The main source of vitamin D for Australians is exposure to sunlight. The National Health and Medical Research Council's recommended dietary intake for vitamin D in Australia assumes that most Australians receive sufficient sunlight to more than adequately meet their vitamin D requirements.1 Current lifestyle and work environments in developed countries, however, may be contributing to an increased prevalence of vitamin D deficiency, particularly in winter.2 Many people leave for work early in the morning, return home after dark, and drive to and from work, so that, during winter, they have limited sunlight exposure for five out of every seven days. Certain population groups, such as the elderly and dark-skinned and/or veiled women and their children, are at particular risk for vitamin D deficiency, and the latter group accounts for the recent upsurge in the number of cases of rickets in developed countries.3-5
It is important to note that physiological dysfunction appears to occur at much higher serum levels of 25-hydroxyvitamin D3 (25OHD; the indicator of vitamin D status) than those required to demonstrate adverse effects on bone and clinical signs of deficiency.6 Thus, the distinction between vitamin D deficiency and insufficiency may no longer be useful, as suboptimal vitamin D levels contribute to the development of osteoporosis.7 Osteoporosis is a major risk factor for hip fractures, one of the major causes of death and disability in the elderly,8 and, in this group, supplementation with vitamin D3 and calcium reduces the risk of hip fractures and other non-vertebral fractures.9 A summary of the metabolism and action of vitamin D is given in Box 1.
Several studies have assessed vitamin D status in Australia and New Zealand. The prevalence of deficiency varies,2,14-18 but is acknowledged to be much higher than previously thought. Deficiency is classified as either marginal (25OHD levels ranging from 25 to 50 nmol/L) or frank (25OHD levels, < 20–25 nmol/L). The highest rates of frank deficiency occur in dark-skinned, veiled, pregnant women (80%),14 with similarly high rates found in mothers of infants treated for rickets.15 Another high-risk group is the elderly, with marginal deficiency rates of 76% in nursing home residents, and 53% in hostel residents.18 Other studies assessing younger adults have reported marginal deficiency rates of 23%16 and 43%,2 with 8% of young women (20–39 years) found to have frank deficiency at the end of winter in Geelong (Victoria, latitude 38°S).2
In general, cutaneous synthesis provides most of the vitamin D to the body (80%–100%),19 and with adequate sunlight exposure dietary vitamin D may be unnecessary.20 Most Australians obtain almost all their vitamin D requirements through casual exposure to sunlight. Vitamin D stored in the adipose tissue is available during the winter, when sunlight exposure is minimal. However, age, skin colour, time spent outdoors, latitude and angle of the sun can all significantly influence the cutaneous production of vitamin D and therefore affect vitamin D status.
Only a few foods contain significant amounts of vitamin D. Rich sources are fish, especially fish with a high fat content, such as sardines, salmon, herring and mackerel. Other sources of importance are meat, milk and eggs, and fortified foods such as margarine.
The recommended dietary intakes of vitamin D in Australia and the United States are given in Box 2.
Fortification with vitamin D for different foods may be mandatory (specific foods must contain a certain level of a vitamin), or voluntary (manufacturers are permitted to add vitamins to specific foods, but are not required to do so). Accordingly, food regulations dictate the level and types of foods that may be fortified. However, when fortification is voluntary, the number of foods that manufacturers choose to fortify with vitamin D can determine the intake of the population.
In the United States, manufacturers voluntarily fortify a large number of foods with vitamin D — milk, margarine, breakfast cereals, pastries, breads.
In Europe, fortification with vitamin D varies and the level of fortification can be quite low. In Finland,23 only margarine-type products are fortified with vitamin D, and in the United Kingdom whole milk is not fortified with vitamin D, but there is vitamin D fortification of margarine.
In Australia, there is mandatory fortification of table edible oil spreads (eg, low-fat spreads) and table margarine, and voluntary fortification of modified and skim milks, and powdered milk, yoghurts and table confections (eg, Frûche dairy products) and cheese.
In New Zealand fortification of margarine is not mandatory, but since 1996 voluntary fortification of margarine, fats and dairy food items has been permitted.
The major food sources of vitamin D vary according to fortification practices. In the United Kingdom, with the increasing fortification of cereals, the main food sources of vitamin D are now cereal products (33%).24 When whole milk and margarine are both fortified, milk takes over as the major source of vitamin D.25 In Australia, for the Commonwealth Scientific and Industrial Research Organisation (CSIRO) National Dietary Survey of 1998–99 by Baghurst and Record (Dr Katrine Baghurst, Program Manager, CSIRO, Health Sciences and Nutrition, personal communication), it was estimated that margarine provides up to 48% of the total vitamin D intake for men and women, followed by canned fish (16%), and eggs (10%).
Box 3 summarises studies that have assessed dietary intake of vitamin D with various levels of food fortification. The average estimated intake in Australians is low, varying from 1.2–2.6 µg/day.2,25 The range of vitamin D intakes found in the CSIRO National Dietary Survey indicated that very few adults reach 10 µg/day. For men, the highest decile of intake was only 5.6 µg/day and the average intake was 2.6–3.0 µg/day; for women, it was 2.0–2.2 µg/day. Similarly, the Australia New Zealand Food Authority (ANZFA) has estimated population mean vitamin D intakes to be similar for men and women (2.0–2.4 µg/day), using the food additive modelling system.26 Dietary intakes of vitamin D are generally low, with the highest mean intake for any population studied being 6.4 µg/day (Box 3).23-25,27-33 A review of 31 studies from the northern hemisphere, assessing vitamin D intake in young adults and the elderly, found regional differences.28 Vitamin D intake per day was lower in Europe, where whole milk is not fortified.28 In the United States, where more products are fortified, the mean intakes were about 60% higher.28,31 Fortification of foods, particularly milk, appears to increase the mean vitamin D intake of a country's population, but groups with a lower energy intake, such as women with osteoporosis25 and those in residential care,33 have lower intakes than the general population. Therefore, it is probably an unrealistic expectation that most people will achieve dietary vitamin D intakes of 5–10 µg/day with the current fortification practices in Australia. For example, to reach an intake of 5 µg/day of vitamin D, one would have to consume two tablespoons of margarine, or three tablespoons of sardines or 1000 mL of fortified skim milk.
Some experts believe that fortification, as a way of increasing vitamin D intake, will be unsuccessful, because the actual amount of vitamin D varies greatly in fortified foods. Furthermore, people with restricted dietary intakes (such as the elderly) will not benefit greatly from fortification.34
Keane et al assessed the effect of vitamin D-fortified milk on serum vitamin D in community-dwelling elderly people.35 They found that daily use of 500 mL of fortified milk for three months (providing 5 µg/day of vitamin D) significantly increased serum 25OHD levels, but was insufficient to correct deficiencies.
A study in England found that serum 25OHD levels were higher in people who consumed margarine daily compared with those who consumed margarine less often, but levels were still low in both groups.36
Rasmussen et al37 assessed the potential effectiveness of fortification of milk, butter/margarine and a combination of these foods to increase the intake of vitamin D in the Danish population. They concluded that fortification of milk is far from optimal (because of the skewed distribution of milk intake), but that the combined fortification of milk (1.1 µg/100 g) and butter/margarine (9.5 µg/100 g) would be optimal, resulting in few people with intakes above 40 µg/day, and ensure that most people have intakes of at least 10 µg/day, although many of the high-risk group (the elderly) would still have intakes less than 10 µg/day.
If the aim of a fortification program were to relieve an established deficiency, it probably would not achieve this outcome in the elderly, the largest and most vulnerable group. These results are confirmed by the ANZFA, which assessed the impact on vitamin D intakes of fortifying whole milk to a level of 1.0 µg/200 mL.26 This resulted in median intakes of 5.5 µg/day for men and 3.8 µg/day for women in Australia.
The prevalence of vitamin D deficiency in Australia appears to be much higher than was previously thought, with evidence of vitamin D deficiency detected in up to 80% of dark-skinned, veiled or unveiled women during pregnancy, up to 76% of elderly people in institutions and 23% of younger adults. During times of reduced exposure to sunlight (eg, when an individual is confined inside, or during winter), vitamin D status is related to dietary vitamin D intake.
To devise an appropriate health message for vitamin D, we need to balance the need for sunshine against the risk of skin cancer. Dark-skinned, veiled women and older people (particularly those in residential care) have reduced exposure to sunlight and increased requirements. The dietary intake of vitamin D of Australians is low and is inadequate to meet the vitamin D requirements of at-risk groups. Current levels of vitamin D food fortification are insufficient to prevent deficiencies. It is unlikely that expansion of the fortification of our food supply would be effective in correcting deficiencies in the groups at greatest risk, although it may assist in maintaining vitamin D status in other groups. Other solutions, such as vitamin D supplementation and/or increased exposure to sunlight, must be considered for at-risk groups.
1: Metabolism and actions of Vitamin D
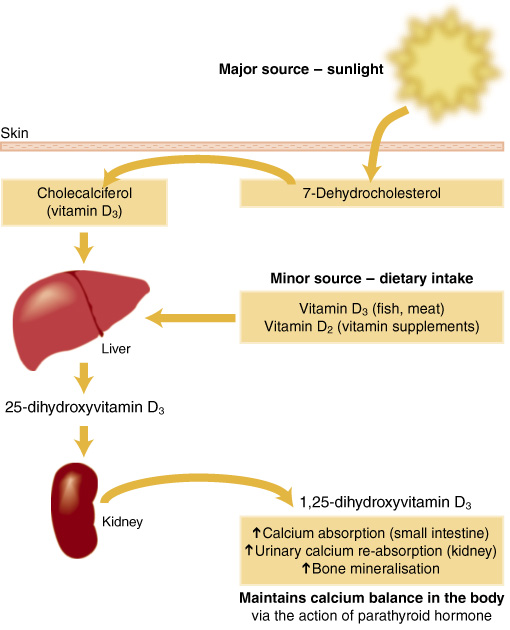 |
Vitamin D was originally classified as a nutrient when cod liver oil (a source of vitamin D) was found to have an antirachitic effect in infants.10 Further research showed that exposure to sunlight or ultraviolet (UV) light could also prevent and cure rickets. There are two forms of vitamin D: Cholecalciferol (vitamin D3) is made from 7-dehydrocholesterol in the skin of animals and humans. The action of UV light on the skin, followed by thermic isomerisation, produces cholecalciferol. This form is generally used in the fortification of foods and is present in cod liver oil (and other food sources of vitamin D). Ergocalciferol (vitamin D2) is produced by UV irradiation of the fungal steroid ergosterol. This appears to be a rare form, but is the one used in some vitamin D supplements. Vitamin D's main role is to maintain serum calcium and phosphorus levels within the normal range to sustain a wide variety of metabolic and physiological functions, including maintaining bone health and normal neuromuscular function. Adequate vitamin D is required to upregulate calcium absorption in times of increased requirement (growth, pregnancy) and when dietary calcium intake is low.11 Vitamin D also appears to have other roles within the body, such as enhancing immune function.12 Levels of serum 25-hydroxyvitamin D3 (25OHD), the indicator of vitamin D status, are usually a direct result of UV irradiation of the skin, but in times of minimal exposure to UV light they can reflect levels of dietary intake.2,13 Vitamin D deficiency results in bone disease: rickets in children and osteomalacia in adults. |
2: Recommended dietary intakes of vitamin D
Australia (1991)
The National Health and Medical Research Council recommends that
pregnant women and young children receive reasonable summer sunlight exposure;
those who are housebound or not exposed to direct sunlight for at least 1–2 hours per week should have a daily oral intake of 10 μg (400 IU) vitamin D; and
food sources of vitamin D should be included in the diets of the elderly.1
United States (1997)
The Food and Nutrition Board of the Institute of Medicine of the US National Academy of Sciences has proposed the following dietary reference intakes for vitamin D:
3: Studies estimating dietary intake of vitamin D, grouped by level of fortification
Studies |
Population group |
Vitamin D intake (µg/day) (mean [SD], median or range) |
|||||||||
Fortified margarine (only) |
|||||||||||
ANZFA26 |
Adults |
2.2 (median) |
|||||||||
Baghurst and Record 2001* |
Adults |
2.6 (M); 2.0 (F) |
|||||||||
Lamberg-Allardt et al 200129 |
Adults |
5.6 (35.9) (M); 4.7 (35.5) (F) |
|||||||||
McKenna 199228 |
Adults |
2.5 (1.3) |
|||||||||
Pascoe et al 20012 |
Females |
1.2 (median) |
|||||||||
Morabia et al 200032 |
Females |
2.39 (median) |
|||||||||
Lamberg-Allardt 198427 |
Children/adolescents |
2.5–5.0 (range) |
|||||||||
ANZFA26 |
Children |
1.2–2.2 (range of median values) |
|||||||||
Lethonen-Veromaa et al 199923 |
Children |
2.9–4.3 (range) |
|||||||||
Fortified margarine plus breakfast cereals |
|||||||||||
Gregory et al 199024 |
Adults |
3.4 (3.8) (M); 2.5 (3.1) (F) |
|||||||||
Finch et al 199830 |
Adults > 65 years |
4.1 (4.6) (M); 2.9 (3.4) (F) |
|||||||||
Fortified milk and margarine |
|||||||||||
McKenna 199228 |
Adults |
5.2 (2.0) |
|||||||||
Fortified milk and margarine plus other products |
|||||||||||
McKenna 199228 |
Adults |
6.2 (2.4) |
|||||||||
Foote et al 200031 |
Adults > 71 years |
5.9 (4.2) (M); 5.0 (4.0) (F) |
|||||||||
Lee et al 200233 |
Adults (long-term care) |
6.4 (2.3) (M); 4.7 (2.2) (F) |
|||||||||
Kinyamu et al 199825 |
Females (osteoporotic) |
3.53 (2.2) |
|||||||||
* Baghurst K, Record S (CSIRO National Dietary Survey of 1998–99), personal communication (October 2001). ANZFA = Australia New Zealand Food Authority. M = males, F = females. |
|||||||||||
- Caryl A Nowson1
- Claire Margerison2
- School of Health Sciences, Deakin University, Burwood, VIC.
This article summarises information in our report Vitamin D status of Australians: impact of changes to mandatory fortification of margarine with vitamin D, which was commissioned by the Australia New Zealand Food Authority (ANZFA) and is available from ANFZA. We would like to thank Janine Lewis, ANZFA, for her invaluable comments and assistance in editing this article.
None identified.
- 1. National Health and Medical Research Council. Recommended dietary intakes for use in Australia. Canberra: AGPS, 1991.
- 2. Pascoe J, Henry, M, Nicholson G, et al. Vitamin D status of women in the Geelong Osteoporosis Study: association with diet and casual exposure to sunlight. Med J Aust 2001; 175: 401-405.
- 3. Majid Molla A, Badawi M, al-Yashi S, et al. Risk factors for nutritional rickets among children in Kuwait. Pediatr Int 2000; 42: 280-284.
- 4. Welch T, Bergstrom W, Tsang R. Vitamin D-deficient rickets: the re-emergence of a once conquered disease. J Pediatr 2000; 137: 143-145.
- 5. Shah M, Salhab N, Patterson D, et al. Nutritional rickets still afflict children in north Texas. Tex Med 2000; 96: 64-68.
- 6. Heaney R. Lessons for nutritional science from vitamin D. Am J Clin Nutr 1999; 69: 825-826.
- 7. Heaney R. Vitamin D: how much do we need, and how much is too much? Osteoporos Int 2000; 11: 553-555.
- 8. Sanders K, Nicholson G, Ugoni A, et al. Health burden of hip and other fractures in Australia beyond 2000. Projections based on the Geelong Osteoporosis Study. Med J Aust 1999; 170: 467-470. <eMJA full text>
- 9. Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med. 1992; 327: 1637-1642.
- 10. Mellanby E. Accessory food factors (vitamins) in the feeding of infants. Lancet 1920; 1: 856-862.
- 11. Norman A. Intestinal calcium absorption: a vitamin D-hormone-mediated adaptive response. Am J Clin Nutr 1990; 51: 290-300.
- 12. Brown A, Dusso A, Slatopolsky E. Vitamin D. Am J Phys 1999; 277: F157-F175.
- 13. Kim J, Moon S. Time spent outdoors and seasonal variation in serum concentration of 25-hydroxyvitamin D in Korean women. Int J Food Sci 2000; 51: 439-451.
- 14. Grover S, Morley R. Vitamin D deficiency in veiled or dark-skinned pregnant women. Med J Aust 2001; 175: 251-252. <eMJA full text>
- 15. Nozza J, Rodda C. Vitamin D deficiency in mothers of infants with rickets. Med J Aust 2001; 175: 253-255. <eMJA full text>
- 16. MacGrath J, Kimlin M, Saha S, et al. Vitamin D insufficiency in south-east Queensland. Med J Aust 2001; 174: 150-151.
- 17. Stein M. Falls relate to vitamin D and parathyroid hormone in Australian nursing homes and hostels. J Am Geriatr Soc 1999; 47: 1265-1266.
- 18. Nowson C, MacInnis R, Stein M, et al. Vitamin D deficiency in residential care facilities in Australia. Proc Nut Soc Aust 2000; 24: 154 (abstract).
- 19. Glerup H, Mikkelsen K, Poulsen L, et al. Commonly recommended daily intake of vitamin D is not sufficient if sunlight exposure is limited. J Intern Med 2000; 247: 260-268.
- 20. Holick M. Sunlight "D"ilemma: risk of skin cancer or bone disease and muscle weakness. Lancet 2001; 357: 4-6.
- 21. Food and Nutrition Board. Dietary reference intakes for Ca, P, Mg, vitamin D and F. Washington: National Academy Press, 1997.
- 22. Utiger RD. The need for more vitamin D [editorial; comment]. N Engl J Med 1998; 338: 828-829.
- 23. Lethonen-Veromaa M, Mottonen T, Irjala K, et al. Vitamin D intake is low and hypovitaminosis D common in healthy 9- to 15-year old Finnish girls. Eur J Clin Nutr 1999; 53: 746-751.
- 24. Gregory J, Foster K, Tyler H, Wiseman M. The Dietary and Nutritional Survey of British Adults. London: HMSO, 1990.
- 25. Kinyamu HK, Gallagher JC, Rafferty KA, et al. Dietary calcium and vitamin D intake in elderly women: effect on serum parathyroid hormone and vitamin D metabolites. Am J Clin Nutr 1998; 67: 342-348.
- 26. Australia New Zealand Food Authority (ANZFA). Review of vitamins and minerals standard. Canberra: ANZFA ,1999, Proposal 16.6.
- 27. Lamberg-Allardt C. Vitamin D intake, sunlight exposure and 25-hydroxyvitamin D levels in the elderly during one year. Ann Nutr Metab 1984; 28: 144-150.
- 28. McKenna M. Differences in vitamin D levels between countries in young adults and the elderly. Am J Med 1992; 93: 69-77.
- 29. Lamberg-Allardt CJ, Outila TA, Karkkainen MU, et al. Vitamin D deficiency and bone health in healthy adults in Finland: could this be a concern in other parts of Europe? J Bone Miner Res 2001; 16: 2066-2073.
- 30. Finch S, Doyle W, Lowe C, et al. National Diet and Nutrition Survey: people aged 65 years and over. Vol 1: Report of the Diet and Nutrition Survey. London: TSO, 1998.
- 31. Foote J, Giuliano A, Harris R. Older adults need guidance to meet nutritional recommendations. J Am Coll Nutr 2000; 19: 628-640.
- 32. Morabia A, Bernstein M, Antonini S. Smoking, dietary calcium and vitamin D deficiency in women: a population-based study. Eur J Clin Nutr 2000; 54: 684-689.
- 33. Lee L, Drake W, Kendler D. Intake of calcium and vitamin D in three Canadian long-term facilities. J Am Diet Assoc 2002; 102: 244-247.
- 34. Compston JE. Vitamin D deficiency: time for action. Evidence supports routine supplementation for elderly people and others at risk [editorial]. BMJ 1998; 317: 1466-1467.
- 35. Keane EM, Healy M, O'Moore R, et al. Vitamin D-fortified liquid milk: benefits for the elderly community-based population. Calcif Tissue Int 1998; 62: 300-302.
- 36. Scragg R, Khaw K, Murphy S. Life-style factors associated with winter serum 25-hydroxyvitamin D levels in elderly adults. Age Ageing 1995; 24: 271-275.
- 37. Rasmussen LB, Hansen GL, Hansen E, et al. Vitamin D: should the supply in the Danish population be increased? Int J Food Sci Nutr 2000; 51: 209-215.





Abstract
The main source of vitamin D for Australians is exposure to sunlight. Thus, levels of serum 25-hydroxyvitamin D3, the indicator of vitamin D status, vary according to the season and are lower at the end of winter.
In Australia and New Zealand, the prevalence of vitamin D deficiency varies, but is acknowledged to be much higher than previously thought. One study found marginal deficiency in 23% of women, and another frank deficiency in 80% of dark-skinned and veiled women. The groups at greatest risk of vitamin D deficiency in Australia are dark-skinned and veiled women (particularly in pregnancy), their infants, and older persons living in residential care.
Only a few foods (eg, fish with a high fat content) contain significant amounts of vitamin D. In Australia, margarine and some milk and milk products are currently fortified with vitamin D.
The average estimated dietary intake of vitamin D for men is 2.6–3.0 µg/day and for women is 2.0–2.2 µg/day. The estimated dietary requirement of vitamin D is at least 5.0 µg/day and may be higher for older people.
Adequate intake of vitamin D is unlikely to be achieved through dietary means, particularly in the groups at greatest risk, although vitamin D-fortified foods may assist in maintaining vitamin D status in the general population.
An appropriate health message for vitamin D needs to balance the need for sunshine against the risk of skin cancer.