Not only is Indigenous health in Australia poor,1-4 "there is widespread agreement that knowledge about the health status of the Aboriginal population is inadequate".5 Some Indigenous health research has been of immense use in designing and evaluating interventions which have improved the health status of Indigenous people, especially at the local level.6,7 Consequently, high-quality, proactive, participatory research is needed.8,9
Because there are few Indigenous healthcare professionals and researchers in Australia, non-Indigenous researchers are involved in Indigenous research. Ensuring these researchers work in culturally appropriate and non-exploitative ways is a key concern.2,10,11 This article documents an approach that developed a partnership between researchers and Koorie communities in parts of northern Victoria and southern New South Wales. It extends previous guidelines about general research issues (cultural beliefs, language, privacy and questioning approaches)12,13 by describing how community research has been appropriately undertaken. This is more innovative, comprehensive and in addition to agreements between specific Indigenous organisations and researchers,14 for it develops a culturally sensitive and outcome-based policy for non-Indigenous researchers before partnerships are entered into.
The multidisciplinary Department of Rural Health (DRH), University of Melbourne, was established in 1999. One of its three objectives is to assist in reducing the health differential between Indigenous and non-Indigenous people.15,16 The DRH was sited in Shepparton, partly because the area has the largest Indigenous population in Victoria outside Melbourne (estimated 6000 Indigenous residents).17 This includes communities in Shepparton/Mooroopna, Barmah/Cummeragunja, Echuca/Moama, Kerang, Swan Hill and Albury/Wodonga. One community is a small town of mostly Aboriginal residents, and the others have Indigenous residents living among the non-Indigenous population. These communities have high rates of diabetes, heart disease and depression (about 40%–50% for each), compounded by huge rates of unemployment, very low completion of high school, alcohol and drug issues, low incomes and low self-esteem.18,19 Exact rates for many of these are lacking at the community level and it is likely that many unidentified health issues also exist.
Indigenous communities in this region have had negative experiences with research projects due to the lack of community control, lack of local benefits, and interpretation of data in isolation from social context.9,13,20 Therefore, a framework was developed to build a partnership between local Indigenous communities and the new academic department.
The Koorie Health Partnership Committee (Box 1) was established in 1999. All Koorie organisations in the region were invited to join the committee, which meets bi-monthly to identify health priorities, develop specific projects and review the activities of the DRH, communities and individual organisations. The committee has initiated projects on topics including cross-cultural issues, workforce, and a "bush tucker" project in which nutritional, cultural and legal aspects of traditional foods can be examined. Members of the partnership committee have also been on selection committees for new appointments to the department and acted as advisers to the Koorie Team.
The partnership committee recognised the need for written protocols to guide non-Indigenous members of the DRH in working within Koorie communities. In consultation, the Koorie Team developed guidelines to ensure that members of the DRH are informed of appropriate actions and negotiation within Koorie communities and organisations. The guidelines are also intended to develop trust, reinforce the integrity of the DRH and maintain robust relationships with local communities that can withstand some difficulties (eg, funding that only partially meets partnership committee objectives). The guidelines also protect non-Indigenous researchers, maintaining their neutrality.
The guidelines are based on general research guidelines, the National Health and Medical Research Council (NHMRC) Guidelines on Ethical Matters in Aboriginal and Torres Strait Islander Health Research,13 and the input of researchers and the partnership committee.
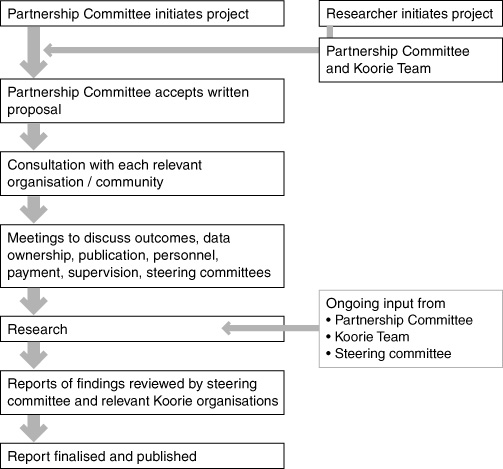
The DRH framework means that research is undertaken with consultation before, during and after the project (Box 2). Usually a Koorie research assistant is employed to assist with consultation and data collection and analysis. Payment of study participants and steering committee members has not been common, but research assistants and project officers are paid.
Although the process appears straightforward, the complexity cannot be overstated. For example, different Koorie organisations often have different expectations of outcomes, and levels of involvement, interest and commitment. Because of the holistic nature of such research, many organisations are usually involved, with unclear boundaries and changing requests. Further, the guidelines sometimes challenge scientific procedures or call for researchers to negotiate sampling, data collection techniques and presentation of results.
The usual university ethics approval is still required.21,22 Ethics committees have agreed on requirements to date, including steering committees, employing Koories, storage of data with the Koorie Team, written consent, the role of the partnership committee, ongoing consultation and approval of all reports. Our framework extends general ethical requirements, calling for research to be culturally sensitive and accepted as necessary and useful by the communities of the participants. This gives communities the power to decide what research should be undertaken, a voice on how research is conducted, and control over presentation of the findings.
Participatory research is increasingly being used in a variety of settings among indigenous communities in Canada, the United States, Sweden, South Africa and New Zealand.2,12,23-25 The approach presented here, in conjunction with others,9,13 should provide a positive starting point for negotiation between Indigenous communities and researchers in other regions of Australia.
Rather than develop one-off Koorie research projects, the DRH has developed a framework to promote partnership with Koorie communities in research, education, employment and community development. This framework reflects the Indigenous holistic view of health and the relationship between physical health outcomes, the social determinants of health and the need to respect the integrity of each Indigenous community. Most importantly, ongoing negotiations allow flexibility within the guidelines — they are adapted to each project and allow for the development of new phases and extensions to previous projects.
As relationships between DRH and Koorie communities have strengthened, the workload for the partnership committee and Koorie Team has increased dramatically. Including Koories in most health research has meant the partnership committee and Koorie Team are involved in most research at the DRH. In addition, despite inclusive processes and openness of information, local political and family histories still raise issues. The partnership committee, Koorie Team and researchers can find themselves between conflicting family groups or perceived to favour some families or organisations over others. The challenge for outsiders to understand and address this, and for insiders to work between them while living in these communities, remains.
The growth and use of evidence for developing and implementing sustainable interventions to improve Indigenous health is urgently required. Our framework addresses the key concern of undertaking this while respecting history and Indigenous cultures.
1: Organisations in the Koorie Health Partnership Committee
Allinjarra Aboriginal Cooperative (Kerang): Cultural centre with a range of support and healthcare programs.
Bangerang Cultural Centre (Shepparton): Keeping Place, cultural centre, community education for Koorie and other communities.
Department of Rural Health, University of Melbourne (Shepparton): Research, university education, training, community development.
Goulburn Valley Aboriginal Women's Resource Group (Shepparton): Koorie women's group to provide support, information and develop women's programs.
Koorie Economic Employment and Training Agency (Shepparton): Training and employment program with non-Indigenous businesses/organisations.
Local Aboriginal Education Consultative Group (Shepparton): Works with primary and secondary schools to support Koorie students. Offers preschool and daycare.
Mungabareena Aboriginal Cooperative (Wodonga): Cultural centre with a range of support and health care programs.
Rumbalara Football Netball Club (Shepparton): Football and netball club participating in 'mainstream' league; also runs a health promotion program.
Rumbalara Aboriginal Cooperative (Mooroopna): Cultural centre with a range of support programs and an Aboriginal Health Service.
Savina Morgan Health Centre (Cummeragunja): Aboriginal Health Service.
Swan Hill and District Aboriginal Co-operative (Swan Hill): Cultural centre with a range of support and health care programs.
- Rick Henderson1
- David S Simmons2
- Lisa Bourke3
- Janice Muir4
- Department of Rural Health, University of Melbourne, Melbourne, VIC.
All the authors acknowledge the Koorie Health Partnership Committee (Box 1). The authors would also like to acknowledge the intellectual and cultural input from the Koorie communities who have worked with the DRH to improve health. Rick and Jan acknowledge our respective countries and connections, to Rick's Elders and ancestors of his mother's people, the Wiradjuri, and his father's, the Yorta Yorta. Jan recognises and respects the earth our mother, homage to Biami our creator and acknowledges her ancestors, Elders from her mother's people, the Nurundjeri, and her father's family connections with the Waddi Waddi and Yorta Yorta nations.
- 1. Australian Institute of Health and Welfare. The health and welfare of Australia's Aboriginal and Torres Strait Islander peoples. Canberra: Australia Bureau of Statistics, 1997. (ABS Catalogue no. 4704.0.)
- 2. O'Donoghue L. Towards a culture of improving Indigenous health in Australia. Aust J Rural Health 1999; 7: 64-69.
- 3. Dodson M. Aboriginal and Torres Strait Islander social justice commission first report. Canberra: AGPS, 1993; 119.
- 4. Ring IT, Firman D. Reducing indigenous mortality in Australia: lessons from other countries. Med J Aust 1998; 169: 528-533.
- 5. Victorian Aboriginal Community Controlled Health Organisation Incorporated, Department of Human Services Victoria. Achieving improved Aboriginal health outcomes: an approach to reform. Melbourne: Public Health Division, Department of Human Services, Victoria, 1996; 3.
- 6. Wronski I. The growth and development of under 5 Aboriginal children in Shepparton/Mooroopna. Victoria: Health Commission of Victoria, 1980.
- 7. VicHealth Koori Health Research and Community Development Unit. We don't like research . . . but in Koori hands it could make a difference. Melbourne: VicHealth Koori Health Research and Community Development Unit, 2000.
- 8. Doyle MJ. The Rumbalara eye care project: primary, secondary and tertiary prevention of eye disease in an Aboriginal community. Proceedings of the 28th Annual conference of the Public Health Association of Australia, 1996; 65.
- 9. Eades SJ, Read AW, Bibbulung Gnarneep Team. The Bibbulung Gnarneep Project: practical implementation of guidelines on ethics in Indigenous health research. Med J Aust 1999; 170: 433-436.
- 10. Donovan RJ, Spark R. Towards community guidelines for survey research in remote Aboriginal communities. Aust N Z J Public Health 1997; 21: 89-95.
- 11. Maher P. A review of 'traditional' Aboriginal health beliefs. Aust J Rural Health 1999; 7: 229-236.
- 12. Golds M, King R, Meiklejohn B, et al. Healthy Aboriginal communities. Aust N Z J Public Health 1997; 21: 386-390.
- 13. National Health and Medical Research Council. Guidelines on ethical matters in Aboriginal and Torres Strait Islander health research. Canberra: NHMRC, 1991.
- 14. Legal agreement between the Tiwi Health Board and Menzies School of Health Research. 1988. <http://www.menzies.edu.au/ethics/tehrec/tiwi_agreement.pdf>. Accessed 7January 2002, no longer available.
- 15. Humphreys J, Lyle D, Wakerman J, et al. Roles and activities of the Commonwealth Government university departments of rural health. Aust J Rural Health 2000; 8: 120-133.
- 16. Lawson KA, Chew M, van der Weyden MB. A revolution in rural and remote Australia: bringing health education to the bush. Med J Aust 2000; 173: 618-624. <eMJA full text>
- 17. Best J. Rural health stocktake advisory paper to the Commonwealth Department of Health and Aged Care. Melbourne: Diagnosis Pty Ltd, 2000; 118.
- 18. Rumbalara Football Netball Club and Department of Rural Health, University of Melbourne. Evaluation of the healthy lifestyles program. Shepparton, Vic: Rumbalara Football Netball Club and Department of Rural Health, University of Melbourne, 2001.
- 19. Rumbalara Aboriginal Co-operative and Department of Psychiatry, University of Melbourne. Report of the Rumbalara Aboriginal mental health research project. Shepparton (Vic): Rumbalara Aboriginal Co-operative, 2001.
- 20. Bonita R, Beaglehole R. Cardiovascular disease epidemiology in developing countries: ethics and etiquette. Lancet 1994; 344: 1586-1587.
- 21. University of Melbourne Human Ethics Committee. Application for approval of a project involving human participants. Melbourne: Melbourne Research and Innovation Office, 2000.
- 22. University of Sydney, Human Research Ethics Committee. Ethics application for research involving humans. Sydney: University of Sydney, Human Research Ethics Committee, 2000.
- 23. Jackson LR, Ward JE. Aboriginal health: why is reconciliation necessary? Med J Aust 1999; 170: 437-440.
- 24. Voyle JA, Simmons D. Community development through partnership: promoting health in an urban indigenous community in New Zealand. Soc Sci Med 1999; 49: 1035-1050.
- 25. McDermott R, O'Dea K, Rowley K, et al. Beneficial impact of the Homelands Movement on health outcomes in central Australian Aborigines. Aust N Z J Public Health 1998; 22: 653-658.





Abstract
The Department of Rural Health, University of Melbourne, has developed a framework for conducting research in partnership with Indigenous communities.
The framework addresses past inappropriate research practices, incorporates cultural understandings, and outlines culturally appropriate protocols.
The four parts of the framework are a committee to initiate, direct and oversee all research projects; a Koorie Team to guide research; a set of research guidelines; and a policy for the department.
The framework has been used to develop strong relations with Koorie communities and conduct various health projects.