Recently, attention has again been drawn to the high prevalence of severe vitamin D deficiency in certain population groups in Australia, including veiled and dark-skinned women and their children.2,3 Another group at high risk are the elderly: 67% of older patients admitted to a short-stay geriatric rehabilitation unit were found to have vitamin D deficiency.4 A similar prevalence has been found in residents of nursing homes.5 However, it is not widely appreciated that moderate to severe vitamin D deficiency may also occur in middle-aged people.
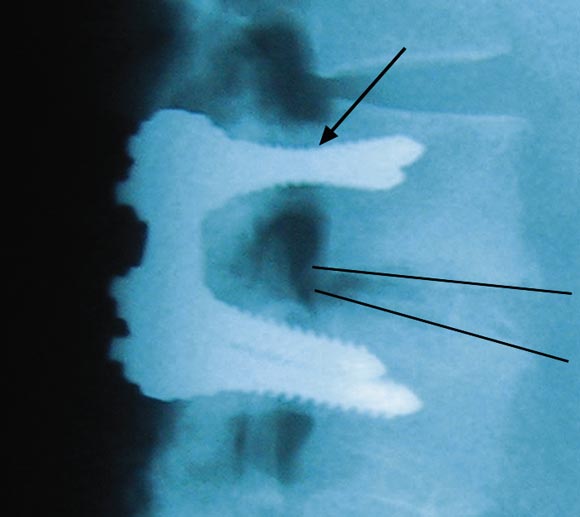
Our two patients were in their late 40s when severe vitamin D deficiency became apparent. In the first patient, recurrent pain a short time after surgery was of such severity that internal fixation plates had to be removed. The screws were loose, and, in the absence of infection, the profound vitamin D deficiency can be assumed to have resulted in failure of mineralisation of osteoid and hence failure of the surgical procedure, with resulting increased morbidity.
This patient had multiple risk factors for vitamin D deficiency (pigmented skin, habitual night-shift work and a vegetarian diet). Although he now exercises regularly, including during daylight hours, and works day-time shifts, he has required ongoing vitamin D supplementation to maintain satisfactory 25-hydroxyvitamin D (25OHD) concentrations.
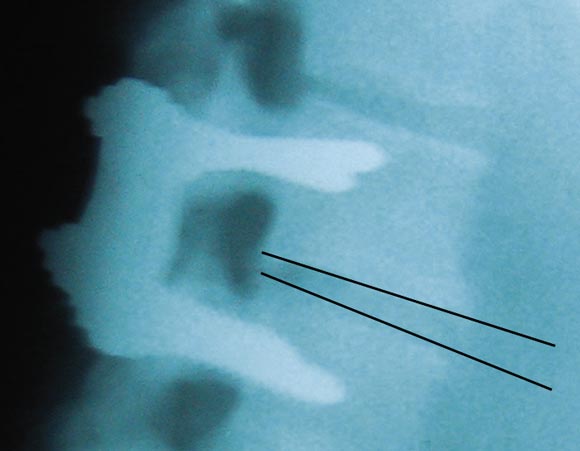
The second patient's bone had an abnormal histological appearance, and, despite an omnivorous diet, her choice to avoid direct sunlight for many years had resulted in profound vitamin D deficiency.
Vitamin D deficiency of the severity reported here is extremely uncommon in younger Australian adults. However, patients with long-standing orthopaedic or spinal disorders who become housebound may be particularly at risk, irrespective of their age.
The functions of vitamin D in bone metabolism are well known and its deficiency may be reconciled with the failure of spinal fusion, as described in these patients. This report highlights the need for attending surgeons and physicians to be aware of the potential for vitamin D deficiency in their patients, since failure to recognise this easily reversible problem may result in complications of treatment, including failure of spinal fusion surgery, additional morbidity and the substantial costs of further surgery and hospitalisation.
- Walter E Plehwe1
- Roy PL Carey2
- Epworth Medical Centre, Richmond, VIC.
- 1. Steffee AD, Biscup RS, Sitkowski DJ. Segmental spinal plates with pedicle screw fixation. A new internal fixation device for disorders of the lumbar and thoracolumbar spine. Clin Orthop 1986; 227: 45-53.
- 2. Nozza JM, Rodda CP. Vitamin D deficiency in mothers of infants with rickets. Med J Aust 2001; 175: 253-255. <eMJA full text>
- 3. Grover SR, Morley R. Vitamin D deficiency in veiled or dark-skinned pregnant women. Med J Aust 2001; 175: 251-252. <eMJA full text>
- 4. Inderjeeth CA, Nicklason F, Al-Lahham Y, et al. Vitamin D deficiency and secondary hyperparathyroidism: clinical and biochemical associations in older non-institutionalised southern Tasmanians. Aust N Z J Med 2000; 30: 209-214.
- 5. Stein MS, Scherer SC, Walton SL, et al. Risk factors for secondary hyperparathyroidism in a nursing home population. Clin Endocrinol (Oxf) 1996; 44: 375-383.