.33 |
||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 29 June 2016, accepted 25 January 2017
- Marc M Cohen1
- De Villiers Smit2
- Nick Andrianopoulos3
- Michael Ben-Meir4
- David McD Taylor5
- Shefton J Parker1
- Chalie C Xue1
- Peter A Cameron2,6
- 1 RMIT University, Melbourne, VIC
- 2 The Alfred Hospital, Melbourne, VIC
- 3 Monash Centre of Cardiovascular Research and Education in Therapeutics, Melbourne, VIC
- 4 Cabrini Hospital, Melbourne, VIC
- 5 Austin Health, Melbourne, VIC
- 6 Monash University, Melbourne, VIC
The trial was supported by a grant from the National Health and Medical Research Council (#555427).
No relevant disclosures.
- 1. Grant PS. Analgesia delivery in the ED. Am J Emerg Med 2006; 24: 806-809.
- 2. Stalnikowicz R, Mahamid R, Kaspi S, Brezis M. Undertreatment of acute pain in the emergency department: a challenge. Int J Qual Health Care 2005; 17: 173-176.
- 3. Taylor DM, Fatovich DM, Finucci DP, et al. Best-practice pain management in the emergency department: a cluster-randomised, controlled, intervention trial. Emerg Med Australas 2015; 27: 549-557.
- 4. Shergis JL, Parker S, Coyle ME, et al. Key considerations for conducting Chinese medicine clinical trials in hospitals. Chin Med 2013; 8: 3.
- 5. Cohen M, Pirotta M, Da Costa C. The integration of complementary therapies in Australian general practice: results of a National Survey. J Altern Complement Med 2005; 11: 995-1004.
- 6. Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012; 172: 1444-1453.
- 7. Madsen MV, Gotzsche PC, Hrobjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ 2009; 338: a3115.
- 8. Hopton A, MacPherson H. Acupuncture for chronic pain: is acupuncture more than an effective placebo? A systematic review of pooled data from meta-analyses. Pain Pract 2010; 10: 94-102.
- 9. Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain 2011; 152: 755-764.
- 10. eTG complete [website]. Melbourne: Therapeutic Guidelines, 2014. https://tgldcdp.tg.org.au/etgcomplete (accessed Dec 2016).
- 11. Macintyre PE, Schug SA, Scott DA, et al; APM:SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Acute pain management: scientific evidence. 3rd edition. Melbourne: ANZCA and FPM, 2010. https://sydney.edu.au/medicine/pmri/pdf/Acute-pain-management-scientific-evidence-third-edition.pdf (accessed Dec 2016).
- 12. Zhang AP, Parker SJ, Smit de V, et al. Acupuncture and standard emergency department care for pain and/or nausea and its impact on emergency care delivery: a feasibility study. Acupuncture Med 2014; 32: 250-256.
- 13. Fleckenstein J, Schottdorf J, Kreimeier U, Irnich D. Acupuncture in emergency medicine: results of a case series. Anaesthetist 2011; 60: 854-862.
- 14. Reinstein AS, Erickson LO, Griffin KH, et al. Acceptability, adaptation, and clinical outcomes of acupuncture provided in the emergency department: a retrospective pilot study. Pain Med 2016; 18:169-178.
- 15. Goertz C, Niemtzow R, Burns SM, et al. Auricular acupuncture in the treatment of acute pain syndromes: a pilot study. Mil Med 2006; 171: 1010-1014.
- 16. Wong A, Leong CP, Su TY, et al. Clinical trial of acupuncture for patients with spinal cord injuries. Am J Phys Med Rehabil 2003; 1: 21-27.
- 17. Grillo CM, Wada RS, da Luz Rosário de Sousa M. Acupuncture in the management of acute dental pain. J Acupunct Meridian Stud 2014; 7: 65-70.
- 18. Cohen M, Parker S, Taylor D, et al. Acupuncture as analgesia for low back pain, ankle sprain and migraine in emergency departments: study protocol for a randomized controlled trial. Trials 2011; 12: 241.
- 19. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med 2003; 10: 390-392.
- 20. Holdgate AK, Kelly, AM. Management of acute migraine (Emergency care evidence in practice series). Melbourne: National Institute of Clinical Studies, 2006. https://www.nhmrc.gov.au/_files_nhmrc/file/nics/programs/Management%20of%20acute%20migraine%20%5BPDF%20190KB%5D.pdf? (accessed Dec 2016).
- 21. Australian Acute Musculoskeletal Pain Guidelines Group. Evidence-based management of acute musculoskeletal pain: a guide for clinicians. Brisbane: Australian Academic Press, 2003. https://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/cp94_evidence_based_management_acute_musculoskeletal_pain_131223.pdf (accessed Dec 2016).
- 22. Fairbank J, Couper J, Davies JB, O’Brian JP. The Oswestry low back pain disability questionnaire. Physiotherapy 1980; 8: 271-273.
- 23. Santanello NC, Hartmaier SL, Epstein RS, Silberstein SD. Validation of a new quality of life questionnaire for acute migraine headache. Headache 1995; 35: 330-337.
- 24. Petrella R, Ekman E, Schuller R, Fort J. Efficacy of celecoxib, a COX-2-specific inhibitor, and naproxen in the management of acute ankle sprain: results of a double-blind, randomized controlled trial. Clin J Sport Med 2004; 14: 225-231.
- 25. Vase L, Baram S, Takakura N, et al. Specifying the nonspecific components of acupuncture analgesia. Pain 2013; 154: 1659-1667.





Abstract
Objectives: This study aimed to assess analgesia provided by acupuncture, alone or in combination with pharmacotherapy, to patients presenting to emergency departments with acute low back pain, migraine or ankle sprain.
Design: A pragmatic, multicentre, randomised, assessor-blinded, equivalence and non-inferiority trial of analgesia, comparing acupuncture alone, acupuncture plus pharmacotherapy, and pharmacotherapy alone for alleviating pain in the emergency department.
Setting, participants: Patients presenting to emergency departments in one of four tertiary hospitals in Melbourne with acute low back pain, migraine, or ankle sprain, and with a pain score on a 10-point verbal numerical rating scale (VNRS) of at least 4.
Main outcome measures: The primary outcome measure was pain at one hour (T1). Clinically relevant pain relief was defined as achieving a VNRS score below 4, and statistically relevant pain relief as a reduction in VNRS score of greater than 2 units.
Results: 1964 patients were assessed between January 2010 and December 2011; 528 patients with acute low back pain (270 patients), migraine (92) or ankle sprain (166) were randomised to acupuncture alone (177 patients), acupuncture plus pharmacotherapy (178) or pharmacotherapy alone (173). Equivalence and non-inferiority of treatment groups was found overall and for the low back pain and ankle sprain groups in both intention-to-treat and per protocol (PP) analyses, except in the PP equivalence testing of the ankle sprain group. 15.6% of patients had clinically relevant pain relief and 36.9% had statistically relevant pain relief at T1; there were no between-group differences.
Conclusion: The effectiveness of acupuncture in providing acute analgesia for patients with back pain and ankle sprain was comparable with that of pharmacotherapy. Acupuncture is a safe and acceptable form of analgesia, but none of the examined therapies provided optimal acute analgesia. More effective options are needed.
Trial registration: Australian New Zealand Clinical Trials Registry, ACTRN12609000989246.