Obesity is shaping up to be one of the greatest health challenges of the 21st century in Western countries. It causes a great deal of unnecessary morbidity and premature mortality, substantially reducing quality of life and increasing demand for health care services.
About 20% of Australian adults (an estimated 2.6 million) are obese (body mass index [BMI] > 30 kg/m2)1 and the incidence of obesity has doubled since 1980. The problem is especially prevalent in more disadvantaged socioeconomic groups, Aboriginal and Torres Strait Islander people and rural women.2 Alarmingly, obesity often starts in childhood — 7% of our teenagers are already obese.3
Obesity is the consummate “pathogen”. It increases the risk of type 2 diabetes, coronary heart disease, stroke, hypertension, obstructive sleep apnoea, depression, a range of cancers (including breast, gynaecological and gastrointestinal malignancies), dyslipidaemia, polycystic ovary syndrome, non-alcoholic steatohepatitis and osteoarthritis of the lower spine and weight-bearing joints. The metabolic syndrome is the paradigm of obesity disease. It is a cluster of problems centring on abdominal obesity and insulin resistance, with the key clinical manifestations being type 2 diabetes, hypertension and dyslipidaemia. It is associated with non-alcoholic steatohepatitis, obstructive sleep apnoea and polycystic ovary syndrome and affects up to one in five Australian adults.4
The US Centers for Disease Control estimated that there were 112 000 excess deaths in the year 2000 from obesity-related disease.5 Using Centers for Disease Control data, Fontaine et al6 have predicted that teenagers entering adulthood with a BMI > 40 kg/m2 have their life expectancy reduced by up to 13 years for males and 8 years for females.
Substantial weight loss has major health benefits. After major weight loss, more than two-thirds of people with type 2 diabetes no longer need treatment and return to normal fasting blood glucose, glycosylated haemoglobin (HbA1c) and serum insulin levels.7 Sixty per cent of people with obesity-associated hypertension revert to having normal blood pressure without need for treatment.8 In many people, obstructive sleep apnoea resolves,9 hypertriglyceridaemia and high-density-lipoprotein (HDL) cholesterol levels return to normal,10 and the fibrosis associated with non-alcoholic steatohepatitis improves or disappears.11 Fertility increases in women with polycystic ovary syndrome,12 and depression at least partially resolves in most people.13 In general, quality of life returns to normal14 and life expectancy improves.15 In view of these outcomes, weight loss in obese people should be a major priority of doctors, public health practitioners and politicians committed to good health care.
Prevention is the first choice. It has to be our first commitment, particularly to our children and adolescents. Unfortunately, no successful program for primary prevention has yet been established. We have a pervasive culture, reinforced by powerful commercial forces, that promotes eating and physical inactivity. To challenge this established culture will take strong political will and a multidisciplinary approach.16
Solutions that involve lifestyle change are simple to prescribe, yet rarely achieve sustainable outcomes. The bottom line is that we need to consume less energy and expend more. Although a healthy lifestyle through good eating and exercise has been promoted for many years, the problem of obesity is not only continuing but is actually increasing. A recent systematic review of the options for weight control found that there is no strong evidence of a durable effect from any current lifestyle methods.17 We should continue to seek effective lifestyle interventions, but must require evidence of benefit before embracing new options. It is encouraging that lifestyle interventions have had significant benefits (eg, improvements in diabetes control, reduced blood pressure and cholesterol levels) for some people at risk.18,19
Orlistat and sibutramine are the only two drugs that can be recommended for long-term use to achieve and maintain weight loss. Neither has been shown to induce sufficient weight loss for treating obesity, and their long-term efficacy and safety are unknown. A recent meta-analysis of pharmacological treatments for obesity showed mean weight losses, after 1 year, of 2.9 kg (95% CI, 2.3–3.5 kg) for orlistat and 4.5 kg (95% CI, 3.6–5.3 kg) for sibutramine.20 For obese individuals, who need to lose 10 kg or more, these results are suboptimal. On the horizon, rimonabant is a potential alternative. In a recent multicentre trial,21 this cannabinoid-1 receptor antagonist produced a mean weight loss of 6.6 kg (SD, 7.2 kg) after 1 year.
Endoscopic procedures do not currently play an important role in obesity treatment. Intragastric balloons were enthusiastically adopted for a period in the 1980s, until randomised controlled trials showed them to be ineffective.22 A new possibility, the BioEnterics intragastric balloon (INAMED Health, Santa Barbara, Calif), which is approved for clinical use in Australia, is yet to be proven effective in equivalent trials.
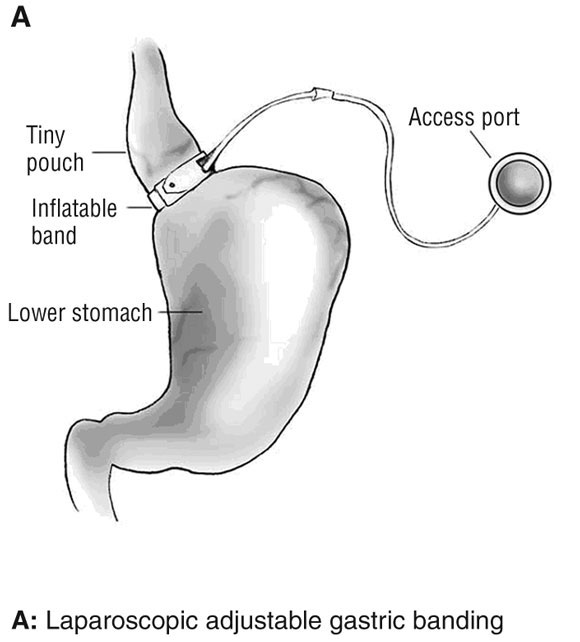
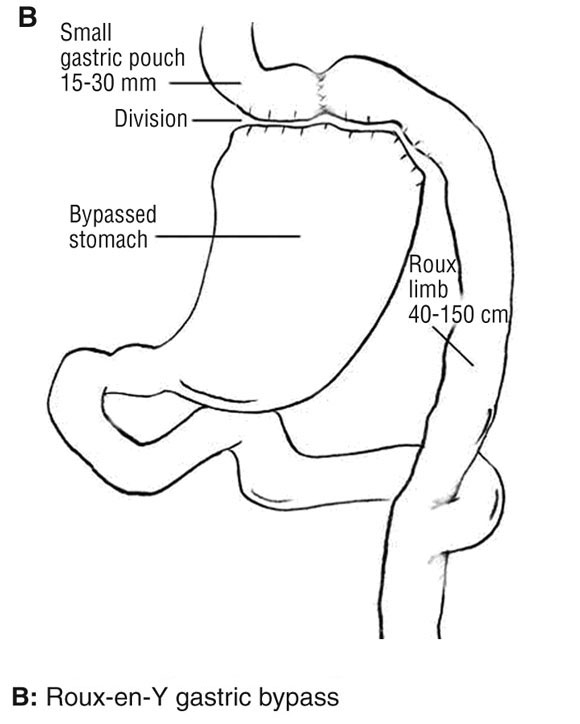
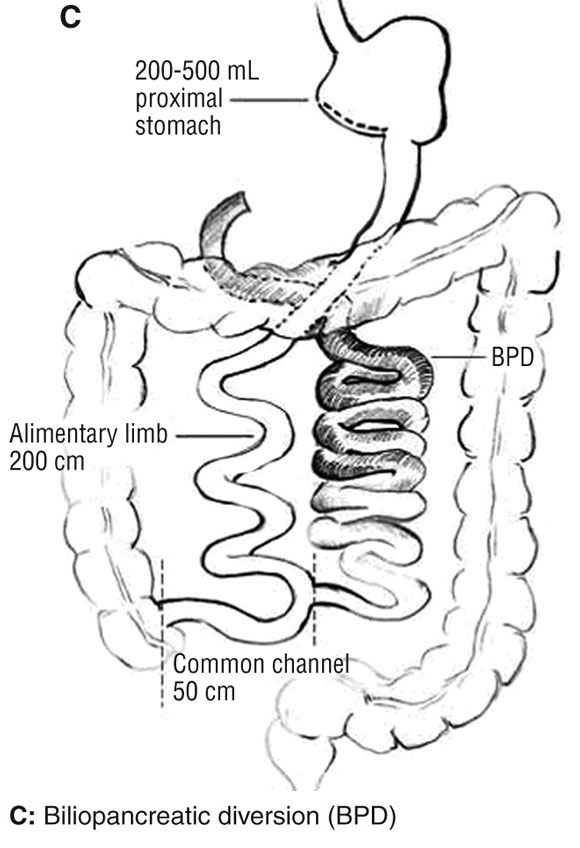
The surgical treatment of obesity (bariatric surgery) is the most rapidly growing area of surgical practice in Australia today.23 This reflects both the ability of bariatric surgical procedures to provide a solution to an otherwise insoluble problem and the evolution of safer, less invasive procedures. Today there are essentially three procedures in use: laparoscopic adjustable gastric banding (LAGB), Roux-en-Y gastric bypass (RYGB) and biliopancreatic diversion (Box 1). There is variation in preferred procedure between countries, often reflecting local regulatory and insurance factors. In Australia, LAGB is the procedure of choice in more than 90% of cases, with RYGB making up most of the rest. Health Insurance Commission data (1994–2004) for Medicare Benefits Schedule item numbers 30511 (LAGB and other gastroplasty procedures) and 30512 (RYGB) are shown in Box 2. The attributes of an ideal bariatric procedure are listed in Box 3, along with an estimate of the degree to which each procedure possesses those attributes. The key features of LAGB that have led to its acceptance are its safety, minimal invasiveness, adjustability, reversibility and overall effectiveness.
The LAGB procedure has led to a greater acceptance of bariatric surgery in Australia for a number of reasons. First, it appears to be considerably safer than the other procedures. A systematic review by the Australian Safety and Efficacy Register of New Interventional Procedures — Surgical (ASERNIP-S) found that the mean short-term mortality rate associated with LAGB was 0.05%.24 Our group has treated more than 2700 severely obese patients with the LAGB procedure since 1994 without a single perioperative death. In contrast, mortality from RYGB is reported at between 0 and 5%, with the ASERNIP-S systematic review showing a mean short-term mortality rate of 0.5% — ten times the risk of LAGB. Second, gastric band placement is minimally invasive. It is placed laparoscopically, with very little tissue dissection, and can be performed safely as a day-patient procedure.25 Third, its primary mode of effect is to induce a feeling of satiety, even in the absence of meals.26 It also has a secondary restrictive effect so that when the person does eat, there is an early feeling of fullness and very small meals will suffice. The total food intake is markedly reduced. Fourth, the LAGB is adjustable — perhaps its most important attribute. The degree of induced satiety and restriction can be controlled by an injection of saline into a subcutaneous access port during a visit to the clinic (Box 4). No other bariatric surgical option provides this important flexibility. Finally, the LAGB is easily and completely reversible, as no organs or parts thereof have been stapled or removed and no redirection of gut pathways has been created. Although there is no intention of removing the device until a better option is available, such a development may be expected in the future. It is comforting, particularly to younger patients, to know that a return to baseline is possible.
It is important to be aware of potential problems associated with LAGB. Although there are very few significant perioperative problems, late events such as prolapse of the stomach through the band, erosion of the band into the stomach and tubing breaks have led to the need for revisional surgery or removal of the band. Prolapse or slippage was more frequent in our early experience,27 but, over the past 4 years, the incidence has fallen to 4.4%. The revisional procedure is performed laparoscopically and requires an overnight stay in hospital. Erosion has become a rare event, with only four erosions (0.4%) in the last 1000 patients treated. Erosion follows a benign course and is treated laparoscopically. Tubing breaks have now almost disappeared with redesign of the access port. Overall, we have removed the band in 3.7% of our patients over a period of 10 years.
All bariatric procedures have been able to achieve loss of more than 50% of excess weight.24,27-29 The ASERNIP-S systematic review showed greater weight loss after RYGB than LAGB during the first 2 years after the procedure, but the difference in weight loss was not significant at 3 and 4 years.24 In a recent review,23 we extended the data of the ASERNIP-S review by including all studies that included at least 50 patients, reported up to March 2004 (Box 5). This showed a substantial weight loss after both procedures, with an initial greater weight loss after RYGB but similar effectiveness for both procedures at 4, 5 and 6 years.
Weight loss after bariatric surgery has a major impact on health and quality of life. No other currently available therapies are as effective in resolving a number of common and serious diseases in the severely obese.
Type 2 diabetes. Multiple studies have now demonstrated that, in association with substantial weight loss induced by bariatric surgery, more than two-thirds of patients with type 2 diabetes return to having no clinical evidence of the disease, and have normal fasting blood glucose, serum insulin and HbA1c levels without therapy. Insulin resistance is reduced and beta-cell function is improved.7,30
Hypertension. In a study of 88 patients with hypertension followed for 12 months after LAGB placement, 59% had normal blood pressure (without any treatment) and a further 33% had improved blood pressure control with less therapy.8
Dyslipidaemia. Several hundred patients with dyslipidaemia were followed for variable periods up to 4 years after LAGB placement. Serum triglyceride levels, initially elevated, returned to normal over this period. HDL cholesterol levels, which were abnormally low before weight loss, returned to normal values.10
Reflux oesophagitis. We had reported earlier on a smaller group31 but have now followed 82 patients with moderate or severe reflux oesophagitis for at least 12 months after LAGB and have achieved full control of the disease (no symptoms and requiring no therapy) in 89%, with improvement in a further 5%. Twenty-four-hour oesophageal pH studies have confirmed the reduction of reflux, and manometry has not revealed any change in oesophageal motility (unpublished data).
Asthma. All 33 patients with asthma who were followed for 1 year after LAGB showed improvement, and a third of these had no episodes of asthma and were off all therapy during the 12 months after band placement. The mean asthma severity score was reduced from 44 to 13.32
Depression. Two hundred and sixty-two patients with depression were studied before and up to 4 years after LAGB. Before the procedure, about 25% of patients fell into each of four categories — major depressive illness, moderate depression, mild depression and normal status — as measured by the Beck Depression Inventory. At 1 year, there were major reductions in the proportion of patients in each of the depression groups, with 75% of patients assessed to be normal. Four years after the procedure, the beneficial effect persisted.13
Non-alcoholic steatohepatitis, obstructive sleep apnoea and polycystic ovary syndrome. These three diseases, which are commonly found in association with insulin resistance, hypertension, type 2 diabetes and obesity, are all improved with weight loss. Out of 21 patients with non-alcoholic steatohepatitis who had repeat liver biopsies after a weight loss of over 33 kg, the disease had resolved in 19.11 Only one of 12 women who had polycystic ovary syndrome before LAGB showed continued evidence of the disease at 1-year follow-up.33 In another study, a group of 25 patients with obstructive sleep apnoea were using continuous positive airway pressure treatment before LAGB. After obesity surgery, which resulted in a mean weight loss of 45 kg, there was a mean reduction in the apnoea/hypopnoea index on polysomnography from 62 to 13, with 74% of patients no longer needing continuous positive airway pressure treatment.34
Quality of life. The Medical Outcomes Trust SF-36 health questionnaire has been used to evaluate quality of life among 459 patients before LAGB placement and annually thereafter. Scores on all eight subscales of the SF-36 were abnormally low before operation. At 1 year, scores on all subscales had returned to normal and the beneficial effect was seen to persist for at least 4 years.14
No bariatric procedure has yet been proven to fulfil all of the ideals listed in Box 3, but LAGB comes the closest and is therefore currently the initial procedure of choice in Australia. There remain several challenges. First, all bariatric surgical patients require a multidisciplinary long-term follow-up care program to obtain optimal benefit. Physicians who treat the comorbidities and general practitioners who care for the patient need to become part of the team. Second, the durability and cost-effectiveness of bariatric surgery need to be improved. Published data indicate that LAGB is effective for up to 8 years, but longer follow-up is desirable. The adjustability of LAGB gives confidence that this will happen. Third, we should seek further reduction of the need for revisional procedures that may occur some years after the initial bariatric procedure. For LAGB, the need for revisional procedures has been reduced from about 30% during our initial experience to 5% or less, but could be reduced further. Finally, we should recognise that obesity remains one of the last areas in which discrimination is regarded as acceptable. Our public hospitals and colleges continue to disregard their responsibilities for patient care and training in this area.35 As a medical community we should push these bodies to better recognise the high morbidity associated with obesity, the options for effective management and the impressive health benefits that can be achieved by weight loss.
2 Annual number of bariatric procedures performed in Australia, 1994–2004*
LAGB = laparoscopic adjustable gastric banding. RYGB = Roux-en-Y gastric bypass. * Medicare Benefits Schedule item numbers 30511 (LAGB and other gastroplasty procedures) and 30512 (RYGB) (from unpublished Health Insurance Commission data).
3 Key attributes of an ideal bariatric procedure, and assessment of each procedure against these attributes*
Attribute |
LAGB |
RYGB |
BPD |
||||||||||||
Safe |
+++ |
++ |
+ |
||||||||||||
Effective (substantial weight loss, improved health and quality of life) |
++ |
++ |
+++ |
||||||||||||
Easily and fully reversible |
Yes |
No |
No |
||||||||||||
Side effects |
+ |
++ |
++ |
||||||||||||
Durable (effective over time) |
++ |
++ |
+++ |
||||||||||||
Minimal invasiveness† |
+++ |
++ |
+ |
||||||||||||
Controllable/adjustable |
Yes |
No |
No |
||||||||||||
Low reoperation/revision rate |
+ |
+ |
+ |
||||||||||||
BPD = biliopancreatic diversion. LAGB = laparoscopic adjustable gastric banding. RYGB = Roux-en-Y gastric bypass. * Assessment levels are based on our synthesis of the published data. †+++ means the least invasive. |
|||||||||||||||
4 Two views of the 10 cm LAP-BAND LAGB system, with and without added fluid, illustrating how the feeling of satiety in the contained proximal stomach can be adjusted by adding fluid*


LAGB = laparoscopic adjustable gastric banding. * The adjustable band consists of a ring of silicone with a balloon on its inner surface connected to an access port. The ring is placed around the top of the stomach and the port is placed on the abdominal wall muscles under the skin. There are two forms of the device for which there are significant published data on effectiveness: the LAP-BAND system (Inamed Health, Santa Barbara, Calif) and the Obtech band (Ethicon Endo-Surgery, Cincinnati, Ohio).
5 A comparison of the percentage weight loss after LAGB and RYGB*
LAGB = laparoscopic adjustable gastric banding. RYGB = Roux-en-Y gastric bypass. *Based on a systematic review of all studies published before Dec 2003 that included more than 50 patients. (Reproduced with permission from O’Brien PE, Dixon JB, Brown W. Obesity is a surgical disease: overview of obesity and bariatric surgery. ANZ J Surg [Blackwell Publishing].23)
- Paul E O’Brien1
- Wendy A Brown2
- John B Dixon3
- Centre for Obesity Research and Education, Monash Medical School, Monash University, Melbourne, VIC.
Paul O’Brien has received research support (grant-in-aid) from INAMED Health and Novartis and contributions to training programs from INAMED Health. John Dixon has received research grants for clinical studies from INAMED Health and Novartis. Paul O’Brien and Wendy Brown are bariatric surgeons.
- 1. Australian Institute of Health and Welfare. Australia's health 2004. Canberra: AIHW, 2004. (AIHW Cat. No. AUS-44.)
- 2. Australian Institute of Health and Welfare. Heart, stroke and vascular disease — Australian facts 2001. Canberra: AIHW, 2001. (AIHW Cat. No. CVD-13.)
- 3. Booth ML, Wake M, Armstrong T, et al. The epidemiology of overweight and obesity among Australian children and adolescents, 1995–97. Aust N Z J Public Health 2001; 25: 162-169.
- 4. Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet 2005; 365: 1415-1428.
- 5. Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight and obesity. JAMA 2005; 293: 1861-1867.
- 6. Fontaine KR, Redden DT, Wang C, et al. Years of life lost due to obesity. JAMA 2003; 289: 187-193.
- 7. Dixon JB, O’Brien P. Health outcomes of severely obese type 2 diabetic subjects 1 year after laparoscopic adjustable gastric banding. Diabetes Care 2002; 25: 358-363.
- 8. Dixon JB, O’Brien PE. Changes in comorbidities and improvements in quality of life after LAP-BAND placement. Am J Surg 2002; 184(6B): 51S-54S.
- 9. Dixon JB, Schachter LM, O’Brien PE. Sleep disturbance and obesity: changes following surgically induced weight loss. Arch Intern Med 2001; 161: 102-106.
- 10. Dixon JB, O’Brien PE. Lipid profile in the severely obese: changes with weight loss after lap-band surgery. Obes Res 2002; 10: 903-910.
- 11. Dixon JB, Bhathal PS, Hughes NR, O’Brien PE. Nonalcoholic fatty liver disease: improvement in liver histological analysis with weight loss. Hepatology 2004; 39: 1647-1654.
- 12. Dixon J, O’Brien P. Ovarian dysfunction, androgen excess and neck circumference in obese women: changes with weight loss [abstract]. Obes Surg 2002; 12: 193.
- 13. Dixon JB, Dixon ME, O’Brien PE. Depression in association with severe obesity: changes with weight loss. Arch Intern Med 2003; 163: 2058-2065.
- 14. Dixon JB, Dixon ME, O’Brien PE. Quality of life after lap-band placement: influence of time, weight loss, and comorbidities. Obes Res 2001; 9: 713-721.
- 15. Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004; 240: 416-423.
- 16. Mullis RM, Blair SN, Aronne LJ, et al. Prevention Conference VII. Obesity, a worldwide epidemic related to heart disease and stroke. Group IV: prevention/treatment. Circulation 2004; 110: e484-e488.
- 17. Glenny AM, O’Meara S, Melville A, et al. The treatment and prevention of obesity: a systematic review of the literature. Int J Obes Relat Metab Disord 1997; 21: 715-737.
- 18. Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343-1350.
- 19. Diabetes Prevention Program Research Group. Within-trial cost-effectiveness of lifestyle intervention or metformin for the primary prevention of type 2 diabetes. Diabetes Care 2003; 26: 2518-2523.
- 20. Li Z, Maglione M, Tu W, et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med 2005; 142: 532-546.
- 21. Van Gaal LF, Rissanen AM, Scheen AJ, et al. Effects of cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet 2005; 365: 1389-1397.
- 22. Mathus-Vliegen EM, Tytgat GN, Veldhuyzen-Offermans EA. Intragastric balloon in the treatment of super-morbid obesity. Double-blind, sham-controlled, crossover evaluation of 500-milliliter balloon. Gastroenterology 1990; 99: 362-369.
- 23. O’Brien PE, Dixon JB, Brown W. Obesity is a surgical disease: overview of obesity and bariatric surgery. ANZ J Surg 2004; 74: 200-204.
- 24. Chapman A, Kiroff G, Game P, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery 2004; 135: 326-351.
- 25. Watkins BM, Ahroni JH, Erlitz MD, et al. Adjustable gastric banding in an ambulatory surgery center. Obes Surg 2005; 15: 1045-1049.
- 26. Dixon AF, Dixon JB, O’Brien PE. Laparoscopic adjustable gastric banding induces prolonged satiety: a randomized blind crossover study. J Clin Endocrinol Metab 2005; 90: 813-819.
- 27. O’Brien PE, Dixon JB, Brown W, et al. The laparoscopic adjustable gastric band (Lap-Band): a prospective study of medium-term effects on weight, health and quality of life. Obes Surg 2002; 12: 652-660.
- 28. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004; 292: 1724-1737.
- 29. Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med 2005; 142: 547-559.
- 30. Dixon JB, Dixon AF, O’Brien PE. Improvements in insulin sensitivity and beta-cell function (HOMA) with weight loss in the severely obese. Homeostatic model assessment. Diabet Med 2003; 20: 127-134.
- 31. Dixon JB, O’Brien PE. Gastroesophageal reflux in obesity: the effect of lap-band placement. Obes Surg 1999; 9: 527-531.
- 32. Dixon JB, Chapman L, O’Brien P. Marked improvement in asthma after Lap-Band surgery for morbid obesity. Obes Surg 1999; 9: 385-389.
- 33. Dixon JB, O’Brien PE. Neck circumference a good predictor of raised insulin and free androgen index in obese premenopausal women: changes with weight loss. Clin Endocrinol (Oxf) 2002; 57: 769-778.
- 34. Dixon JB, Schachter LM, O’Brien PE. Polysomnography before and after weight loss in obese patients with severe sleep apnea. Int J Obes Relat Metab Disord 2005; Apr 19 [Electronic publication ahead of print].
- 35. Talbot ML, Jorgensen JO, Loi KW. Difficulties in provision of bariatric surgical services to the morbidly obese. Med J Aust 2005; 182: 344-347. <MJA full text>





Abstract
Obesity is shaping up to be the major health care problem and one of the most frequent causes of preventable death in Western countries in the 21st century.
Bariatric surgery is the only current treatment that has been shown to achieve major and durable weight loss.
Major weight loss in the severely obese leads to total or partial control of a wide range of common and serious diseases, such as diabetes, heart disease and hypertension.
Laparoscopic adjustable gastric banding is the most common type of obesity surgery performed in Australia. It is effective, relatively safe and minimally invasive.
The blocks to broader application of bariatric surgery should be identified and resolved.