Reperfusion treatment for patients with ST-elevation myocardial infarction (STEMI) is time-critical.1 While percutaneous coronary intervention (PCI) is the preferred treatment, excessive delays have a serious adverse impact on patient outcomes. The main indicator of delay is the door-to-balloon time (DTB), and recently updated Australian guidelines have reduced the target DTB from a maximum of 90 minutes to less than 60 minutes.2,3
The state government-funded Victorian Cardiac Outcomes Registry (VCOR) was established in 2012 as a clinical quality registry for monitoring the safety and quality of treatment provided to patients with cardiovascular disease. VCOR has grown to encompass all 30 public and private PCI hospitals in Victoria.4,5 In light of the recently reduced DTB target, we undertook an in depth analysis of delays to PCI for patients with a STEMI to assist health services improve their compliance with the new guidelines. The project was approved by the Alfred Hospital (reference, 47/12) and Monash University Human Research Ethics Committees (reference, 1861).
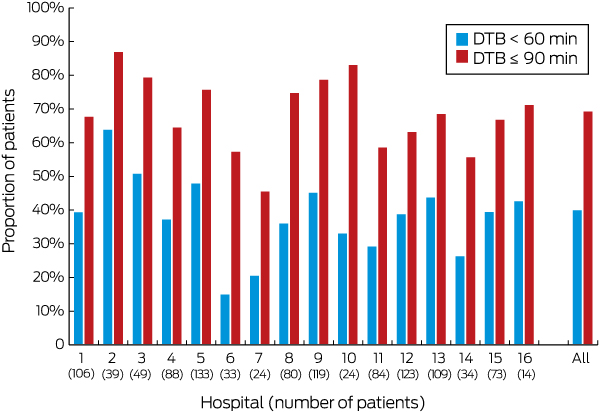
From July 2014 to June 2015, 16 of 23 participating hospitals performed PCI in 1133 patients with STEMI. Median DTB was 69 min (interquartile range [IQR], 46–100 min), compliant with the older guideline, but not with the more stringent new guideline. Five hospitals treated more than 75% of patients within 90 minutes (mean hospital compliance rate, 69.5%; range, 46–87%); none treated more than 75% of patients in under 60 minutes. There were no overall differences in DTB compliance rates between public and private hospitals (Box).
In total, 14% of patients (hospital range, 7–29%) presented during the “golden” first hour after symptom onset, when there is the greatest potential for myocardial salvage. These patients should be treated with minimal delay, but we found that the median DTB for this group was similar to that for all patients (70.5 min; IQR, 53.3–104 min) and that only 36% were treated in less than 60 minutes.
Hospital DTB compliance was greatest when ambulance officers provided pre-hospital notification of the STEMI event to hospitals; for patients with pre-notification, four sites achieved near 100% rates of DBTs of no more than 90 minutes. However, pre-hospital notification rates varied considerably between hospitals (range, 14–63%). Compliance rates were also influenced by time of presentation (in hours, 77% v after hours, 64% within 90 minutes; P < 0.001) because of increases in time taken after hours to transfer patients from hospital entry to the catheterisation laboratory. However, the median times from catheterisation laboratory arrival to reperfusion were identical (in hours, 23 min, IQR, 16–31 min; after hours, 23 min, IQR, 16–32 min).
Our analysis indicates that Victorian hospitals struggle to comply with target DTBs for timely PCI of patients with STEMI, especially with the more stringent new Australian guidelines. Reducing delays after hours and increasing rates of pre-hospital notification of receiving hospitals reduce DTB. However, more effort is needed to improve time to reperfusion for patients with STEMI treated with PCI. It is critical that health services are aware of their own performance, and registries can play an important role, assisting hospitals with their own performance assessment and continuous improvement activities.
Received 1 December 2017, accepted 8 May 2018
- 1. Yudi MB, Ramchand J, Farouque O, et al. Impact of door-to-balloon time on long-term mortality in high-and low-risk patients with ST-elevation myocardial infarction. Int J Cardiol 2016; 224: 72-78.
- 2. Aroney CN, Aylward P, Kelly AM, et al. Guidelines for the management of acute coronary syndromes 2006. Med J Aust 2006; (8 Suppl): S1-S32. <MJA full text>
- 3. Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med J Aust 2016; 205: 128-133. <MJA full text>
- 4. Asrar ul Haq M, Tsay IM, Dinh DT, et al. Prevalence and outcomes of trans-radial access for percutaneous coronary intervention in contemporary practise. Int J Cardiol 2016; 221: 264-268.
- 5. Stub D, Lefkovits J, Brennan AL, et al. The establishment of the Victorian Cardiac Outcomes Registry (VCOR): monitoring and optimizing outcomes for cardiac patients in Victoria. Heart Lung Circ 2018; 27: 451-463.





We gratefully acknowledge contributions by the VCOR Steering Committee, the VCOR Clinical Quality Committee, and the VCOR Data Research and Publications Committee. We also acknowledge the other VCOR Data and Project Management Committee staff at the Department of Epidemiology and Preventive Medicine, Monash University (Nick Andrianopoulos, Rita Brien, Harriet Carruthers, Jill Edmonds, Janine Doyle). VCOR would not be possible without the efforts of doctors, nurses, data managers, and other hospital staff who contribute data. Lead clinical staff from hospitals participating in the VCOR are also gratefully acknowledged.
No relevant disclosures.