Internationally, Australia is a leader in tobacco control policies that reduce community exposure to tobacco-related harm. In December 2012, Australia became the first country in the world to enact legislation mandating plain packaging for all tobacco products.1 The Tobacco Plain Packaging Act 2011 (Cwlth) is designed to prevent tobacco industry promotion by simultaneously reducing pack attractiveness and increasing the size of graphic health warnings. The legislation required manufacturers to produce plain packs with new warnings from 1 October 2012. From 1 December 2012, plain packaging became compulsory for all tobacco products. The new plain packs are olive green and devoid of brand design. Telephone numbers for the national smoking cessation helpline, Quitline, feature prominently on the packs.
Plain packaging legislation exists to encourage smokers to quit and discourage the uptake of smoking.1 Quitline is a free resource that can be used by smokers who are motivated and seeking support to quit. Therefore, the volume of calls to cessation helplines has frequently been used as one indicator of changes in interest in quitting in response to population-wide cessation policies and programs.2-6
In this study, we sought to examine behavioural change resulting from the introduction of the Tobacco Plain Packaging Act, complementing a recent report of smokers’ feedback.7 We did this by investigating the impact of the introduction of tobacco plain packaging on Quitline calls. To provide context, we compared the impact on Quitline calls of the introduction of tobacco plain packaging with the nationwide introduction of graphic health warnings on cigarette packaging in 2006.8 The null hypothesis was that there would be no change in call numbers, adjusting for known confounders.
This study did not require institutional ethics approval as it did not involve data about individuals. The study received no external funding. Reporting of the study complies with the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) consensus guidelines for reporting observational studies.9
An increase in anti-smoking advertising in mass media such as television is a potential confounder as it increases the number of calls to the Quitline.2,3,6 We ascertained weekly target audience rating points (TARPs) for advertisements broadcast in NSW and the ACT during the periods of interest, using OzTAM (Australian television audience measurements) for adults aged 18 years and older for free-to-air and cable television using established methods (unpublished report prepared by OzTAM for the Cancer Institute NSW). TARPs are a product of the percentage of the target audience exposed to an advertisement (reach) and the average number of times a target audience member would be exposed (frequency), adjusted for the length of the advertisement. For example, 200 TARPs might represent 100% of the target audience receiving the message twice on average over a specified period, or 50% reached four times.
Another potential confounder is cigarette costliness. We followed Wakefield et al10 and calculated cigarette costliness as the ratio of the average quarterly recommended retail price for a pack of the two top-selling Australian cigarette brands (obtained from the retail trade magazine Australian Retail Tobacconist, volumes 65 to 87) to the average weekly earnings in the same quarter obtained from the Australian Bureau of Statistics.11
Finally, the number of smokers in the community can be a potential confounder. We obtained data on smoking prevalence during the study periods from Health Statistics New South Wales,12 and this was applied to quarterly figures for population size from the Australian Bureau of Statistics13 to calculate the number of smokers in the community. Data for the first quarter of 2012 were not available, so we used results carried forward from the final quarter of 2011.
As the data for weekly number of calls to the Quitline were autocorrelated (each value was correlated with the previous value) we used autoregressive integrated moving average (ARIMA) analysis in SAS version 9.3 (SAS Institute Inc). ARIMA models enable the investigation of changes over time while accounting for seasonal variation and background trends in such things as the effects of television anti-tobacco advertising, changes in cigarette pricing relative to weekly earnings and number of smokers in the community. In ARIMA modelling, comprising model investigation, estimation and diagnostic checking, we followed the methods of Box et al (Appendix).14
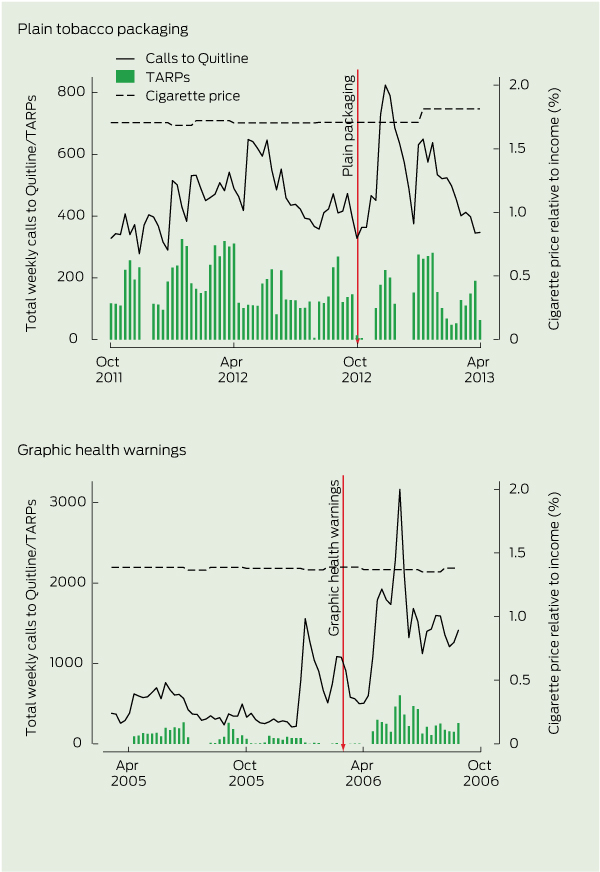
Overall, there was a general decrease in the number of calls each week to the Quitline over the period of observation. There were 910 calls in the week before the introduction of graphic health warnings in 2005 compared with 363 calls in the week before the introduction of plain tobacco packaging in 2012 (Box 1, Box 2).
Based on the estimated regression parameters from the ARIMA models (Box 3), the plain packaging intervention resulted in an increase of 288 calls (95% CI, 160–517 calls) to the NSW Quitline, representing a 78% increase from the number of calls in the week the plain packaging legislation was introduced (Box 1). This effect was sustained in subsequent weeks, with an estimated 86% of extra calls retained relative to the previous week (Box 1). As a comparison, the introduction of graphic health warnings increased the number of calls by 763 (95% CI, 473–1053), an estimated increase of 84% relative to the number of calls in the week graphic health warnings legislation was implemented (Box 1). The effect of graphic health warnings diminished more quickly, with each post-peak week retaining only 40% of the previous week’s extra calls (Box 1).
These changes need to be interpreted in the context of the earlier introduction of graphic health warnings and a raft of other legislated tobacco control policies, and secular trends in smoking rates. It is possible that the magnitude and duration of effect could be different in countries that are implementing aspects of the Framework Convention on Tobacco Control in different ways or different orders.15 For example, in NSW, the most recently legislated changes include the widespread introduction of smoke-free public spaces from 2007,16,17 and banning the display of tobacco products at the point of sale in 2010.18,19 Furthermore, smoking prevalence has declined markedly from 17.7% of NSW residents reporting daily or occasional smoking in 2006 to 14.7% in 2011.12
anti-tobacco advertising activity;
the costliness of tobacco;
the number of smokers in the community; and
seasonal peaks that are observed in the New Year period.
Although the volume of calls to the Quitline is an indirect measure of quitting intentions and behaviour, it does provide an objective outcome measure that is not subject to selection or social desirability biases that may occur in community surveys. Quitline data are available almost in real time so that the immediate impact of community-wide programs or policies can be evaluated soon after implementation. Interrupted time-series analysis provides one of the most robust methods of evaluating the impact of programs and policies that affect the whole population.20 We examined legislation enacted nationally simultaneously, precluding the use of a control group.
smoking uptake in non-smokers;
prevention of relapse among ex-smokers; and
cessation of smoking among current smokers.
This would include the need to investigate variations in impact on subgroups of the population. A comprehensive evaluation of the policy will require ongoing monitoring to assess factors such as changes in brand recognition, awareness of the health risks of smoking, the social acceptability of smoking as well as smoking prevalence.21
1 Autoregressive integrated moving average (ARIMA) modelling results for the plain packaging and graphic health warning interventions
Peak call volume attributable to intervention (calls/week) |
|||||||||||||||
2 Weekly calls to Quitline, target audience rating points (TARPs) and cigarette price relative to income, before and after the introduction of plain tobacco packaging and graphic health warnings
3 Change in numbers of call to Quitline after the introduction of plain packaging and graphic health warnings, adjusted for anti-tobacco advertising, seasonal trend, smoking prevalence and tobacco costliness*
Cigarette costliness (per 1% increase relative to average earnings) |
|||||||||||||||
* Full model details can be supplied by the authors on request. |
|||||||||||||||
Received 16 August 2013, accepted 22 October 2013
- Jane M Young1
- Ingrid Stacey2
- Timothy A Dobbins1
- Sally Dunlop2
- Anita L Dessaix2
- David C Currow2
- 1 Cancer Epidemiology and Services Research (CESR), Sydney School of Public Health, University of Sydney, Sydney, NSW.
- 2 Cancer Institute NSW, Sydney, NSW.
We thank Donna Perez and James Kite for help with obtaining the data. This study was internally funded by the Cancer Institute NSW. Thanks also to Bruce Armstrong, Sanchia Aranda, and Rebecca Kenyon for their helpful comments on the manuscript.
No relevant disclosures.
- 1. Australian Commonwealth Government. Tobacco Plain Packaging Act 2011 (Cwlth) (No. 148, 2011). http://www.comlaw.gov.au/Details/C2011A00148 (accessed Oct 2013).
- 2. Pierce JP, Anderson DM, Romano RM, et al. Promoting smoking cessation in the United States: effect of public service announcements on the Cancer Information Service telephone line. J Natl Cancer Inst 1992; 84: 677-683.
- 3. Siahpush M, Wakefield M, Spittal M, Durkin S. Antismoking television advertising and socioeconomic variations in calls to Quitline. J Epidemiol Community Health 2007; 61: 298-301.
- 4. Chan SS, Wong DC, Fong DY, et al. Short-term impact of new smoke-free legislation on the utilization of a quitline in Hong Kong. Nicotine Tob Res 2009; 11: 356-361.
- 5. Miller CL, Wakefield M, Roberts L. Uptake and effectiveness of the Australian telephone Quitline service in the context of a mass media campaign. Tob Control 2003; 12 Suppl 2: ii53-ii58.
- 6. Farrelly MC, Davis KC, Nonnemaker JM, et al. Promoting calls to a quitline: quantifying the influence of message theme, strong negative emotions and graphic images in television advertisements. Tob Control 2011; 20: 279-284.
- 7. Wakefield MA, Hayes L, Durkin S, Borland R. Introduction effects of the Australian plain packaging policy on adult smokers: a cross-sectional study. BMJ Open 2013; 3: e003175.
- 8. Australian Commonwealth Government. Trade Practices (Consumer Product Information Standards) (Tobacco) Regulations 2004. http://www.comlaw.gov.au/Details/F2007C00131 (accessed Oct 2013).
- 9. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806-808.
- 10. Wakefield MA, Durkin S, Spittal MJ, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health 2008; 98: 1443-1450.
- 11. Australian Bureau of Statistics. Average weekly earnings, Australia, Nov 2012. (ABS Cat. No. 6302.0.) http://abs.gov.au/ausstats/abs@.nsf/mf/6302.0 (accessed Oct 2013).
- 12. Centre for Epidemiology and Evidence. Health statistics New South Wales. Sydney: NSW Ministry of Health. http://www.healthstats.nsw. gov.au (accessed Oct 2013).
- 13. Australian Bureau of Statistics. Australian Demographic Statistics, Dec 2012. (ABS Cat. No. 3101.0.) http://www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 (accessed Oct 2013).
- 14. Box GEP, Jenkins GM, Reinsel GC. Time series analysis: forecasting and control. 4th ed. Hoboken, NJ: John Wiley & Sons, 2008.
- 15. World Health Organization. WHO Framework Convention on Tobacco Control. Geneva: WHO, 2003. http://whqlibdoc.who.int/publications/2003/9241591013.pdf (accessed Oct 2013).
- 16. New South Wales Government. Tobacco Legislation Amendment Act 2012 (NSW) No 56. http://www.legislation.nsw.gov.au/sessionalview/sessional/act/2012-56.pdf (accessed Oct 2013).
- 17. Australian Capital Territory Government. Smoke-Free Public Places Act 2003 (ACT). http://www.l egislation.act.gov.au/a/2003-51/current/pdf/2003-51.pdf (accessed Oct 2013).
- 18. New South Wales Government. Tobacco retailing laws. Public Health (Tobacco) Act 2008 (NSW). http://www0.health.nsw.gov.au/publichealth/healthpromotion/tobacco/information_for_tobacco_retailers_and_consumers.asp (accessed Oct 2013).
- 19. Australian Capital Territory Government. Tobacco Amendment Act 2008. (repealed) http://www. legislation.act.gov.au/a/2008-50/default.asp (accessed Oct 2013).
- 20. Lagarde M. How to do (or not to do) . . . assessing the impact of a policy change with routine longitudinal data. Health Policy Plan 2012; 27: 76-83.
- 21. Hammond D, Wakefield M, Durkin S, Brennan E. Tobacco packaging and mass media campaigns: research needs for Articles 11 and 12 of the WHO Framework Convention on Tobacco Control. Nicotine Tob Res 2013; 15: 817-831.





Abstract
Objectives: To investigate whether the introduction of tobacco plain packaging in Australia from 1 October 2012 was associated with a change in the number of calls to the smoking cessation helpline, Quitline, and to compare this with the impact of the introduction of graphic health warnings from 1 March 2006.
Design and setting: Whole-of-population interrupted time-series analysis in New South Wales and the Australian Capital Territory between 1 March 2005 and October 2006 for the comparator, graphic health warnings, and October 2011 and April 2013 for the intervention of interest, tobacco plain packaging.
Main outcome measure: Weekly number of calls to the Quitline, after adjusting for seasonal trends, anti-tobacco advertising, cigarette costliness and the number of smokers in the community.
Results: There was a 78% increase in the number of calls to the Quitline associated with the introduction of plain packaging (baseline, 363/week; peak, 651/week [95% CI, 523–780/week; P < 0.001]). This peak occurred 4 weeks after the initial appearance of plain packaging and has been prolonged. The 2006 introduction of graphic health warnings had the same relative increase in calls (84%; baseline, 910/week; peak, 1673/week [95% CI, 1383–1963/week; P < 0.001]) but the impact of plain packaging has continued for longer.
Conclusions: There has been a sustained increase in calls to the Quitline after the introduction of tobacco plain packaging. This increase is not attributable to anti-tobacco advertising activity, cigarette price increases nor other identifiable causes. This is an important incremental step in comprehensive tobacco control.