Ingredients in the two antiseptic bath oils used by these patients include benzalkonium chloride (6%), triclosan (2%), and paraffin. Direct contact with triclosan in formulated products has only rarely been associated with skin irritation or sensitisation in humans.1 Allergic contact dermatitis to benzalkonium chloride is also rare.2 Benzalkonium is a known strong cutaneous irritant and is reported to be corrosive to mucous membrane at a concentration of 10%.3
For Patient 1, the antiseptic bath oil was frequently being applied to his skin in the bathwater and not rinsed off. We believe that secondary occlusion to the groin (and axilla) by skin folds and the close fit of his nappy contributed to ongoing irritation. Prolonged contact with another bath oil with the same active ingredients in the same concentration has previously been reported to cause irritant dermatitis.3
Lessons from practice
Consider a diagnosis of acute contact dermatitis if brown hyperpigmentation and superficial desquamation complicate eczema, particularly if the patient is using an antiseptic bath oil.
Use antiseptic bath oils in a diluted concentration, not exceeding the manufacturer’s instructions.
If antiseptic bath oil is used, rinse off after use.
Use only plain bath oils for cool compresses and wet wraps.
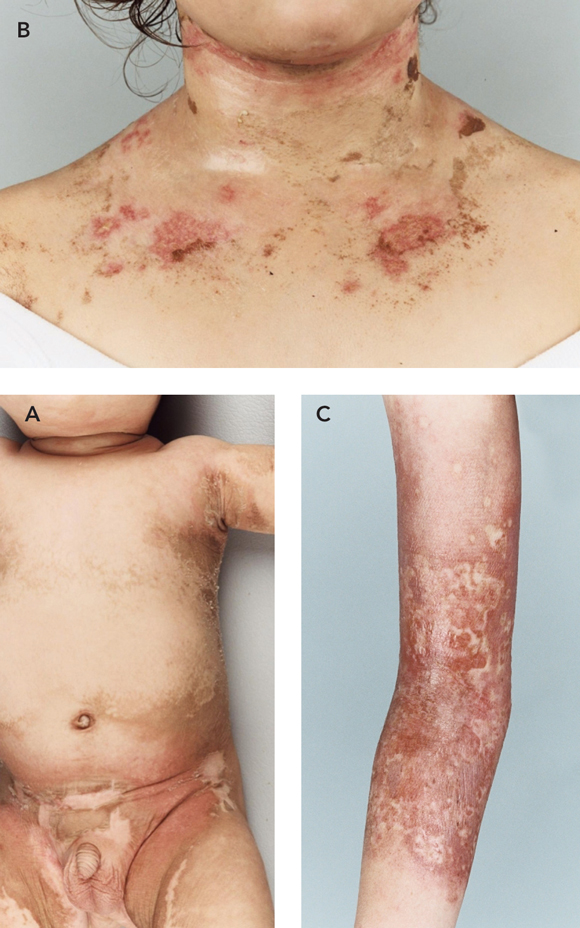
It remains unclear whether the frequent application of cool compresses to the softer skin of the neck of Patient 2 resulted in irritant contact dermatitis, or whether true allergy developed. Similar eruptions have been described in reaction to standard concentrations of bath oil, as well as to concentrations greater than the manufacturer’s recommendations.3-6 However, the distribution in this case suggested irritant contact dermatitis.
The older child, Patient 3, stated that she had had marked initial improvement after starting use of the bath oil. Her mother thought that after this improvement there may have been a decrease in vigilance in measuring the concentration of the oil, as well as possible prolonged exposure time, which probably resulted in the subsequent acute burn seen in Figure C. A case has been previously described where an increased concentration of the same antiseptic bath oil caused subcorneal pustular dermatitis, with some features resembling a chemical burn, and restriction of movement.6
It is notable that, in all three cases, the thinner skin folds were preferentially affected. This has been previously described, when total body application of antiseptic bath oil to a 27-year-old man resulted in diffuse swelling of his penis and scrotum only.5
- 1. Bhargava HN, Leonard PA. Triclosan: applications and safety. Am J Infect Control 1996; 24: 209-218.
- 2. Basketter DA, Marriott M, Gilmour NJ, White IR. Strong irritants masquerading as skin allergens: the case of benzalkonium chloride. Contact Dermatitis 2004; 50: 213-217.
- 3. Loo WJ, Alexandroff A, Burrows NP. Irritant dermatitis due to prolonged contact with Oilatum Plus®. Br J Dermatol 2003; 148: 171-172.
- 4. Ling TC, Highet AS. Irritant reactions to an antiseptic bath emollient. J Dermatolog Treat 2000; 11: 263-267.
- 5. Saw NK, Hindmarsh JR. Acute irritant reaction to an antiseptic bath emollient. Postgrad Med J 2005; 81: 131-132.
- 6. Storer E, Koh KJ, Warren L. Severe contact dermatitis as a result of an antiseptic bath oil. Australas J Dermatol 2004; 45: 73-75.





We wish to thank the other staff members of the dermatology team, and other staff members of the Royal Children’s Hospital for their contributions to the care of these children.
None identified.