Multiple, evidence-based guidelines worldwide have indicated how acute low back pain should be managed.1 These are soon to be complemented by Australian guidelines, one set developed by the Royal Australian College of General Practitioners and another by the Acute Musculoskeletal Guidelines Group. These guidelines emphasise effective communication with the patient to provide explanation and assurance, allay fears, promote activity and avoid passive therapies. Followed conscientiously, these guidelines are safe, effective and cost-effective. Over 70% of patients can expect to become pain-free, with a recurrence rate of less than 25%.2
For chronic low back pain, the situation is entirely different. By definition, this is pain that has persisted for longer than 3 months.3 In addition to the pain, patients typically suffer physical disabilities and psychological distress. They may be unable to work and depressed. No organisation has developed evidence-based guidelines for chronic low back pain. Yet evidence is not lacking. This article cites evidence distilled in two monographs,3,4 supplemented by later systematic reviews (Box 1).
The prevailing approaches to chronic low back pain fall into three categories: monotherapies, multidisciplinary therapy, and reductionism.3
Monotherapies are interventions of a single, particular kind that a medical practitioner might prescribe as sole treatment. Some might be used simultaneously, but there is no evidence that such combinations are more effective than monotherapies used alone.
Paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) may be of short-term benefit, but no published data vindicate their long-term use for chronic low back pain.3,5,6 Intriguingly, willow bark has been shown to be superior to placebo and as effective as NSAIDs for treating relapses of recurrent low back pain.24,25
Opioids are more effective than naproxen or placebo for relieving chronic low back pain,26 but the average effect is little more than a 10-point reduction on a 100-point scale.7,26 Nor do they improve the psychological or functional status of patients treated.7
Antidepressants are slightly more effective than placebo for relief of chronic low back pain, but have not been tested for longer than 8 weeks.8 They provide only partial relief, and their utility is limited by side effects. Some muscle relaxants (eg, cyclobenzaprine) are effective for short-term relief, but are not available in Australia.9
Orthoses, transcutaneous electrical nerve stimulation (TENS), and electromyographic biofeedback show no evidence of efficacy.3,5
Traction, acupuncture, magnet therapy, injections into trigger points, and hydrotherapy are no more effective than sham treatment, placebo, or being put on a waiting list.3,5,27,28
Manipulative therapy was found in the latest meta-analysis to be slightly more effective than sham therapy (by 4 points on a 100-point scale), but not more effective than other forms of care, including care by a general practitioner, physiotherapy or exercises, “back school”, or therapies known to be ineffective.10 A contemporary review echoed these findings.27
Massage is a relative newcomer as a scientifically tested treatment for chronic low back pain. Three controlled trials show that it is more effective than sham therapy, self-care educational materials, acupuncture, muscle relaxation and remedial exercises.27
Botulinum toxin is more effective than placebo at 8 weeks, but no long-term studies have been conducted.29
Prolotherapy (the injection of sclerosing agents into tender ligaments) has given mixed results in the past,3 but was found in a recent study to be no more effective than placebo.30 However, even the placebo treatment (injecting normal saline into tender points) achieved complete relief of pain that was sustained at 12 months in 20% of patients, and more than 50% relief of pain in just under half of all patients.
Behavioural therapy is better than no therapy and better than placebo, but it is not better than exercise therapy, and provides no additional benefit when added to other interventions.3,31 Although some systematic reviews have concluded that back school is effective, this has been in the context of multidisciplinary treatment.3,5
Exercise therapy is more effective than usual care by a GP,32 and better than back school; but the evidence is conflicting on whether exercise is more effective than an inactive, sham treatment.3,5,11 There is strong evidence that strengthening exercises are not more effective than other types of exercises.11
Surgery for back pain lacks compelling evidence of efficacy.3,33 The one controlled study showed it to be more effective than physical therapy, with more than 60% of patients feeling “much better” or “better” after surgery, compared with 30% of patients treated with physical therapy.12 However, surgery was not curative; mean pain scores (on a 100-point scale) fell from 64 at baseline to 30 at 6 months, but reverted to 43 by 2 years.12 Mean pain scores for patients treated with physical therapy did not differ from baseline at any time.
Spinal cord stimulation and intraspinal opioids are sometimes used to treat patients whose back pain has not responded to surgery. Their use is sustained only by consensus views based on descriptive studies.34 Similarly, no data vindicate epidural lysis of adhesions.35
There is no universal definition of multidisciplinary therapy. In the literature and in practice, it comprises various combinations of exercises, education and behavioural therapy. When work-hardening is emphasised, it has been called functional restoration.3 A distinguishing characteristic of all programs is that they address physical disabilities and patients’ beliefs about their pain and resulting behaviour. Pain relief is not an overt objective. Nor are a diagnosis and specific anatomical treatment pursued.
While proponents of multidisciplinary therapy have published favourable reviews of its efficacy for chronic pain in general,36 a review focusing on chronic low back pain was less encouraging.13 There is strong evidence that intensive multidisciplinary biopsychosocial rehabilitation with functional restoration improves function, and moderate evidence that it reduces pain, when compared with outpatient non-multidisciplinary rehabilitation or usual care. The evidence is contradictory on its effect on return to work. However, these conclusions apply to intensive rehabilitation, which means intensive exercises. The available trials of less intensive multidisciplinary rehabilitation did not show improvements in pain, function, or vocational outcomes when compared with non-multidisciplinary outpatient rehabilitation or usual care.13
Although intensive rehabilitation is more effective than some other interventions, outcomes are variable and limited.3 One study found that this type of rehabilitation reduced disability scores from 15.5 (on a 30-point scale) to 8.5 at 4 months, yet another study from the same institution found that it improved disability scores from 16.9 (also on a 30-point scale) to only 12.1. In these studies, pain scores were reduced from 5.3 (on a 10-point scale) to 2.7, and from 6.1 to 5.7, respectively. Another study found that pain scores were reduced by only 17 points on a 100-point scale. In these terms, multidisciplinary therapy cannot be regarded as curative. For some patients, it offers the possibility of better pain control and improved function, but overall it amounts only to palliative therapy.3
Reductionism describes the pursuit of a pathoanatomical diagnosis for chronic low back pain with the view to implementing a target-specific treatment.3 In this regard it differs from monotherapies and multidisciplinary therapy, neither of which requires a classical diagnosis to be established. Pursuing a cure has been criticised on the grounds that it ignores the psychosocial aspects of chronic pain. Nevertheless, proponents of reductionism have persisted, as monotherapies and multidisciplinary therapy have not provided a satisfying solution to chronic low back pain.
In most cases, causes for chronic low back pain cannot be found using conventional investigations, such as radiography and magnetic resonance imaging (MRI), with fewer than 10% of cases diagnosed by these means.3 Degenerative changes and conditions such as spondylolysis and spondylolisthesis are not valid diagnoses of the cause of pain, as they are no more common in patients with pain than in asymptomatic individuals.3
However, sources and causes of chronic low back pain can be established if less conventional investigations are used (Box 2):
Joint blocks can be used to pinpoint pain from the sacroiliac joint or the lumbar zygapophysial joints.3
Provocation and computed tomography (CT) discography can be used to diagnose discogenic pain and internal disc disruption.3 The latter differs from disc herniation. It is characterised by radial and circumferential fissures in the anulus fibrosus of the affected disc, in association with a degraded nuclear matrix; externally the disc is intact.3 This condition is not related to degeneration or age changes,37 but appears to be caused by fatigue failure of the vertebral endplate after repeated loading.38
When diagnostic joint blocks are used, the source of pain can be traced to the sacroiliac joint in about 20% of patients,14 while lumbar zygapophysial joint pain is found in about 15% of injured workers,15 and as many as 40% of people with chronic back pain in older populations.16 CT discography reveals internal disc disruption in at least 40% of patients.17 These figures belie the assertion that 80% of patients with chronic low back pain cannot be diagnosed. This is true if investigations are limited to CT or MRI, but a diagnosis becomes possible if diagnostic blocks and discography are used.
These investigations are not indicated for every patient with chronic low back pain. They are indicated if there is a desire or need to know. They have diagnostic utility in that they bring about closure. They prevent the futile pursuit of a diagnosis by other non-valid means. They may have a beneficial psychological effect; patients may be relieved to have an explanation for their pain. For medicolegal purposes, establishing a diagnosis under controlled conditions protects patients from accusations of malingering or imagining their pain.
The ultimate measure of a diagnostic test is its therapeutic utility. In the past, pursuing a pathoanatomical diagnosis of low back pain could be criticised on the grounds that the diagnosis did not alter treatment. This is no longer the case.
Zygapophysial joint pain can be treated with radiofrequency medial branch neurotomy.3,18,19 A controlled trial has shown that this treatment is not a placebo,18 and an observational study has shown that, provided patients are carefully selected using controlled diagnostic blocks, and provided a correct surgical technique is used, some 60% of patients can expect at least 80% relief of their pain at 12 months, and 80% of patients can expect at least 60% relief.19
For sacroiliac joint pain, there is no established, proven treatment, but therapies involving denervation of the joint are emerging.20
For internal disc disruption, the mainstay of treatment has been arthrodesis. However, the hazards of this major surgery, and its questionable efficacy, have prompted the exploration of minimally invasive alternatives. One of these has been intradiscal electrothermal therapy (IDET), in which the fissures of the painful disc are coagulated percutaneously with flexible electrodes introduced into the disc. Launched on the basis of observational studies, this treatment became controversial for lack of controlled trials. One study has now shown that IDET is more effective than physical rehabilitation;21 and a forthcoming study found it to be significantly more effective than placebo for relieving pain and improving function.22 However, IDET is not a panacea for chronic low back pain. It is indicated only for patients with proven internal disc disruption, but even then fails to provide any benefit in 50% of cases. Nevertheless, some 20% of patients can obtain complete relief of pain, sustained at 2 years, and a further 30% obtain greater than 50% relief, associated with return to work.33
Patients with chronic low back pain who fail to benefit from surgery can be difficult to treat. These patients have generally been treated with multidisciplinary therapy, spinal cord stimulation or intraspinal opioids. Although some patients can benefit from each of these approaches, they have not been universally successful.
The prevailing attitude to patients with failed back surgery syndrome has been that it is futile to pursue a pathoanatomical diagnosis. Recent studies are reversing that attitude. If carefully investigated, a treatable lesion can be found in substantial proportions of these patients.39 In those who have predominantly leg pain, unrecognised lateral stenosis is the most common cause. In those who have predominantly back pain, the most common cause is unrecognised internal disc disruption. Such findings are grounds for optimism that, in the future, patients with failed back surgery need not be relegated to symptomatic treatment only.
The evidence on treatment of chronic low back pain leaves GPs with few options. Established treatments either do not work or have limited efficacy. Emerging treatments may still be regarded as controversial, or are not widely available.
The evidence indicates that prescribing analgesics, tricyclic antidepressants and muscle relaxants is not the answer; nor is sending the patient for more physiotherapy or manipulative therapy. Nevertheless, some guidance can be formulated (Box 3). Information for patients is summarised in Box 4.
For exacerbations of chronic low back pain, the evidence supports the use of willow bark. Massage is emerging as an innocuous but effective intervention that is commonly available. Injections into tender attachment sites for ligaments are a simple treatment that GPs can perform. The agent used is immaterial; even normal saline works if the injection is given with confidence. They can achieve complete relief of pain in 20% of patients and significantly reduce pain in 40%.30 These figures are no worse than those for the best alternatives, and better than most.
If a diagnosis is required, diagnostic blocks and discography can be undertaken. This should be in consultation with a practitioner experienced in the technique and interpretation of results. If treatment is to follow, it should be in the hands of an experienced practitioner of the technique.
If a diagnosis is not required or is not possible, the current mainstay of management is multidisciplinary therapy. The evidence requires that this be a program based on intensive exercises, as less intensive programs are not effective. Even so, neither GPs nor patients should be under the misapprehension that multidisciplinary therapy will be curative. While some patients may have outstanding responses, most will benefit only partially with respect to function and pain.
Opioids may be needed for patients with persistent severe pain, but should be used carefully. Patients must understand that they will not be cured of their pain; relief will be only partial. Opioid therapy is best undertaken under the aegis of a pain clinic, or according to published guidelines if a pain clinic is not available.40,41
Although not proven in controlled trials, spinal cord stimulation or intrathecal opioids constitute a final option for patients with intractable back pain, particularly after failed surgery. They are costly but provide appreciable relief for up to 50% of those treated.
1: Evidence-based practice points*
There is no evidence of long-term efficacy for drug therapy with analgesics, non-steroidal anti-inflammatory drugs, muscle relaxants or antidepressants for treatment of chronic low back pain (E1); 5-7 opioids are only partially effective and do not improve function (E2).8,9
Orthoses, transcutaneous electrical nerve stimulation, electromyographic biofeedback, traction, acupuncture, magnet therapy, injections into trigger points, and hydrotherapy are no more effective than sham therapy (E1); 3,5 manipulative therapy is barely more effective than sham therapy (E1).10
While exercise therapy is more effective than other interventions, it has also not been shown to be better than sham therapy (E1).11
Surgery is more effective than physiotherapy, but outcomes are modest (E2).12
Multidisciplinary therapy based on intensive exercises improves physical function but has modest effects on pain (E1).13
Conventional investigations do not reveal the cause of pain (E1),3 but diagnostic joint blocks and discography can provide a diagnosis in many cases (E2).14-17
Between 15% and 40% of patients have zygapophysial joint pain (E2); 3,15,16 about 20% have sacroiliac joint pain (E2),3,14 and over 40% have internal disc disruption (E2).17
Zygapophysial joint pain can be relieved by radiofrequency neurotomy (E2, E3),18,19 and techniques are emerging for treating sacroiliac joint pain and internal disc disruption (E2, E3, E4).20-22
* Grading of evidence is based on the system of the National Health and Medical Research Council:23 E1 Evidence obtained from a systematic review of all relevant randomised controlled trials; E2 Evidence obtained from at least one properly designed randomised controlled trial; E3 Evidence obtained from pseudorandomised controlled trials or comparative studies; and E4 Evidence obtained from case series, either post-test or pre-test and post-test.
2: Diagnostic and treatment methods for chronic low back pain
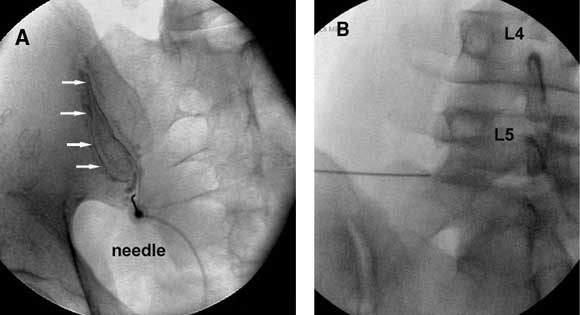
Joint blocks Joints thought to be the source of pain can be anaesthetised by injecting local anaesthetic into the joint (Figure A) or by blocking the nerves that supply the joint (Figure B). |
|||||||||||
 |
|||||||||||
A: Oblique anteroposterior radiograph of a sacroiliac arthrogram. A needle has been inserted into the cavity of the sacroiliac joint and contrast medium (arrows) injected to confirm intra-articular placement, before injection of local anaesthetic (image kindly provided by Dr Paul Dreyfuss, Seattle, Washington). B: Anteroposterior radiograph showing a needle in place for a left L5 medial branch block. |
|||||||||||
Provocation discography (Figure C) To test if a particular intervertebral disc is painful, contrast medium is injected into the disc to distend it. The disc is deemed to be the source of pain if the patient’s accustomed pain is reproduced at low pressure of injection, provided that stimulation of adjacent discs does not reproduce pain. Computed tomography discography (Figure D) After a discogram has been performed, the internal architecture of the disc can be demonstrated by computed tomography (CT). Radial fissures correlate strongly with the disc being painful. |
|||||||||||
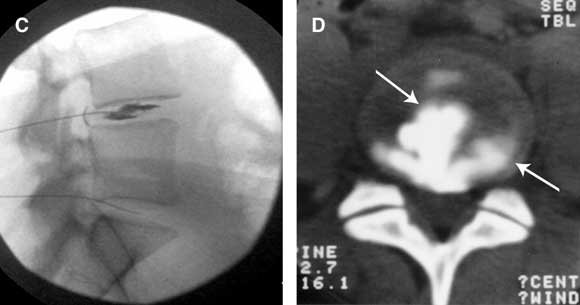 C: Lateral radiograph of an L4–L5 discogram, showing needles placed in the L4–L5 and L5–S1 intervertebral discs and contrast medium injected into the L4–L5 disc. D: Post-discography CT scan of (a painful) L4–L5 intervertebral disc. Contrast medium outlines a radial and a circumferential fissure (arrows), diagnostic of internal disc disruption. |
|||||||||||
4: Messages for patients with chronic low back pain
Drug treatment does not cure back pain.
Opioids only partially relieve the pain and must be used carefully.
Willow bark is effective therapy for exacerbations of pain.
Massage can help relieve pain.
Manipulative therapy is barely more effective than sham treatment, and other physical therapies and devices are no more effective than sham treatment.
Exercises can be beneficial.
Multidisciplinary therapy can help improve function, but will not completely cure pain.
Surgery can help some patients to various degrees, but nearly half will not benefit.
Spinal cord stimulators can help some patients who gain no relief from surgery.
Tests are available to make a diagnosis when CT scans and MRI scans are said to be normal.
Treatment is available for zygapophysial joint pain.
New treatments are being developed and tested for sacroiliac joint pain and pain coming from intervertebral discs.
CT = computed tomography. MRI = magnetic resonance imaging.
- Nikolai Bogduk1
- Newcastle Bone and Joint Institute, Royal Newcastle Hospital, Newcastle, NSW.
None identified.
- 1. Koes BW, can Tulder M, Ostelo R, et al. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine 2001; 26: 2504-2513.
- 2. McGuirk B, King W, Govind J, et al. The safety, efficacy, and cost-effectiveness of evidence-based guidelines for the management of acute low back pain in primary care. Spine 2001; 26: 2615-2622.
- 3. Bogduk N, McGuirk B. Medical management of acute and chronic low back pain: an evidence-based approach. Amsterdam: Elsevier, 2002.
- 4. Nachemson A, Jonsson E, editors. Neck and back pain: the scientific evidence of causes, diagnosis, and treatment. Philadelphia: Lippincott, Williams and Wilkins, 2000.
- 5. van Tulder MV, Goossens M, Waddell G, Nachemson A. Conservative treatment of chronic low back pain. In: Nachemson A, Jonsson E, editors. Neck and back pain: the scientific evidence of causes, diagnosis, and treatment. Philadelphia: Lippincott, Williams and Wilkins, 2000: 271-304.
- 6. van Tulder MW, Scholten RJPM, Koes BW, Deyo RA. Nonsteroidal anti-inflammatory drugs for low back pain. A systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2000; 25: 2501-2513.
- 7. Moulin DE, Iezzi A, Amireh R, et al. Randomised trial of oral morphine for chronic non-cancer pain. Lancet 1996; 347: 143-147.
- 8. Salerno S, Browning R, Jackson SL. The effect of antidepressant treatment of chronic back pain. A meta-analysis. Arch Intern Med 2002; 162: 19-24.
- 9. van Tulder MW, Touray T, Furlan AD, et al. Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration. Spine 2003; 28: 1978-1992.
- 10. Assendelft WJJ, Morton SC, Yu EI, et al. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann Intern Med 2003; 138: 871-881.
- 11. van Tulder M, Malmivaara A, Esmail R, Koes B. Exercise therapy for low back pain. A systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2000; 21: 2784-2796.
- 12. Fritzell P, Hagg O, Wessberg P, Nordwall A, Swedish Lumbar Spine Study Group. 2001 Volvo award winner in clinical studies: lumbar fusion versus nonsurgical treatment for chronic low back pain. A multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine 2001; 26: 2521-2534.
- 13. Guzman J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic back pain: systematic review. BMJ 2001; 322: 1511-1516.
- 14. Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low-back pain. Spine 1996; 21: 1889-1892.
- 15. Schwarzer AC, Aprill CN, Derby R, et al. Clinical features of patients with pain stemming from the lumbar zygapophysial joints. Is the lumbar facet syndrome a clinical entity? Spine 1994; 19: 1132-1137.
- 16. Schwarzer AC, Wang S, Bogduk N, et al. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis 1995; 54: 100-106.
- 17. Schwarzer AC, Aprill CN, Derby R, et al. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine 1995; 20: 1878-1883.
- 18. van Kleef M, Barendse GAM, Kessels A, et al. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine 1999; 24: 1937-1942.
- 19. Dreyfuss P, Halbrook B, Pauza K, et al. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine 2000; 25: 1270-1277.
- 20. Cohen SP, Salahadin A. Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med 2003; 28: 113-119.
- 21. Bogduk N, Karasek M. Two-year follow-up of a controlled trial of intradiscal electrothermal anuloplasty for chronic low back pain resulting from internal disc disruption. Spine J 2002; 2: 343-350.
- 22. Pauza KJ, Howell S, Dreyfuss P, et al. A randomized, placebo-controlled trial of intradiscal electrothermal therapy (IDET) for discogenic low back pain. Spine J 2004. In press.
- 23. National Health and Medical Research Council. A guide to the development, implementation and evaluation of clinical practice guidelines. Canberra: NHMRC, 1999: 56.
- 24. Chrubasik S, Eisenberg E, Balan E, et al. Treatment of low back pain exacerbations with willow bark extract: a randomized double-blind study. Am J Med 2000; 109: 9-14.
- 25. Chrubasik S, Kunzel O, Model A, et al. Treatment of low back pain with a herbal or synthetic anti-rheumatic: a randomised controlled study. Willow bark extract for low back pain. Rheumatology 2001; 40: 1388-1393.
- 26. Jamison RN, Raymond SA, Slawsby EA, et al. Opioid therapy for chronic noncancer back pain. A randomized prospective study. Spine 1998; 23: 2591-2600.
- 27. Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain. Ann Intern Med 2003; 138: 898-906.
- 28. McIlveen B, Robertson V. A randomized controlled study of the outcome of hydrotherapy for subjects with low back or back and leg pain. Physiotherapy 1998; 84: 17-26.
- 29. Foster L, Clapp L, Erickson M, Jabbari B. Botulinum toxin A and chronic low back pain. A randomized, double-blind study. Neurology 2001; 56: 1290-1293.
- 30. Yelland M, Glasziou P, Bogduk N, et al. Randomised controlled trial of prolotherapy injections, saline injections and exercises in the treatment of chronic low back pain. Spine 2003. In press.
- 31. van Tulder MW, Ostelo R, Vlaeyen JWS, et al. Behavioral treatment for chronic back pain. A systematic review within the framework of the Cochrane Back Review Group. Spine 2000; 25: 2688-2699.
- 32. O’Sullivan PB, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 1997; 22: 2959-2967.
- 33. Waddell G, Gibson A, Grant I. Surgical treatment of lumbar disc prolapse and degenerative lumbar disc disease. In: Nachemson A, Jonsson E, editors. Neck and back pain: the scientific evidence of causes, diagnosis, and treatment. Philadelphia: Lippincott, Williams and Wilkins, 2000: 305-325.
- 34. Bennett G, Serafini M, Burchiel K, et al. Evidence-based review of the literature on intrathecal delivery of pain medication. J Pain Symptom Manage 2000; 20: S12-S36.
- 35. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anaesth Pain Med 1999; 24: 202-207.
- 36. Flor H, Fydich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain 1992; 49: 221-230.
- 37. Moneta GB, Videman T, Kaivanto K, et al. Reported pain during lumbar discography as a function of anular ruptures and disc degeneration. A re-analysis of 833 discograms. Spine 1994; 17: 1968-1974.
- 38. Adams MA, McNally DS, Wagstaff J, Goodship AE. Abnormal stress concentrations in lumbar intervertebral discs following damage to the vertebral bodies: cause of disc failure? Eur Spine J 1993; 1: 214-221.
- 39. Waguespack A, Schofferman J, Slosar P, Reynolds J. Etiology of long-term failures of lumbar spine surgery. Pain Med 2002; 3: 18-22.
- 40. Graziotti PJ, Goucke CR. The use of oral opioids in patients with chronic non-cancer pain. Management strategies. Med J Aust 1997; 167: 30-31. <MJA full text>
- 41. Canadian Pain Society. Use of opioid analgesia for the treatment of chronic non-cancer pain – a consensus statement and guidelines from the Canadian Pain Society. Pain Res Manage 1998; 3: 197-208.





Abstract
Treatment for chronic low back pain (pain persisting for over 3 months) falls into three broad categories: monotherapies, mulitidisciplinary therapy, and reductionism.
Most monotherapies either do not work or have limited efficacy (eg, analgesics, non-steroidal anti-inflammatory drugs, muscle relaxants, antidepressants, physiotherapy, manipulative therapy and surgery).
Multidisciplinary therapy based on intensive exercises improves physical function and has modest effects on pain.
The reductionist approach (pursuit of a pathoanatomical diagnosis with the view to target-specific treatment) should be implemented when a specific diagnosis is needed.
While conventional investigations do not reveal the cause of pain, joint blocks and discography can identify zygapophysial joint pain (in 15%–40%), sacroiliac joint pain (in about 20%) and internal disc disruption (in over 40%).
Zygapophysial joint pain can be relieved by radiofrequency neurotomy; techniques are emerging for treating sacroiliac joint pain and internal disc disruption.