Chironex fleckeri, the major Australian box jellyfish (Class Cubozoa), has been the attributed cause of around 70 fatal jellyfish envenomings in tropical Australian waters.1 C. fleckeri is a multitentacled (Order Chirodropidae) box jellyfish with a bell up to 35 cm in diameter, with up to 15 tentacles off each of the four pedalia of the bell. The taxonomy of multitentacled box jellyfish remains poorly defined, with a number of other species implicated in deaths in the northern hemisphere and the northernmost distribution of C. fleckeri not established.1
A second chirodropid species has long been recognised in northern Queensland waters.1-4 This was originally called Chiropsalmus quadrigatus, but is now recognised to be a different species from the C. quadrigatus responsible for many fatalities in the Philippines and Japan.1,5 Furthermore, another multitentacled box jellyfish, the Gove chirodropid, has recently been described from the Gove Peninsular in north-east Arnhem Land, Northern Territory.6 To date, these two species have not been associated with documented fatalities; their stings are similar to mild C. fleckeri envenoming.
Stinging cells (nematocysts) from the three species, seen on microscopy of skin scrapings or sticky tape samples from victims, cannot reliably distinguish between the species.1,3,6 The Gove chirodropid and northern Queensland Chiropsalmus spp. have, as yet, not been reported from the Darwin harbour or Tiwi islands (Phil Alderslade, Northern Territory Museum of Arts and Sciences, personal communication).
Here, we present an analysis of prospectively collected data from jellyfish sting patients who were stung in NT coastal areas where C. fleckeri is present, but the other two Australian chirodropid species have not been documented.
From April 1991, a standard data collection form has been used for patients presenting to RDH with suspected jellyfish envenoming; these forms have also been available at Gove Hospital and the coastal community health centres. Variables listed include demographic, weather and sea details, nature of the suspected sting and clinical parameters reflecting jellyfish envenoming. Treatment details, including the nature and route of analgesia and the use of antivenom, are also recorded. Skin scrapings and, more recently, sticky tape samples from the sting site are collected and processed at the Menzies School of Health Research.7,8 Nematocyst description and identification is based on previous publications.1,7,8 Skin sample results are divided into those with predominantly cigar-shaped nematocysts and therefore consistent with chirodropid box jellyfish, and those with predominantly lemon-shaped or round nematocysts and consistent with four-tentacled box jellyfish (Order Carybdeidae) such as the Darwin carybdeid.8 The National Tidal Centre provided tidal information, regional hourly wind speed and hourly sea surface and air temperatures over the duration of the study.
Data were stored in EpiData (version 3.02; EpiData Association, Odense, Denmark) and statistical analysis was performed using Intercooled Stata (version 7.9; Stata Corporation, College Station, Tex, USA). The study was approved by the Human Research Ethics Committee of the Menzies School of Health Research and the NT Department of Health and Community Services.
Between April 1991 and May 2004, of the 606 jellyfish report forms returned, 70 had clinical features consistent with classical descriptions of the Irukandji syndrome,1 while 110 others had no nematocysts seen on microscopy, and a further 108 did not have skin samples taken for microscopy. Of the 318 that were positive on microscopy, 35 had nematocysts not consistent with C. fleckeri or the other two chirodropids (29 of these were stung in Darwin Harbour and had nematocysts consistent with the Darwin carybdeid). The remaining 283 had cigar-shaped nematocysts consistent with chirodropid envenoming. Of these, 58 were from Arnhem Land where both C. fleckeri and the Gove chirodropid are present, and 225 were stung in Darwin Harbour or the Tiwi Islands and were thus classified as C. fleckeri envenoming.
Box 1 shows the circumstances and features of those with C. fleckeri envenoming. Most stings occurred in the months November–April, with only 17 (8%) occurring outside the official NT “stinger season” of 1 October till 1 June (eight in June, five in July, 2 in August and 2 in September). Box 2 shows the time of day, tide cycle and weather parameters for the C. fleckeri envenomings.
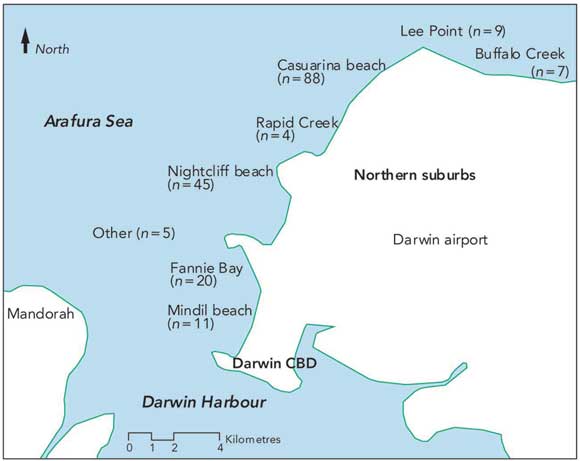
Nearly all of those stung by C. fleckeri were NT residents; their median age was 17 years and 37% were children aged under 15 years. Stings were almost twice as likely to occur between 15:00 and 18:00 than in either of the two preceding 3-hour periods of daylight. Most C. fleckeri stings (84%) occurred at a depth of 1 metre or less, with 17% occurring on entering the water and 43% while standing in the water. The only sting in water over 2 metres deep occurred while the victim was pulling an anchor aboard a boat in 5 metres of water. There was a statistically significantly lower proportion of stings on the outgoing tide than for the rest of the tidal cycle. Stings were rare during strong winds, and wind speeds at time of sting were below the median for that month in 72% of stings; median wind speed during the hour of each sting was 1.3 m/s (2.5 knots), compared with a median monthly speed of 2.7 m/s (5.2 knots) for all stings (Wilcoxon signed rank test, P < 0.001).Box 3 shows the location of the Darwin Harbour beaches which were the sites of 189 stings.
All people with C. fleckeri envenoming had sting marks with linear welts the most common presentation. The legs were most commonly affected and the maximum sting length was 4.2 metres. Although it is unusual for more than two limbs to be affected, 25 (11%) had five or more discrete body sites affected. Adherent tentacles were present in 32%, and the cross-hatching which reflects bands of nematocysts perpendicular to the tentacle line was present in 27%. Onset of pain after tentacle contact was immediate in 94%, vinegar was applied in all but one case where this was documented, and ice in 71%. Analgesia in addition to ice was required in 48%, with parenteral narcotic required in 30%. Eight per cent of those with of C. fleckeri stings required hospital admission. In accordance with long-standing NT policy, pressure-immobilisation first aid was not used for any sting.
Box 4 gives details of the 22 patients with jellyfish stings of any kind who were given antivenom. Eleven patients given antivenom were considered to have C. fleckeri envenoming, being either from Darwin or the Tiwi Islands. It is probable that the four patients with chirodropid-positive stings from Arnhem Land who were given antivenom were also stung by C. fleckeri. Of the seven Arnhem Land patients given antivenom who were nematocyst negative or in whom the skin test was not done, one had Irukandji syndrome and was given antivenom inappropriately, one was stung in September which is before the official stinger season and was possibly stung by a Gove chirodropid,6 and the other five may well have been stung by C. fleckeri. There were no documented adverse reactions to antivenom.
Box 5 shows the clinical features of the one fatality. In addition to the fatal case, two other patients experienced collapse with loss of consciousness within several minutes of the sting. Both woke after brief cardiopulmonary resuscitation; the 10-year-old boy (Box 4) who was subsequently given antivenom; and a 4-year-old boy with 3.6 metres of tentacle contact whose skin sticky-tape sample was positive for nematocysts consistent with C. fleckeri, and who was subsequently treated with intravenous narcotics, but no antivenom. Immediate excruciating pain over the tentacle contact sites was universal in all severe stings, and sinus tachycardia and sinus arrhythmia were common in severe cases. More worrying electrocardiogram findings were unusual, but conduction abnormalities included: periods of sinus arrest in a 5-year-old with 1.7 metres of tentacle contact, which persisited after 1 ampoule of intravenous antivenom, but subsequently resolved; unifocal ventricular ectopic beats with runs of bigeminy in a 27-year-old with 0.6 metres of tentacle contact which resolved after intramuscular narcotic; and right bundle branch block in a 25-year-old with 0.7 metres of tentacle contact which resolved after intramuscular narcotic.
C. fleckeri has been described as “the world’s most venomous animal”1 because of the dramatic nature of severe envenoming, where death may occur within a few minutes of tentacle contact. However, our prospective study has confirmed that the vast majority of C. fleckeri envenomings are not life-threatening.
Attributing stings to specific jellyfish species is problematic because of uncertainties about jellyfish taxonomy and similar nematocyst morphology between species such as the multitentacled box jellyfish (chirodropids).1,3,4,6 Because both C. fleckeri and Chiropsalmus spp. occur in northern Queensland waters, and both C. fleckeri and the Gove chirodropid occur in Arnhem Land waters, chirodropid nematocysts from stings from these locations cannot usually be definitively attributed to C. fleckeri. Nevertheless, it is likely that the reported severe stings and fatalities from northern Queensland and the NT were C. fleckeri envenomings.9-11 However, in chirodropid-nematocyst-positive stings from Darwin Harbour and the Tiwi Islands, where the other two chirodropids have not been found, attribution to C. fleckeri is considered valid even for less severe stings. This enables us to report the clinical spectrum of 225 C. fleckeri stings.
One limitation of our study is that we are unable to quantify the risks as we do not know how many people were in the water during various times of day, tidal cycles and weather conditions. However, most C. fleckeri stings occur when the weather is “fine” and the wind is “still” or slight. Stings are also most common in shallow water, and frequently occur on entering the sea. These features reflect the natural history of C. fleckeri which develops and replicates as polyps in tidal estuarine creeks and enters the sea at the beginning of each stinger season.12 The species is generally a shallow-water feeder, but is easily damaged by surf or rough seas and has the ability to sink to the ocean floor to rest.13 However, our data do not support the observation that this resting occurs from 15:00,13 as stings in our study were most common between 15:00 and 18:00. The significantly lower proportion of stings during the outgoing tide is likely to reflect C. fleckeri avoiding potential stranding by moving further offshore. In adverse weather, C. fleckeri may swim offshore and sink to calmer deep water until storms pass, or may move up tidal creeks. This is different from the natural history of the smaller four-tentacled box jellyfish (carybdeids) which cause the Irukandji syndrome. Humans may encounter these carybdeids during periods of onshore winds in shallow water or in deeper water offshore in the case of divers.1,14,15
C. fleckeri stings affected people of all ages, with a slight male predominance. Interestingly, the vast majority of stings were in NT residents, which reflects both the risk-taking behaviour of local residents and visitors heeding the well publicised health warnings about not entering the water during the stinger season. Overall, Aboriginal patients were not over-represented in terms of NT demographics, but most stings outside Darwin were in Aboriginal people from remote communities. All C. fleckeri envenomings had sting marks, with linear welts being the most common presentation, adherent tentacles in almost a third, and cross-hatching of the welts in one quarter (Box 6). Vinegar was almost universally used, ice was often adequate for pain relief, but half required some form of analgesia, and almost a third required parenteral narcotics. Few required hospital admission. In some of those with severe pain not controlled by narcotics, antivenom appeared helpful, although attribution of improvement to the antivenom cannot be definitive.
In this study, 22 patients had been given C. fleckeri antivenom, one inappropriately as the patient had Irukandji syndrome for which the antivenom is ineffective.16 The biological basis of the lethal activity of C. fleckeri venom remains to be fully elucidated, with the specific toxins involved yet to be characterised.17,18 In animals, C. fleckeri venom causes abnormalities in ionic transport across membranes resulting in altered membrane permeability which affects both sodium and calcium channels.19 Cardiac and skeletal muscle, smooth muscle, cardiac conduction pathways, and, possibly, central neurological pathways are affected. Cardiotoxicity appears to be the major outcome, with impaired cardiac contraction, hypertension then hypotension, arrhythmias (such as various conduction blocks and ventricular tachycardia), and decreased coronary flow.17 The most recent studies in rats20 support previous concerns about suboptimal activity of C. fleckeri antivenom against lethal factors in C. fleckeri venom,21 while also supporting studies in piglets which suggested that the previously recommended use of calcium antagonists such as verapamil may be harmful in C. fleckeri envenoming.22 In addition, the recently reported potential benefit of magnesium for the Irukandji syndrome23,24 was also seen in the C. fleckeri rat study. In particular, a combination of intravenous magnesium and antivenom was beneficial, and this should be considered in severe human envenoming.20
The last 10 people who have died from jellyfish envenoming in the NT have all been children, reflecting the greater risk of a smaller body mass exposed to the billions of nematocysts on jellyfish tentacles.17 The single fatality from C. fleckeri in this study shows how rapidly cardiopulmonary arrest can follow severe envenoming.11 The 1.2 m of tentacle contact in this case is the smallest yet described in a fatality. There have been two further deaths from northern Queensland, both with similar rapid cardiopulmonary arrest following tentacle contact; the victims were a 5-year-old boy in January 2000 and a 7-year-old boy in March 2003. The NT case is the only one, to our knowledge, in which verapamil was used, but the chronology suggests that verapamil and the antivenom were given at a time when irreversible hypoxic damage had already occurred. Nevertheless, it is important to note that intramuscular antivenom given to a patient in cardiac arrest and circulatory shutdown is unlikely to be absorbed. Other reports of use of intramuscular C. fleckeri antivenom25,26 were not in situations of cardiac arrest and the subjective reports of improvement may well have reflected spontaneous improvement, which was seen in the vast majority of stings in this study. While there are a number of published reports of people with severe envenoming who have survived and who have been given antivenom,9,10 there are similar case reports where antivenom was not given, but patients survived with expert critical care management. These included a 12-year-old boy in the pre-antivenom era with a documented 16 metres of tentacle contact.27 On the other hand, there have now been four documented deaths despite the use of C. fleckeri antivenom, including two where it was given intramuscularly.17 In none of the 21 survivors in this study who were given antivenom could survival be attributed to the antivenom. Indeed, in one of these, and in another child not given antivenom, recovery from documented rapid loss of consciousness occurred after attempted cardiopulmonary resuscitation at the scene and before arrival at a health facility.
Because of the rapidity of fatal C. fleckeri envenoming, the critical window of opportunity for potentially life-saving use of antivenom is much smaller than that for snake envenoming, possibly only minutes. Furthermore, from animal study data, it was calculated that around 12 ampoules of antivenom may be required to counter the effects of a theoretical envenoming containing twice the human lethal dose of venom.21 Therefore, the situation where C. fleckeri antivenom may save a life is a severe sting with cardiorespiratory arrest near a health centre or hospital, where immediate resuscitation and rapid use of large volumes of intravenous antivenom is possible. It is for this scenario that the NT revised protocol for managing severe C. fleckeri envenoming is written,8 with the potential use of intravenous magnesium recently added (see Box 7).
Our prospective study has confirmed that, for most C. fleckeri stings, treatment with vinegar, followed by pain relief with ice and oral or parenteral analgesia if required, is adequate.
1 Details and circumstances of 225 Chironex fleckeri stings*
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
|
* Denominator is 225 unless indicated, where data was not available for all cases. |
|||||||||||||||
3 Darwin Harbour, showing locations of the occurrence of Chironex fleckeri stings
CBD = central business district.
4 Details of 22 patients given Chironex fleckeri antivenom
|
|
|||||||||||||||
|
Woke after brief CPR; then AV with narcotic; decreased pain, but needed more narcotic |
|||||||||||||||
|
Tourist. AV after narcotic; no response, given more narcotic |
|||||||||||||||
|
|
|||||||||||||||
5 Fatal Chironex fleckeri envenoming, February 1996.
|
|
|||||||||||||||
|
Intravenous access obtained; adrenaline and bicarbonate given intravenously. |
|||||||||||||||
7 Summary of treatment of Chironex fleckeri stings — the revised Northern Territory protocol
- Bart J Currie1
- Susan P Jacups2
- Menzies School of Health Research, Charles Darwin University, and Northern Territory Clinical School, Flinders University and Royal Darwin Hospital, Darwin, NT.
We are extremely grateful to the many nurses and doctors who have assisted with this study and with treating the patients, including Nick Barclay, Philippa Binns, Allen Cheng, Sam Hone, Geoff Isbister, Rowena Ivers, Gerrard O’ Reilly, Didier Palmer, Vijay Selvarajah, Marg St Leone, Peter Thorn and Jo Wright. We thank Yvonne Wood, Jacquie Rifkin, Melita McKinnon, Maree Brennan, Paula Lawrie and Kevin Lee for assistance with nematocyst microscopy, Phil Alderslade from the NT Museum of Arts and Sciences for taxonomy expertise, Daryl Metters from the National Tidal Centre, and Michael Foley and Peter Bate from the Darwin Bureau of Meteorology.
None identified.
- 1. Williamson JA, Fenner PJ, Burnett JW, Rifkin JK, editors. Venomous and poisonous marine animals — a medical and biological handbook. Sydney: University of New South Wales Press, 1996.
- 2. Barnes JH. Studies on three venomous cubomedusae. Symp Zool Soc London 1966; 16: 309-332.
- 3. Carrette T, Alderslade P, Seymour J. Nematocyst ratio and prey in two Australian cubomedusans, Chironex fleckeri and Chiropsalmus sp. Toxicon 2002; 40: 1547-1551.
- 4. Barnes JH. Chironex fleckeri and Chiropsalmus quadrigatus — morphological distinctions. North Queensland Naturalist 1965; 32: 13-22.
- 5. Koyama T, Noguchi K, Matsuzaki T, et al. Haemodynamic effects of the crude venom from nematocysts of the box-jellyfish Chiropsalmus quadrigatus (Habu-kurage) in anaesthetized rabbits. Toxicon 2003; 41: 621-631.
- 6. Currie BJ, McKinnon M, Whelan B, Alderslade P. The Gove chirodropid: a box jellyfish appearing in the “safe season”. Med J Aust 2002; 177: 649.
- 7. Currie BJ, Wood YK. Identification of Chironex fleckeri envenomation by nematocyst recovery from skin. Med J Aust 1995; 162: 478-480.
- 8. O’Reilly GM, Isbister GK, Lawrie PM, et al. Prospective study of jellyfish stings from tropical Australia, including the major box jellyfish Chironex fleckeri. Med J Aust 2001; 175: 652-655. <MJA full text>
- 9. Williamson JA, Callanan VI, Hartwick RF. Serious envenomation by the Northern Australian box-jellyfish (Chironex fleckeri). Med J Aust 1980; 1: 13-16.
- 10. Williamson JA, Le Ray LE, Wohlfahrt M, Fenner PJ. Acute management of serious envenomation by box-jellyfish (Chironex fleckeri). Med J Aust 1984; 141: 851-853.
- 11. Lumley J, Williamson JA, Fenner PJ, et al. Fatal envenomation by Chironex fleckeri, the north Australian box jellyfish: the continuing search for lethal mechanisms. Med J Aust 1988; 148: 527-534.
- 12. Hartwick RF. Distribution ecology and behaviour of the early life stages of the box-jellyfish Chironex fleckeri. Hydrobiologia 1991; 216/217: 181-188.
- 13. Seymour JE, Carrette TJ, Sutherland PA. Do box jellyfish sleep at night? Med J Aust 2004; 181: 707. <MJA full text>
- 14. Macrokanis CJ, Hall NL, Mein JK. Irukandji syndrome in northern Western Australia: an emerging health problem. Med J Aust 2004; 181: 699-702. <MJA full text>
- 15. Little M, Mulcahy RF. A year’s experience of Irukandji envenomation in far north Queensland. Med J Aust 1998; 169: 638-641.
- 16. Fenner PJ, Rodgers D, Williamson J. Box jellyfish antivenom and “Irukandji” stings. Med J Aust 1986; 144: 665-666.
- 17. Currie BJ. Marine antivenoms. J Toxicol Clin Toxicol 2003; 41: 301-308.
- 18. Bailey PM, Little M, Jelinek GA, Wilce JA. Jellyfish envenoming syndromes: unknown toxic mechanisms and unproven therapies. Med J Aust 2003; 178: 34-37. <MJA full text>
- 19. Mustafa MR, White E, Hongo K, et al. The mechanism underlying the cardiotoxic effect of the toxin from the jellyfish Chironex fleckeri. Toxicol Appl Pharmacol 1995; 133: 196-206.
- 20. Ramasamy S, Isbister GK, Seymour JE, Hodgson WC. The in-vivo cardiovascular effects of box jellyfish Chironex fleckeri venom in rats: efficacy of pre-treatment with antivenom, verapamil and magnesium sulphate. Toxicon 2004; 43: 685-690.
- 21. Endean R, Sizemore DJ. The effectiveness of antivenom in countering the actions of box-jellyfish (Chironex fleckeri) nematocyst toxins in mice. Toxicon 1988; 26: 425-431.
- 22. Tibballs J, Williams D, Sutherland SK. The effects of antivenom and verapamil on the haemodynamic actions of Chironex fleckeri (box jellyfish) venom. Anaesth Intensive Care 1998; 26: 40-45.
- 23. Corkeron MA. Magnesium infusion to treat Irukandji syndrome. Med J Aust 2003; 178: 411. <MJA full text>
- 24. Corkeron M, Pereira P, Makrocanis C. Early experience with magnesium administration in Irukandji syndrome. Anaesth Intensive Care 2004; 32: 666-669.
- 25. Fenner PJ, Williamson JA, Blenkin JA. Successful use of Chironex antivenom by members of the Queensland Ambulance Transport Brigade. Med J Aust 1989; 151: 708-710.
- 26. Beadnell CE, Rider TA, Williamson JA, Fenner PJ. Management of a major box jellyfish (Chironex fleckeri) sting. Lessons from the first minutes and hours. Med J Aust 1992; 156: 655-658.
- 27. Maguire EJ. Chironex fleckeri (“sea wasp”) sting. Med J Aust 1968; 2: 1137-1138.







Abstract
Objective: To describe the epidemiology and clinical features of box jellyfish envenoming in the Top End of the Northern Territory and, in particular, confirmed stings from the major Australian box jellyfish, Chironex fleckeri.
Design: Prospective collection of clinical data and skin scrapings or sticky-tape tests for nematocyst identification from patients presenting to Royal Darwin Hospital and remote coastal community health clinics in the Northern Territory, spanning 10 950 km of coastline; analysis of tidal, weather and seasonal data.
Patients: All patients with jellyfish sting details recorded between 1 April 1991 and 30 May 2004.
Main outcome measures: Demographic and clinical features, use of C. fleckeri antivenom, and associations between weather, seasonal and tidal factors and confirmed C. fleckeri stings.
Results: Of 606 jellyfish stings documented, 225 were confirmed to have been caused by C. fleckeri. 37% of C. fleckeri stings were in children, 92% occurred during the “stinger season” (1 October to 1 June), 83% occurred in water 1 m or less deep, and 17% occured while victims were entering the water. Stings were least common on outgoing tides (P < 0.001) and commonest between 15:00 and 18:00 (P < 0.001) and on days with wind speed less than that month’s average (P < 0.001). Nearly all victims experienced immediate pain, but this could often be controlled with ice; only 30% required parenteral narcotics and 8% required hospital admission. Cardiorespiratory arrest occurred within several minutes of the sting in the one fatal case, involving a 3-year-old girl with only 1.2 m of visible tentacle contact. C. fleckeri antivenom was given to another 21 patients, none of whom had life-threatening features at the time they were given antivenom.
Conclusions: Most C. fleckeri stings are not life-threatening; patients who die usually have cardiopulmonary arrest within minutes of the sting. The potential benefit of antivenom and magnesium under these circumstances remains to be shown, but a protocol with their rapid use is recommended if cardiopulmonary arrest has occurred. Unfortunately, this is unrealistic for many rural coastal locations, and the priority remains prevention of stings by keeping people, especially children, out of the sea during the stinger season.