The effectiveness of clinical quality registries (registries) to monitor and benchmark patient outcomes is well established.1-3 There is also compelling evidence for the ability of registry information to drive continuous improvements in patient outcomes and adherence to guideline-recommended care.2-5 Systematic and ongoing collection of standardised data on medical and surgical interventions allows the identification and analysis of clinical practice variation and its effect on patient outcomes. Registry data has credibility with clinicians, stimulating increased use of evidence-based clinical management, decreased variation in care and improved patient outcomes.2,4
Capturing a high proportion of a registry’s eligible patient population is critically important in minimising the selection bias associated with incomplete capture. A low capture rate renders the pool of results unrepresentative and ungeneralisable, thus weakening the power of a registry to inform policy determinations.3 Omissions of data within a single clinical unit create the potential for “manipulation” of included and excluded data, thus weakening the credibility of unit-level reports and their ability to drive change.
Current reporting in Australia
A small number of national registries in Australia now capture a high proportion of their eligible patient populations. These include the Australia and New Zealand Dialysis and Transplant Registry,6 the Australian Orthopaedic Association National Joint Replacement Registry,7 the adult and paediatric registries run by the Australian and New Zealand Intensive Care Society,8 the Australasian Rehabilitation Outcomes Centre9 and the Palliative Care Outcomes Collaboration.10
Examples of how these registries report on rates of appropriate or recommended care include reports from the Australia and New Zealand Dialysis and Transplant Registry, which show improvement in the preferred type of vascular access — arteriovenous fistula — for haemodialysis patients over the period 2008 to 2012 (Box 1).11
The extent of adherence to guideline-recommended care delivered in intensive care units (ICUs) across Australia is demonstrated by information provided by the Adult Patient Database8 of the Australian and New Zealand Intensive Care Society’s Centre for Outcome and Resource Evaluation. Box 2 shows the high proportion of ICU admissions for which the patient received guideline-recommended care for venous thromboembolism prophylaxis each year for 5 years.8
Data from the Australasian Rehabilitation Outcomes Centre (AROC) demonstrate improvements in a key process indicator — assessment of functional status — for rehabilitation care provided in Australian hospitals over the period from 2002, when the Centre opened, to 2015 (unpublished data provided by AROC, July 2016) (Box 3).
The Palliative Care Outcomes Collaboration (PCOC) collects data from palliative care services across Australia on the length of time palliative care patients spend in the unstable phase of illness. An unstable phase ends when a new plan of care is in place, has been reviewed, and no further changes are required. A patient is considered to have an acceptable outcome if they experience no more than 3 days of instability. Information reported by the PCOC shows a considerable improvement in palliative care services achieving this benchmark over the period 2010–2015 (unpublished data provided by PCOC, July 2016). For care provided in hospital, the proportion of patients spending no more than 3 days in the unstable phase increased from 57% in 2010 to 86% in 2015. Similarly, for patients receiving care at home, the proportion increased from 41% to 76% (Box 4).
Governments across Australia have developed a number of registries with a jurisdictional focus. The Victorian Department of Health and Human Services, in particular, has invested in a significant number of clinical quality registries. In some instances, substantial funding has been made available by other organisations such as the Victorian Transport Accident Commission, Medibank Private and the Movember Foundation. Some state-based registries such as the Victorian Cardiac Outcomes Registry and its counterparts in South Australia, Queensland and New South Wales are collaborating to develop nationally consistent datasets.
There remains, however, limited capacity across Australia to benchmark outcomes and assess the degree with which health care aligns with evidence-based practice in a number of high priority clinical domains. In 2011, Evans and colleagues conducted a national survey to determine the capacity of Australian clinical registries to accurately assess quality of care. Of 28 registries surveyed, the majority were found to require modifications to provide useful and reliable information for quality improvement purposes. Thirteen of the 28 registries (46%) recruited fewer than 80% of the eligible population. Twenty-three surveyed registries (82%) did not formally audit reliability of coding at the clinical level and five (18%) did not collect the information required for basic risk adjustment of outcome measures.12
In a 2010 systematic review of how medical registries provide information feedback to health care providers, van der Veer and colleagues confirmed findings from previous studies that process of care measures — such as adherence to guideline-recommended treatment or treatment modality, time to treatment, and use of secondary prevention medication — are more readily influenced by feedback than by outcome measures.13 However, national measurement of health care appropriateness (as measured by how closely care aligns with guidelines) in some important clinical domains such as acute coronary syndrome and stroke care has relied on intensive periods of clinical audit.14,15 This could be monitored more effectively using registries, which routinely collect a minimum dataset. Well constructed registries collect and report information on both the effectiveness of care (outcomes) and the appropriateness of care (process) on an ongoing basis, obviating the requirement for clinical audit.3,16,17
Some Australian registries are developing to the point where national auditing of clinical care will no longer be required in order to gain an accurate picture of national outcomes and patterns of care. The Australian Cardiac Outcomes Registry18 intends to develop its collection of outcomes data for patients with acute coronary syndrome along with processes of care data in line with the Guidelines for the management of acute coronary syndromes 2006.19 The recently launched Australian and New Zealand Hip Fracture Registry20 has commenced collecting data items on both effectiveness and appropriateness of care in line with the Australian and New Zealand guideline for hip fracture.21 The Australian Stroke Clinical Registry22,23 collects and reports information on the outcomes of care for stroke patients and information on processes of care in accordance with the Clinical guidelines for stroke management 2010.24 For example, Box 5 shows participating adult hospitals’ adherence to five guideline-recommended process of care indicators.
Registry reporting outside Australia
In the United Kingdom, the National Hip Fracture Database (NHFD) was developed as a collaboration between the British Orthopaedic Association (BOA) and the British Geriatrics Society (BGS). Data are collected on casemix, care processes and patient outcomes.25 Care is measured against six standards laid out in the 2007 Blue Book (clinical care standards) on the care of fragility fracture patients, including prompt admission to orthopaedic care; surgery within 48 hours and within normal working hours; nursing care aimed at minimising pressure ulcer incidence; routine access to orthogeriatric medical care; assessment and appropriate treatment to promote bone health; and falls assessment.26 In 2010, the NHFD registry became a ready-made data collection and reporting mechanism for measuring compliance with a set of clinical care standards incentivised by a best practice tariff.27 Box 6 shows the compliance with best practice for a number of clinical care standards using registry data.
The authors of the 2012 NHFD national report note:
clinical teams have used the synergy of audit, feedback and standards locally in clinical change or service development initiatives prompted and monitored by the NHFD, often with very substantial and quantifiable improvements. These include reduced mortality and reductions in length of stay, often arising from care pathway redesign and improved collaboration between surgeons, anaesthetists and ortho-geriatricians; and substantial efficiency savings that are in keeping with an important point made in the BOA/BGS Blue Book: “Looking after hip fracture patients well is cheaper than looking after them badly”.25
In the United States, the American Heart Association/American Stroke Association Stroke registry has been successful in measuring adherence to a number of agreed care processes, including deep vein thrombosis prophylaxis, antithrombotic therapy, discharge medication, dysphagia screening, stroke education, smoking cessation and assessment for rehabilitation.28 The registry has over two million patients enrolled from more than 2000 hospitals and links performance data with Medicare fee-for-service claims data. This has enabled the creation of 30-day and 1-year mortality prediction models, outcomes variation comparison across hospitals and the assessment of the impact of critical variables on outcomes of interest.28
Heart failure registries in the US collect data on clinical characteristics, patterns of hospital and outpatient care, as well as outcomes of patients admitted with this condition.4 Online tools are used to provide personally tailored feedback on performance and other quality measures against a national benchmark. Process of care improvement tools have been developed and made available in a toolkit, which includes evidence-based practice algorithms, critical pathways, standardised orders, discharge checklists, pocket cards, and chart stickers. The toolkit also includes algorithms and dosing guides for guideline-recommended therapies and a comprehensive set of patient education materials. Participation in heart failure registries in the US has been associated with substantial improvements in the use of guideline-recommended therapies for heart failure in both the inpatient and outpatient settings.4 Conformity with appropriateness measures has been shown to improve patient outcomes and disparities in care have been reduced or eliminated.4
Swedish registries have contributed to a vast amount of information used in health services research in that country.29 Many of the Swedish registries commenced operations over 20 years ago with government financial support and have been attentively maintained. Incentives are provided to hospitals complying with routine contributions to the registries. Required datasets are succinct, thereby minimising data entry burden. This has produced high participation rates which are closely representative of the eligible population. In return hospitals and clinicians are provided with high quality reports which are up to date and risk adjusted.30
Opportunities that registries provide
Well designed and managed clinical registries provide clinical information which is richer, more reliable and more credible than information generated from hospital administrative systems.31 Analyses based on clinical data are respected by clinicians and patients. A comparative review by Cohen in 2014 demonstrated that the Cardiac Care Network Registry in Ontario, Canada, provides relevant clinical details with greater accuracy when compared with administrative databases.32 Data from the registry were found to be more robust for informing best practice cardiac clinical care pathways and evidence-based cardiac procedures. Information provided by registries therefore enjoys a high level of trust by clinicians, health managers, governments, private hospital groups and funding bodies.
The use of registries to monitor health care quality and safety is supported by patients. Analyses show that as long as appropriate measures are taken to ensure data security and confidentiality, the majority of patients acknowledge the value of registries and the necessity to collect identifying data, and accept the requirement for registries to operate under opt-out consent with scope for linkage to other datasets.33
The purpose and scope of patient registries are expanding. Aside from the principal function of monitoring and benchmarking the appropriateness and effectiveness of clinical care, registries can provide the foundation for opportunities to undertake evidence-based health care reform. The potential for articulation with best practice pricing incentive schemes has been highlighted above. Registries also provide a way of generating an early warning of lowered outcomes and a means to share learnings from high performing units, such as those with lower infection rates. Examples of other opportunities provided by registries include clinician and facility performance assessment and credentialing; greater accountability and transparency through public reporting; performance-based reimbursement; value-based purchasing; the development of evidence-based practice guidelines; enhanced post-market surveillance of medical devices and pharmaceuticals; monitoring trends in utilisation and access to care; supporting cost-effectiveness studies; and the provision of infrastructure with which to conduct clinical trials and comparative effectiveness studies.5,29,34
Patient-reported outcome measures (PROMs) are increasingly being introduced into registries,35 providing a personal perspective on the expectations and impact of surgery. For example, the Victorian Severe Trauma Registry and the Victorian Prostate Cancer Registry both collect and report PROMs at a time of clinical stability. The Arthroplasty Clinical Outcomes Registry in NSW reports pre- and post-operative PROMs, and health-related quality of life, for primary and revision procedures (Box 7).36 In the UK, the National Health Service requires the routine measurement of PROMs for all patients undergoing total knee or hip arthroplasty (http://content.digital.nhs.uk/proms). In Sweden, almost all units performing total hip arthroplasty are administering PROMs before and after surgery.37 The respective registries in those countries collect and report such data.
There is increasing evidence that registries demonstrate good value for money, that is, improved health outcomes at lower cost.38-40 In 2012, Larsson and colleagues calculated that if the US had a registry for hip replacement surgery that encouraged reductions in surgical revision rates comparable with those attributed, in part, to the presence of the Swedish registry, the US might have avoided $2 billion of an expected $24 billion in total costs in 2015 for these surgeries.39
Barriers to effective reporting
Barriers to registry development are well documented.41-45 Adequate funding is a problem that registries share with many other health care initiatives. Funding aside, the principal barriers to the development of clinical quality registries in Australia are:
reluctance of some health care providers and organisations to supply source data;
poor interoperability between clinical information systems leading to unnecessary duplication of data entry;
limited availability of the skills (clinical, epidemiological, biostatistical) and resources (advanced and secure data systems) to run national registries; and
data governance burdens and constraints, including restrictions on the disclosure, collection, linkage and reporting of patient level data.
Notwithstanding successful efforts to develop new registries20 and improve established registries, these barriers persist for clinical groups and registry experts wishing to improve the quality of information and level of participation in registries in Australia.
Beyond the barriers
To address these barriers, the Australian Commission on Safety and Quality in Health Care worked with jurisdictional representatives and registry experts to develop a framework detailing national arrangements under which patient level data may be routinely and securely disclosed, collected, analysed and reported. The Framework for Australian clinical quality registries46 (endorsed by the Australian Health Ministers’ Advisory Council in March 2014) describes a mechanism by which government jurisdictions and private hospital groups can authorise and secure record-level data, within high priority clinical domains, to measure, monitor and report the appropriateness and effectiveness of health care. Application of the Framework to registries provides assurances to jurisdictions, private hospital groups, clinicians and patients, that registry data and the systems that hold those data have satisfied minimum security, technical and operating standards.
The establishment of a number of national clinical quality registries for high burden, high variance conditions or interventions is a cost-effective38-40 way of addressing Australia’s information gaps in order to effectively monitor the appropriateness and effectiveness of health care. The development of one national registry per clinical domain — rather than multiple state and territory-based registries all attempting to monitor similar indicators — has obvious efficiencies and is more likely to attract funding. Well designed registries are an increasingly important component of clinical practice47 and health system monitoring. The provision of timely, relevant and reliable feedback about patient care to clinicians drives improvements in health care quality. Improved reporting of registry information on the appropriateness of care is likely to improve adherence to evidence-based practice.
Box 1 – Vascular access type at initial treatment, by time to referral for haemodialysis in Australia, 2008–2012
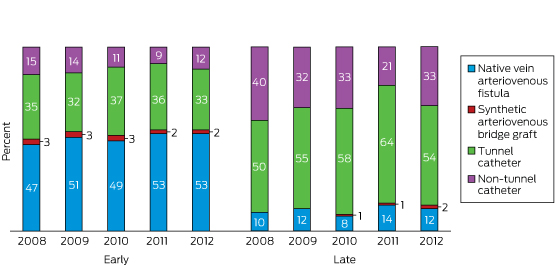
Source: reproduced with permission from ANZDATA Annual Report 2013, Ch 5: Haemodialysis, Fig 5.75.11
Box 2 – Proportion of admissions in which venous thromboembolism prophylaxis was administered to eligible patients within 24 hours of admission to an intensive care unit, 2010–11 to 2014–15
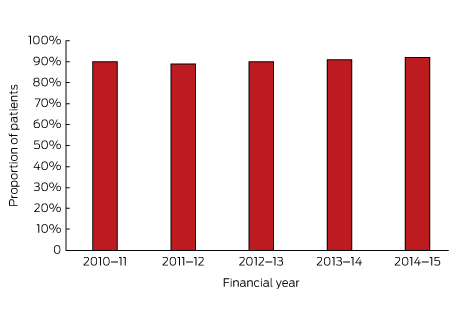
Source: data provided by the Australian and New Zealand Intensive Care Society, July 2016.
Box 3 – Proportion of patients assessed for functional status (activities of daily living) within three days of admission to a hospital rehabilitation ward, 2002–2015
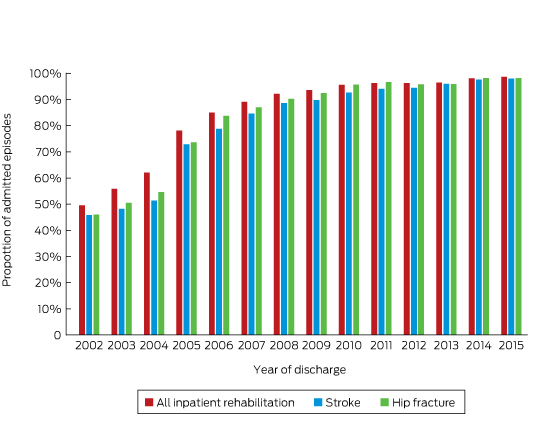
Source: data provided by the Australasian Rehabilitation Outcomes Centre, Australian Health Services Research Institute, University of Wollongong, July 2016.
Box 4 – Proportion of patients in the unstable phase with an effective care plan implemented in 3 days or less
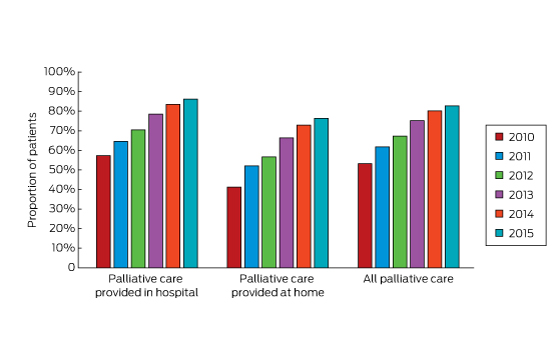
Source: data provided by the Palliative Care Outcomes Collaboration, Australian Health Services Research Institute, University of Wollongong, July 2016.
Box 5 – Hospital adherence to process indicators for stroke care
Hospital stroke care |
All episodes |
Ischaemic |
TIA |
||||||||||||
Patients admitted to a stroke unit |
5847/7608 (77%) |
3904/4583 (85%) |
992/1489 (67%) |
||||||||||||
Patients who received intravenous thrombolysis (tPA) of an ischaemic stroke |
na |
476/4583 (10%) |
na |
||||||||||||
Patients discharged (not deceased while in hospital) |
6744/7400 (91%) |
4115/4481 (92%) |
1470/1474 (99.7%) |
||||||||||||
Patient discharged on an antihypertensive (if not deceased while in hospital) |
4661/6555 (71%) |
3044/4027 (76%) |
969/1440 (67%) |
||||||||||||
Patients who received a care plan at discharge (if discharged home or to RACF) |
2046/3713 (55%) |
1122/1996 (56%) |
651/1289 (51%) |
||||||||||||
Source: Australian Stroke Clinical Registry Annual Report 2013, Table 7, p.29.22 na = not applicable. RACF = residential aged care facility. TIA = transient ischaemic attack. tPA = tissue plasminogen activator. Unknowns coded as no; inpatient death determined using National Death Index data. | |||||||||||||||
Box 6 – Compliance with best practice standards for hip fracture patients in the United Kingdom, 2009–2012
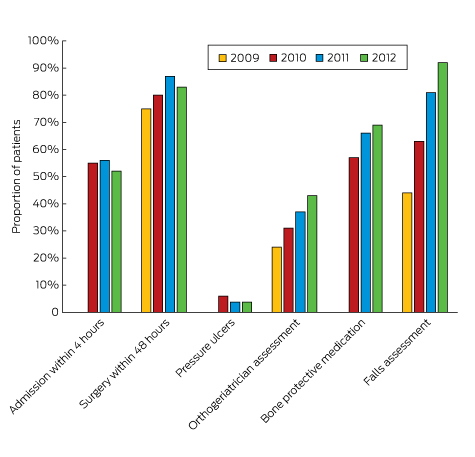
Source: prepared with permission from data in the National Hip Fracture Database National Report 2012 – Supplement, Table 1.25
Box 7 – Pre- and post-operative patient-reported outcome measures (Oxford Hip Scores [OHS]) for hip arthroplasty — all hospitals, 2013
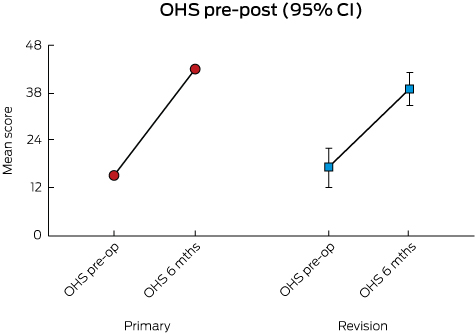
Source: reproduced with permission from Arthroplasty Clinical Outcomes Registry, 2013 Annual Report, Fig 7.1.36
Provenance: Commissioned; externally peer reviewed.
- Nick Wilcox1
- John J McNeil2
- 1 Australian Commission on Safety and Quality in Health Care, Sydney, NSW
- 2 Monash University, Melbourne, VIC
No relevant disclosures.
- 1. Liu FX, Rutherford P, Smoyer-Tomic K, et al. A global overview of renal registries: a systematic review. BMC Nephrol 2015; 16: 31.
- 2. Stey AM, Russell MM, Ko CY, et al. Clinical registries and quality measurement in surgery: a systematic review. Surgery 2015; 157: 381-395.
- 3. Gliklich R, Dreyer N, Leavy M, editors. Registries for evaluating patient outcomes: a user’s guide. 3rd edition. Two volumes. Rockville, MD: Agency for Healthcare Research and Quality, 2014.
- 4. Fonarow GC. Improving quality of care and outcomes for heart failure: role of registries. Circ J 2011; 75: 1783-1790.
- 5. Ashrafi R, Hussain H, Brisk R, et al. Clinical disease registries in acute myocardial infarction. World J Cardiol 2014; 6: 415-423.
- 6. McDonald SP, Russ GR. Australian registries — ANZDATA and ANZOD. Transplant Rev (Orlando) 2013; 27: 46-49.
- 7. Australian Orthopaedic Association National Joint Replacement Registry. Annual report. Adelaide: AOA, 2014.
- 8. Australian and New Zealand Intensive Care Society. ANZICS CORE annual report 2014-15. Melbourne: ANZICS, 2016. http://www.anzics.com.au/Downloads/ANZICS%20CORE%20Annual%20Report%202015.pdf (accessed Oct 2016).
- 9. Australian Health Services Research Institute. Australasian Rehabilitation Outcomes Centre. University of Wollongong. http://ahsri.uow.edu.au/aroc/index.html (accessed Oct 2016).
- 10. Australian Health Services Research Institute. Palliative Care Outcomes Collaboration. University of Wollongong. http://ahsri.uow.edu.au/pcoc/index.html (accessed Oct 2016).
- 11. Australia and New Zealand Dialysis and Transplant Registry (ANZDATA). Annual Report 2013. Chapter 5: Haemodialysis. Figure 5.75. http://www.anzdata.org.au/anzdata/AnzdataReport/36thReport/2013c05_haemodialysis_v1.7.pdf (accessed July 2016).
- 12. Evans SM, Bohensky M, Cameron PA, McNeil J. A survey of Australian clinical registries: can quality of care be measured? Intern Med J 2011; 41: 42-48.
- 13. van der Veer SN, de Keizer NF, Ravelli ACJ, et al. Improving quality of care. A systematic review on how medical registries provide information feedback to health care providers. Int J Med Inform 2010; 79: 305-323.
- 14. Chew DP, French J, Briffa TG, et al. Acute coronary syndrome care across Australia and New Zealand: the SNAPSHOT ACS study. Med J Aust 2013; 199: 185-191. <MJA full text>
- 15. National Stroke Foundation. National Stroke Audit: Acute Services. Clinical audit report 2013. Melbourne: NSF, 2013.
- 16. Australian Commission on Safety and Quality in Health Care. Operating principles for Australian clinical quality registries. Sydney: ACSQHC, 2010.
- 17. McNeil JJ, Evans SM, Johnson NP, Cameron PA. Clinical-quality registries: their role in quality improvement. Med J Aust 2010; 192: 244-245. <MJA full text>
- 18. Cardiac Society of Australia and New Zealand. Australian Cardiac Outcomes Registry. http://acor.net.au (accessed Oct 2016).
- 19. Acute Coronary Syndrome Guidelines Working Group. Guidelines for the management of acute coronary syndromes 2006. Med J Aust 2006; 184 (8 Suppl): S1-S32. <MJA full text>
- 20. ANZ Hip Fracture Registry. Enhancing outcomes for older people. ANZHFR Newsletter, Issue 3, March 2013.
- 21. Australian and New Zealand Hip Fracture Registry (ANZHFR) Steering Group. Australian and New Zealand Guideline for Hip Fracture Care - Improving outcomes in hip fracture management of adults. Sydney: ANZHFR Steering Group, 2014.
- 22. Cadilhac DA, Lannin NA, Anderson CS, et al; on behalf of the AuSCR Consortium. The Australian Stroke Clinical Registry Annual Report 2013. Florey Institute of Neuroscience and Mental Health; November 2014, Report No 5. http://www.auscr.com.au/wp-content/uploads/AuSCR-AnnualReport-2013-FINAL.pdf (accessed Oct 2016).
- 23. Middleton S, Coughlan K, Mnatzaganian G, et al. Feasibility of long term follow-up of quality in acute stroke care trial participants: an evaluation of data linkage from state and national death registries. Int J Stroke 2014; 9: 44-45.
- 24. National Stroke Foundation. Clinical guidelines for stroke management 2010. Melbourne: NSF, 2010.
- 25. National Hip Fracture Database. The National Hip Fracture Database national report 2012 – Supplement. http://www.nhfd.co.uk/20/hipfractureR.nsf/vwcontent/2012ReportDownload/$File/NHFDSupplement2012.pdf?openelement (accessed Oct 2016).
- 26. British Orthopaedic Association and British Geriatrics Society. The care of patients with fragility fracture (Blue Book). British Orthopaedic Association, 2007.
- 27. Department of Health Payment by Results Team. A simple guide to payment by results. National Health Service, United Kingdom. November 2012. https://www.gov.uk/government/publications/simple-guide-to-payment-by-results (accessed Oct 2016).
- 28. Schwamm LH. Measuring and changing the quality of care via national registries. Stroke 2013; 44: S132-S135.
- 29. Tavazzi L. Do we need clinical registries? Eur Heart J 2014; 35: 7-9.
- 30. Swedish HealthCare. Improved results in healthcare using quality registries. June 2013. http://www.swedishhealthcare.com/improved-results-in-healthcare-using-quality-registries (accessed Oct 2016).
- 31. McCoy RG, Tulledge-Scheitel SM, Naessens JM, et al. The method for performance measurement matters: Implications of transitioning from administrative claims to registries. Diabetes 2014; 63: A5.
- 32. Cohen E, Peterson B, Braga V, et al. Evidence for utility of clinical registries to support development of cardiac QBPs and clinical care pathways. Can J Cardiol 2014; 30 Suppl: S134.
- 33. Donohue F. Patient opinions of patient registries. Irish J Med Sci 2012; 181: S127.
- 34. Jain HS, Conway PH, Berwick DM. A public-private strategy to advance the use of clinical registries. J Am Soc Anesthesiol 2012; 117: 227-229.
- 35. Gemmen E, Leavy MB. Collecting PROs in patient registries: the need for and potential impact of providing pro data to the treating physician-and when. Value Health 2014; 17: A207.
- 36. Arthroplasty Clinical Outcomes Registry. 2013 annual report. Sydney, ACORN, 2014. http://www.acornregistry.org/images/ACORN%20Annual%20Report%202013.pdf (accessed Oct 2016).
- 37. Paulsen A. Patient reported outcomes in hip arthroplasty registries. Dan Med J 2014; 61.
- 38. Walters SR. Demonstrating value: registries and beyond. Gastrointest Endosc Clin North Am 2012; 22: 135-145.
- 39. Larsson S, Lawyer P, Garellick G, et al. Use of 13 disease registries in 5 countries demonstrates the potential to use outcome data to improve health care’s value. Health Aff (Millwood) 2012; 31: 220-227.
- 40. Ryan TJ. Large cardiac registries: the path to higher quality and lower cost in our healthcare system. Circulation 2010; 121: 2612-2614.
- 41. Gliklich RE, Karl J, Leavy MB, et al. Challenges in developing an outcome measures framework for patient registries. Value Health 2013; 16: A265.
- 42. Hogan DB, Warner J, Patten S, et al. Ethical and legal considerations for Canadian registries. Can J Neurol Sci 2013; 40: S5-S23.
- 43. Evans SM, Loff B, Cameron PA. Clinical registries: the urgent need to address ethical hurdles. Med J Aust 2013; 198: 134-135. <MJA full text>
- 44. Hickey GL, Grant SW, Cosgriff R, et al. Clinical registries: governance, management, analysis and applications. Eur J Cardiothorac Surg 2013; 44: 605-614.
- 45. Evans SM, Scott IA, Johnson NP, et al. Development of clinical-quality registries in Australia: the way forward. Med J Aust 2011; 194: 360-363. <MJA full text>
- 46. Australian Commission on Safety and Quality in Health Care. Framework for Australian clinical quality registries. Sydney, Australia: ACSQHC, 2014.
- 47. Brieger D, Aliprandi-Costa B. Developments in procedural and disease registries: a focus on coronary artery disease. Curr Opin Cardiol 2013; 28: 405-410.





Summary