Clinical record
|
Fluorescein staining of a central corneal scar after Pseudomonas keratitis  A: View with the naked eye 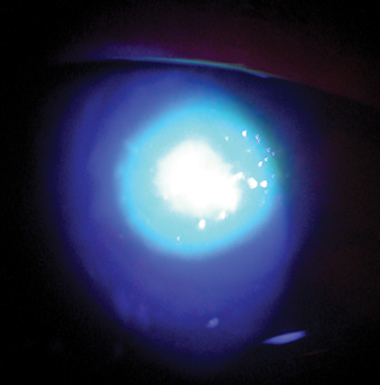 B: Slit-lamp view |
Keratitis remains a significant risk of wearing contact lenses, despite advances over the past 10 years such as disposable and silicone hydrogel lenses. The incidence of severe keratitis from extended hydrogel lens wear was estimated at 96.4 (95% CI, 37.5–254.2) per 10 000 lens wearers in a British study.1 Even among users of daily disposable hydrogel lenses, the incidence of severe keratitis was 4.9 (95% CI, 2.5–9.6) per 10 000 lens wearers.
Contact lens keratitis is precipitated by microtrauma from lens wear, which allows pathogens (Pseudomonas aeruginosa, Acanthamoeba spp., Streptococcus spp., Staphylococcus spp., Serratia spp., Fusarium spp., Aspergillus spp., Curvularia spp., Herpes simplex virus, and others) to invade the damaged cornea. Pseudomonas aeruginosa is one of the most virulent and common pathogenic organisms. It possesses virulence factors that facilitate survival and growth in the human cornea, including bacterial cell surface adherence factors and secreted cytotoxins that destroy corneal epithelium.2 The host immune response further damages the cornea,3 leading to scarring and loss of visual acuity and function. A Pseudomonas corneal ulcer is usually located centrally, and infection develops and progresses rapidly. Among people with contact lens keratitis, Pseudomonas accounts for the largest mean diameter of corneal ulcers, the highest mean nmber of days in hospital, the greatest mean number of outpatient visits, and the poorest visual acuity outcome.4
Lessons from practice
Contact lens keratitis is a potentially vision-destroying infection.
Pseudomonas keratitis progresses rapidly and often results in significant scarring and visual loss.
Lens wearers presenting with a red eye should be referred early for specialist care.
Contact lens wearers need to be properly educated regarding contact lens handling and hygiene and made aware of the serious risk of keratitis.
Poor contact lens hygiene is a well known risk factor for keratitis.5,6 However, the importance of contact lens hygiene is still poorly appreciated by the community. In a survey of contact lens keratitis in New South Wales, 40% of keratitis patients reported poor hygiene.7 In a study of contact lens users in Auckland, 81% of cosmetic contact lens cases were contaminated with various pathogens.8
- 1. Morgan PB, Efron N, Hill EA, et al. Incidence of keratitis of varying severity among contact lens wearers. Br J Ophthalmol 2005; 89: 430-436.
- 2. Fleiszig SMJ, Evans DJ. The pathogenesis of bacterial keratitis: studies with Pseudomonas aeruginosa. Clin Exp Optom 2002; 85: 271-278.
- 3. Hazlett LD. Corneal response to Pseudomonas aeruginosa infection. Prog Retin Eye Res 2004; 23: 1-30.
- 4. Cheng KH, Leung SL, Hoekman HW, et al. Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet 1999; 354: 181-185.
- 5. Poggio EC, Glynn RJ, Schein OD, et al. The incidence of ulcerative keratitis among users of daily-wear and extended-wear soft contact lenses. N Engl J Med 1989; 321: 779-783.
- 6. Lam DS, Houang E, Fan DS, et al. Incidence and risk factors for microbial keratitis in Hong Kong: comparison with Europe and North America. Eye 2002; 16: 608-618.
- 7. Butler TK, Males JJ, Robinson LP, et al. Six-year review of Acanthamoeba keratitis in New South Wales, Australia: 1997–2002. Clin Experiment Ophthalmol 2005; 33: 41-46.
- 8. Gray TB, Cursons RT, Sherwan JF, et al. Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases. Br J Ophthalmol 1995; 79: 601-605.





None identified.