Abbreviations used in text
ED |
Emergency department |
ViCCU |
Virtual Critical Care Unit |
BMH |
Blue Mountains District ANZAC Memorial Hospital |
NH |
Nepean Hospital |
ICU |
Intensive care unit |
AMRS |
Aeromedical and Medical Retrieval Service |
BV |
Before the ViCCU intervention |
AV |
After the ViCCU intervention |
Technological advances have provided new opportunities for the use of telemedicine systems, particularly in time-critical settings such as emergency departments. Systematic reviews1,2 of telemedicine evaluations have demonstrated limited evidence of effectiveness in improving care delivery or patient outcomes compared with existing care. This may be related to a failure of studies to examine these indicators or to the use of poor methods of investigating outcomes. Emergency department (ED) telemedicine studies have rarely featured in systematic reviews of telemedicine applications.1,3 This reflects the significant lack of high-quality evidence of ED telemedicine effectiveness and of when and how systems may be most effectively used.1,2,4 Further, there has been little investigation of their impact on clinicians’ work, particularly in the context of the ED, where communication processes are highly disruptive.5,6
The Virtual Critical Care Unit (ViCCU, a registered trademark of the Commonwealth Scientific and Industrial Research Organisation [CSIRO])7 is a telemedicine system that allows real-time, broadcast-quality, low-latency audiovisual communication between ED clinicians at different sites. This level of high-quality data transfer has not been possible with previous low-bandwidth systems.
The aims of our study were to evaluate whether the ViCCU changed patient management and outcome indicators for acutely ill patients presenting for urgent care at a district ED, and to investigate clinicians’ perceptions of the impact of the ViCCU system on care provided and on their work.
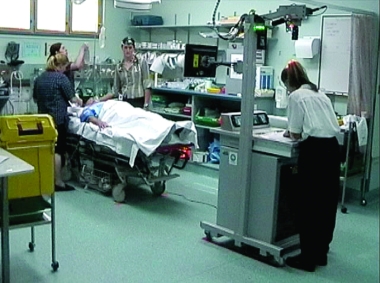
The ViCCU7 uses an ultrabroadband, fibre-optic connection (1000 megabytes of data per second) that allows real-time audiovisual communication between clinicians at BMH and ED specialists at NH. The NH specialist can be heard by the patient and BMH staff and can be seen on a cart monitor (Box 1). The NH specialist can simultaneously view three images of the patient (end of bed, above bed and roving camera), a vital signs monitor and a document camera with x-ray viewing (Box 2).
BMH clinicians were requested to use the ViCCU for all patients presenting with acute illness. Consultations were initiated by telephone to the NH ED physician on duty. Use of the ViCCU system commenced on 1 January 2004.
The before-ViCCU (BV) and after-ViCCU (AV) patient samples consisted of acutely ill patients requiring urgent care, defined as those triaged to category 1 (resuscitation) or specified subcategories of triage category 2 (emergency) (Box 3).8 We calculated that we would need a sample size of 192 presentations (5% significance and 80% power), assuming a 12.5% decrease in hospital admissions after the introduction of the ViCCU. This meant that 12 months of BV and 18 months of AV data were required.
Patients were classified by case type (Box 4). The indicators selected were based on clinical importance, likelihood of influence by the ViCCU, and their availability in routine datasets. Management indicators were changes in disposition (admission, discharge or transfer), treatment time (defined as time spent under clinician supervision at BMH ED), and the number of procedures performed at BMH. Outcome indicators were changes in length of stay at BMH or NH, rapid acute physiology scores and, for patients transferred to NH, hours spent on ventilation or in the NH ICU.
At the end of the study period, 12 months of BV patient data (1 January to 31 December 2003) and 18 months of AV data (1 January 2004 to 30 June 2005) were abstracted. In addition, semi-structured interviews were held with 31 of 33 doctor and nurse clinicians at both hospitals after June 2005. Clinicians were asked: “What impact has the ViCCU had on the way patients are treated in BMH?” and “As an individual, how has the ViCCU impacted on your experience working in the emergency department?”
There were no significant BV–AV differences in the characteristics of presenting patients (Box 5).
Patterns of disposition from BMH ED changed significantly after the ViCCU was introduced. While the overall likelihood of being transferred did not change (38%), the likelihood of admission to BMH fell from 30% to 15%, and the likelihood of discharge increased from 25% to 35% (Box 6). Patterns of disposition for patients with major trauma remained the same, but patients with moderate trauma were less likely to be transferred and more likely to be discharged. Critical care patients were less likely to be admitted to BMH (54% BV v 30% AV) and more likely to be transferred. Critical care and moderate trauma patients who were transferred were more likely to be transferred to hospitals other than NH after the ViCCU was introduced.
There was no significant change in median treatment time for critical care patients (231 min [95% CI, 204–282 min] BV v 226 min [95% CI, 195–259 min] AV) or for major trauma patients (145 min [95% CI, 113–275 min] BV v 211 min [95% CI, 175–286 min] AV). For moderate trauma patients, median treatment time increased (128 min [95% CI, 90–175 min] BV v 188 min [95% CI, 165–232 min] AV). There was no change in the BMH median treatment time for patients transferred by the AMRS (203 min [95% CI, 143–245 min] BV v 172 min [95% CI, 95–199 min] AV).
The average number of procedures performed at BMH per patient did not change for trauma patients (3.2 BV v 3.7 AV), but increased from 4.0 (BV) to 5.0 (AV) for critical care patients (t = 2.039; df = 152; P = 0.04). The use of haemorrhage control within BMH increased (10.6% BV v 22.1% AV; χ2 = 8.286; df = 1; P = 0.004). There was no before–after difference in intubation rate (58.6% BV v 64.6% AV), central venous access (1.2% BV v 2.2% AV), administration of inotropes (10.0% BV v 9.9% AV) or thrombolysis (1.2% BV v 1.1% AV) at BMH overall. However, for patients transferred to NH, inotrope administration rates increased (2.2% [95% CI, 0–6.2%] BV v 15.8% [95% CI, 9.9%–21.7%] AV), as did intravenous fluid administration rates (76.6% [95% CI, 64.5%–88.7%] BV v 94.7% [95% CI, 87.6%–100%] AV).
Thirty-one of 33 clinicians (94%) participated in interviews at the two sites. At BMH, six of seven doctors and 12 of 13 nurses participated. All 13 NH specialists participated (nurses at NH did not use the ViCCU).
All NH specialists reported that the ViCCU allowed them to increase decision support to BMH clinicians and that this had improved patient management. Some specific examples of their responses in this regard are shown in Box 7.
Over half the NH specialists referred to an increase in their workloads. For example:
Concerns were raised by some about the increasing use of the ViCCU for minor conditions:
Specialists commented on perceptions of increased responsibility:
Clinicians at BMH reported feelings of greater support:
But some reported loss of autonomy:
Several BMH nurses reported increased perceptions of autonomy, and nine reported they felt less stressed after the introduction of the ViCCU. The majority of clinicians at both hospitals reported that interhospital relationships had improved. As one NH specialist reported, “[I]t’s a bit easier to see the problems that they have up there”, while one BMH doctor stated “[I]t’s actually created more commitment on their [NH’s] part to supervise [our ED]”. Nurses, particularly, reported that the ViCCU had enabled them to develop relationships with NH specialists that were not possible when telephones were the only avenue of support.
We found significant changes in some patient management indicators but not in patient outcome indicators. Admissions to BMH halved and discharges increased by 40% overall. The increased discharges among moderate trauma patients, who were also less likely to be transferred, suggests the ViCCU is effective in identifying patients not requiring further care. United Kingdom studies of ED telemedicine systems to assess minor injuries have reported reduced patient transfers9 and no negative effects in terms of return visits or need for additional care.3 Increased transfers of critical care patients suggest that the ViCCU supported these decisions. Alternatively, NH specialists may have lowered their transfer decision threshold because they felt more responsible for patients with whom they had visual contact than patients known only through telephone contact (under the previous system). Some clinicians had reported this effect at interview.
Our failure to demonstrate significant changes in outcomes could have arisen because patients were already receiving good care and improvements in management were unlikely to change outcomes. It is also possible that the ViCCU affected decisions as intended, but that these had little impact, as treatments instituted may not have affected the underlying disease process.
As our study was not a randomised controlled trial, any differences or non-differences observed could potentially be attributable to other factors. We were reliant on routinely collected data, some of which were of limited quality. A large-scale prospective trial is required to address such limitations.
The interviews with clinicians revealed positive and negative issues. Increased workloads and feelings of greater responsibility of those being consulted, including expansion of the support now being requested via the ViCCU, were central issues. Lack of recognition of increased workloads has been found to hinder the adoption of telemedicine10 and is important in sustainability of services.
Improved understanding between staff at the two hospitals occurred as a result of both using the ViCCU and changes in organisational processes undertaken during implementation. This knowledge may have influenced specialists’ transfer decisions and contributed to the increased transfer rate for critical care patients. It is possible that organisational change processes may be as effective in improving patient management as a telemedicine system.
Telemedicine interventions are rarely subjected to the same level of scrutiny as other health interventions. More concerning is the increasing investment in telemedicine in the absence of robust data on efficacy or effectiveness.11 Our results demonstrate that technologies may have unanticipated effects not previously reported, such as clinicians feeling more responsible for remote patients. We urge future telemedicine developers to identify at the outset the mechanisms by which clinical benefits will arise and specify indicators by which expected benefits may be measured using a controlled study design.
1 View of the Virtual Critical Care Unit at the local site at Blue Mountains District ANZAC Memorial Hospital
4 Case type of selected patients
Case type |
Definition |
||||||||||||||
Critical care |
Patients with acute, life-threatening illness |
||||||||||||||
Major trauma |
Patients experiencing a blunt or penetrating external force exerted on the body, causing significant physiological changes or meeting trauma criteria including:
|
||||||||||||||
Moderate trauma |
Patients experiencing a blunt or penetrating external force exerted on the body resulting in ≥ 2 injuries |
||||||||||||||
5 Patient characteristics before and after implementation of the ViCCU
Characteristic |
Before ViCCU (BV) (n = 169)* |
After ViCCU (AV) (n = 181)* |
Test for BV–AV difference |
||||||||||||
Triage category and case type |
|
|
χ2 = 5.223; df = 5; P = 0.39 |
||||||||||||
Resuscitation, critical care |
76 (45.0%) |
68 (37.6%) |
|
||||||||||||
Resuscitation, major trauma |
16 (9.5%) |
15 (8.3%) |
|
||||||||||||
Resuscitation, moderate trauma |
11 (6.5%) |
14 (7.7%) |
|
||||||||||||
Emergency, critical care |
5 (3.0%) |
2 (1.1%) |
|
||||||||||||
Emergency, major trauma |
40 (23.7%) |
58 (32.0%) |
|
||||||||||||
Emergency, moderate trauma |
21 (12.4%) |
24 (13.3%) |
|
||||||||||||
Age |
|
|
χ2 = 1.414; df = 3; P = 0.70 |
||||||||||||
0–24 years |
48 (28.4%) |
55 (30.4%) |
|
||||||||||||
25–49 years |
51 (30.2%) |
60 (33.2%) |
|
||||||||||||
50–74 years |
35 (20.7%) |
37 (20.4%) |
|
||||||||||||
≥ 75 years |
35 (20.7%) |
29 (16.0%) |
|
||||||||||||
Sex |
|
|
χ2 = 2.077; df = 1; P = 0.15 |
||||||||||||
Male |
108 (63.9%) |
102 (56.4%) |
|
||||||||||||
Female |
61 (36.1%) |
79 (43.6%) |
|
||||||||||||
ViCCU = Virtual Critical Care Unit. * Figures represent number (%) of patients. |
|||||||||||||||
6 Estimated likelihood of admission, discharge and transfer from BMH ED before and after implementation of the ViCCU
|
Admission |
Discharge |
Transfer |
||||||||||||
Patient group |
Before |
After |
P |
Before |
After |
P |
Before |
After |
P |
||||||
Critical care |
0.54 |
0.30 |
0.01 |
0.15 |
0.15 |
ns |
0.21 |
0.39 |
0.01 |
||||||
Major trauma |
0.13 |
0.13 |
ns |
0.19 |
0.19 |
ns |
0.66 |
0.66 |
ns |
||||||
Moderate trauma |
0.05 |
0.05 |
ns |
0.45 |
0.63 |
0.039 |
0.48 |
0.25 |
0.01 |
||||||
All patients |
0.30 |
0.15 |
0.001 |
0.25 |
0.35 |
0.045 |
0.38 |
0.38 |
ns |
||||||
BMH = Blue Mountains District ANZAC Memorial Hospital. ED = emergency department. ns = not significant. ViCCU = Virtual Critical Care Unit. |
|||||||||||||||
7 Interviews with NH specialists: examples of ways in which information provided via the ViCCU was reported as influencing patient management
“The question was, should we give thrombolysis. If I’d had that ECG described to me over the phone, I would have said ‘yes’ . . . [but] we had a look at some old ECGs on the ViCCU and . . . decided against thrombolysis on the strength of that.”
“. . . a septic patient . . . we got the ViCCU cranked up then, from the end of the bed it was . . . obvious that this person was in quite severe respiratory failure and needed to be intubated and put on a ventilator promptly. The vital signs hadn’t been recognised by [the staff at BMH ED], and that’s the sort of thing again, just standing at the end of the bed, I would have thought it would be . . . obvious . . . but it wasn’t. Having the visual cue there made all the difference.”
“There was a 3-year-old . . . run over by a car. [Another NH specialist and I] had a look [via the ViCCU] and said ‘They look like full thickness burns, don’t they?’ They [BMH] put the portable camera on and it is like, ‘oh yeah, why don’t you pinprick him?’ So they pinpricked it and the skin didn’t bleed. It was full thickness burns. So we go, ‘Wow, well that’s the problem’. So, number one, they hadn’t actually identified that problem. Number two, we saw it instantly when we turned the ViCCU on. We took about 3 seconds to work it out, mainly because of experience, and skill, but a fresh set of eyes without all these extraneous red herrings.”
BMH = Blue Mountains District ANZAC Memorial Hospital. ECG = electrocardiogram. ED = emergency department. NH = Nepean Hospital. ViCCU = Virtual Critical Care Unit. | |||||||||||||||
Received 5 September 2007, accepted 17 December 2007
- Johanna I Westbrook1
- Enrico W Coiera2
- Michelle Brear2
- Stuart Stapleton3
- Marilyn I Rob1
- Monique Murphy3
- Patrick Cregan3
- 1 Health Informatics Research and Evaluation Unit, University of Sydney, Sydney, NSW.
- 2 Centre for Health Informatics, University of New South Wales, Sydney, NSW.
- 3 Nepean Hospital, Sydney, NSW.
The CSIRO designed and built the ViCCU in collaboration with clinicians from the BMH and NH. We thank the clinicians at BMH and NH for their support and participation in our research.
Our research was funded by NSW Health. Johanna Westbrook was funded by a National Health and Medical Research Council fellowship. Monique Murphy was funded by the Australian Council for Safety and Quality in Health Care. The Centre for Health Informatics is supported by a NSW Health Capacity Building Infrastructure grant. The authors had full independence from the funding bodies.
- 1. Hersh WR, Hefland M, Wallace J, et al. Clinical outcomes resulting from telemedicine interventions: a systematic review. BMC Med Inform Decis Mak [Internet] 2001; 1: 5. Epub 2001; Nov 26. http://www.biomedcentral.com/1472-6947/1/5 (accessed Jan 2008).
- 2. Hailey D, Ohinmaa A, Roine R. Study quality and evidence of benefit in recent assessments of telemedicine. J Telemed Telecare 2004; 10: 318-324.
- 3. Brennan JA, Kealy J, Geradi L, et al. A randomized controlled trial of telemedicine in an emergency department. J Telemed Telecare 1998; 4: 18-20.
- 4. Hailey D, Roine R, Ohinmaa A. Systematic review of evidence for the benefits of telemedicine. J Telemed Telecare 2002; 8 Suppl 1: 1-30.
- 5. Coiera EW, Jayasuriya RA, Hardy J, et al. Communication loads on clinicians in the emergency department. Med J Aust 2002; 176: 415-418. <MJA full text>
- 6. Spencer R, Coiera E, Logan P. Variation in communication loads on clinical staff in the emergency department. Ann Emerg Med 2004; 44: 268-273.
- 7. Cregan P, Stapleton S, Wilson L, et al. The ViCCU Project — achieving virtual presence using ultrabroadband internet in a critical clinical application — initial results. In: Westwood JD, Haluck RS, Hoffman HM, et al, editors. Medicine meets virtual reality 13: the magical next becomes the medical now. Long Beach: IOS Press, 2005: 94-98. (Studies in health technology and informatics Vol. 111.)
- 8. Australian College of Emergency Medicine. Guidelines for implementation of the Australasian Triage Scale in emergency departments. Melbourne: ACEM, 2000. http://www.medeserv.com.au/acem/open/documents/triageguide.htm (accessed Jan 2008).
- 9. Tachakra S, Uko Uche C, Stinson A. Four years’ experience of telemedicine support of a minor accident and treatment service. J Telemed Telecare 2002; 8 Suppl 2: 87-89.
- 10. Lam DM, Mackenzie C. Human and organizational factors affecting telemedicine utilization within US military forces in Europe. Telemed J E Health 2005; 11: 70-78.
- 11. Brebner EM, Brebner J, Ruddick-Bracken H, et al. Evaluation of a pilot telemedicine network for accident and emergency work. J Telemed Telecare 2002; 8 Suppl 2: 5-6.






Abstract
Objectives: To evaluate whether introduction of an emergency department (ED) telemedicine system changed patient management and outcome indicators and to investigate clinicians’ perceptions of the impact of the system on care provided and on their work.
Design: Before-and-after study of use of the Virtual Critical Care Unit (ViCCU), which uses an ultrabroadband connection allowing real-time audiovisual communication between clinicians at distant sites. Semi-structured interviews were conducted with medical and nursing staff at the end of the study.
Participants and setting: The ViCCU intervention commenced on 1 January 2004. Our study was conducted in the EDs of an 85-bed district hospital and a 420-bed metropolitan tertiary hospital. It involved all acutely ill patients requiring urgent care (defined by triage category and grouped into critical care, major trauma and moderate trauma) who were treated during the 12 months before (n = 169) and 18 months after (n = 181) the intervention at the district hospital. Thirty-one of 33 clinicians (doctors and nurses) participating at the two hospitals took part in interviews at the end of the study.
Main outcome measures: Changes in patterns of management (disposition [admission, discharge or transfer], treatment times, number of procedures) and outcomes (rapid acute physiology scores, hours on ventilation or in intensive care, length of stay).
Results: Patient disposition remained unaltered for major trauma patients. For critical care patients, admissions fell significantly (54% to 30%), transfers increased (21% to 39%), and more procedures were performed. For moderate trauma patients, discharges increased significantly (45% to 63%), transfers decreased (48% to 25%) and treatment times were longer. No significant changes were found in outcome indicators. Clinicians reported that the ViCCU allowed greater support to remote clinicians. Specialists reported increased workloads and feelings of greater responsibility for patients at the district hospital. Nurses at the district site reported reduced stress, but district doctors reported some loss of autonomy.
Conclusions: The ViCCU appears most effective for moderate trauma patients, with associated reductions in admissions and transfers. Large-scale trials of telemedicine systems that include measurements of both patient care and impact on clinicians’ work are required.