This is the first reported case of eye injury caused by a crayfish antenna. A 20-year-old male crayfish diver sustained a scleral penetrating injury that led to a subconjunctival abscess. The foreign body was histologically similar to a crayfish antenna.
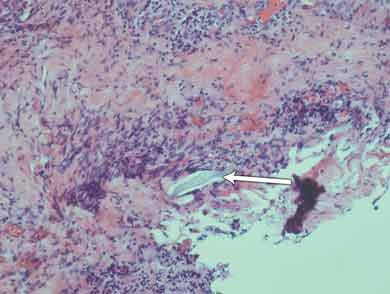
Histological results of the initial surgical specimen showed a small foreign body several microns in length intimately associated with deeply placed active inflammation (Box 1). There was fibroproliferative activity and an infiltrate of inflammatory cells; these were associated with tissue necrosis and microabscess formation. Culture of a preoperative conjunctival swab was negative for microbial growth.
The original foreign body extracted during surgery was compared with a specimen of crayfish antennae and was found to be similar to the very outer layer (1–2 μm) of the specimen (Box 2). It most likely became lodged while the patient was handling crayfish or cleaning the crayfish tank without eye protection, which he was doing extensively during the morning that the red eye developed. The crayfish caught in this area are of several different types, although the Panulirus ornatus (tropical rock lobster) make up 95% of the local population.1
A population-based cross-sectional study of eye injuries in Australia found that they were more common among men, people living in rural areas and tradespeople, and that the workplace was the most common location where the injury occurred.2 A review of 109 penetrated or ruptured globes over 4 years in Adelaide identified that 80% of patients were men; the most common cause of injury was hammering metal; and the final visual acuity was 6/12 or better in 40% of patients, and no perception of light in 26%.3 Another group found that of 6308 patients treated at their hospital over 12 months, 6% were admitted for severe ocular trauma and most of these were young men.4
Workplace-related injuries accounted for 44% of all ocular injuries and 19% of cases of severe eye trauma.4 The annual medical costs for eye injuries have been estimated at $155 million for the projected 116 000 cases nationwide.4 In 2006, a review of ocular trauma over 7 years at Cairns Base Hospital estimated the incidence of open globe injuries to be 3.7 per 100 000 population.5 An international study of PEIs in rural areas found that 16% were work-related.6 Most injuries were related to maintenance or repair work, wood chopping or machine use. A small number were the result of cow butting. At the final review, 64% of these eyes were blind.6
Crayfish antenna penetration is a mechanism that has not previously been reported. Thorns of plants have been previously reported to cause PEIs in children, but the most common aquatic-related PEI is with fish hooks.7,8 Appropriate preventive measures, such as use of protective eyewear and implementation of education programs, could be effective in decreasing the incidence of these aquatic-related ocular traumas.
- 1. Fisheries of Queensland’s East Coast CRC Reef Research Centre. Tropical rock lobster. 2005. http://www.reef.crc.org.au/research/fishing_fisheries/statusfisheries/harvestlobster.htm (accessed Nov 2011).
- 2. McCarty CA, Fu CL, Taylor HR. Epidemiology of ocular trauma in Australia. Ophthalmology 1999; 106: 1847-1852.
- 3. Casson RJ, Walker JC, Newland HS. Four-year review of open eye injuries at the Royal Adelaide Hospital. Clin Experiment Ophthalmol 2002; 30: 15-18.
- 4. Fong LP. Eye injuries in Victoria, Australia. Med J Aust 1995; 162: 64-68.
- 5. Smith AR, O’Hagan SB, Gole GA. Epidemiology of open and closed globe trauma presenting to Cairns Base Hospital, Queensland. Clin Experiment Ophthalmol 2006; 34: 252-259.
- 6. Mackiewicz J, Machowicz-Matejko E, Saaga-Pylak M, et al. Work-related, penetrating eye injuries in rural environments. Ann Agric Environ Med 2005; 12: 27-29.
- 7. Blomdahl S, Norell S. Perforating eye injury in the Stockholm population. An epidemiological study. Acta Ophthalmol (Copenh) 1984; 62: 378-390.
- 8. Knox FA, Chan WC, McAvoy CE, et al. Penetrating ocular injuries from fish-hooks. Int Ophthalmol 2004; 25: 291-294.






No relevant disclosures.