Humans are one of the few mammals that cannot synthesise vitamin C (ascorbic acid). Stores are readily depleted, with studies showing clinical manifestations after about a month on a vitamin C-free diet.1 Vitamin C is absorbed by an energy-dependent, saturable transport system throughout the length of the small intestine, with any excess excreted by the kidneys. Ascorbic acid promotes the hydroxylation of proline and lysine residues in procollagen, helping to stabilise the collagen triple helix. It is the defect in collagen synthesis that produces most of the clinical manifestations.
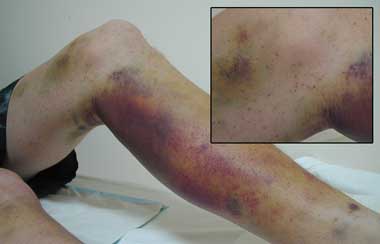
Vitamin C is particularly abundant in citrus fruit and many green vegetables. Scurvy is usually seen in mentally ill patients, people on “fad” diets, people who misuse alcohol, and, occasionally, elderly patients who live alone.2 Initial symptoms are non-specific, including weakness, anorexia, depression and lethargy. Subsequent dermatological features include broken and coiled hairs (due to abnormal keratin formation) and perifollicular haemorrhages and hyperkeratosis. Bleeding tends to be a late feature and affects spongy, friable gums as well as muscles, joints and skin. This is thought to be due to breakdown of the connective tissue within and supporting the vessel walls, rather than a platelet or clotting factor defect.3 Many patients with scurvy are anaemic, with contributing causes likely to be bleeding, altered absorption and metabolism of iron and folate,3 and other dietary deficiencies.
- 1. Padayatty SJ, Levine M. New insights into the physiology and pharmacology of vitamin C. CMAJ 2001; 164: 353-355.
- 2. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 39-1995. A 72-year-old man with exertional dyspnea, fatigue, and extensive ecchymoses and purpuric lesions. N Engl J Med 1995; 333: 1695-1702.
- 3. Reuler JB, Broudy VC, Cooney TG. Adult scurvy. JAMA 1985; 253: 805-807.





None identified.