Practice nursing is one of the few growth areas in the Australian general practice workforce. Between 2003 and 2007, the number of practice nurses nearly doubled, to 7824.1,2 By contrast, in the 5 years to 2005, the Australian nursing workforce increased overall by only 6.6%.3,4 The growth of general practice nursing has been facilitated by a number of Medicare-rebatable items for nurses, incentives in rural areas to hire nurses, support from the Divisions of General Practice,5 and the federal government’s Nursing in General Practice program. Employing practice nurses has been touted as a way of solving health workforce shortages6 and improving quality of health care.7,8 Despite the largely positive rhetoric about practice nurses in the medical and mainstream media,9,10 there has been little detailed research on their roles or the ways in which they may be changing the general practice workplace.11
Australian general practices are small-scale, geographically dispersed businesses with considerable structural diversity. Australian studies on practice nursing have for the most part been small studies using interviews (which may have poor generalisability)12,13 or larger surveys of reported activities by nurses (which may overlook contextual issues).14,15 Our study aimed to describe the evolving roles of practice nurses in Australia and the impact of nurses on general practice function.
A cross-sectional study exploring the scope and contextual determinants of nurse roles (Substudy 1); and
A 12-month longitudinal study exploring change in nurse roles and their impact on general practices as organisations (Substudy 2).
For Substudy 1, multiple data were collected during day-long visits (one per practice) to 25 practices in New South Wales and Victoria between September 2005 and March 2006 (Box 1). The diverse datasets gathered (using interviews, observations, photographs, field notes and practice maps) were designed to illuminate the relationships between nurse roles and the practice’s physical and managerial structure, as well as the perspectives of nurses, managers and general practitioners on nurse roles (Box 2).
For Substudy 2, action research (a process of collective problem-solving)17 was used to engage nurses, GPs and practice managers in identifying and introducing a change to the role of the practice nurse. The sampling frame included seven practices nominated by their Divisions of General Practice as “cutting edge” or “mainstream” general practices (one urban, three regional and three rural practices located in Victoria, NSW, Western Australia, South Australia and Queensland). The impact on the practice was followed with collection of baseline, process and outcome data over a 1-year period (between January 2007 and March 2008) and interviews with practice and Division staff (Box 2). Practices received minimal external support from the research team.
In both substudies, intra-case and inter-case analyses were performed for each practice by a multidisciplinary team (sociologist, nurse, GP, policy analyst). The team probed for emergent themes, using the constant comparison method,18 and cross-checked with practices. Emergent themes included structural elements (health care policy, environment, gender, nursing culture); practice-level elements (interprofessional relationships, time-use patterns, spatial structures); and individual factors. All data, including photographs and floorplans, were coded into a database using NVivo qualitative data analysis software, version 7 (QSR International, Melbourne, Vic), enabling triangulated data interpretation.
[B]ecause I do health assessments I know a lot of them and they do ring me too for problems they have. I’m expecting someone to come over — I’ve just organised a new blood sugar monitor for her. She’s a diabetic and she rang me and said she wanted to know how to use it. So I’m going to go through that with her . . . she doesn’t have to see the doctor, it’s just a service, just an extra thing to fit into the day. [Practice nurse 2, Practice 5]
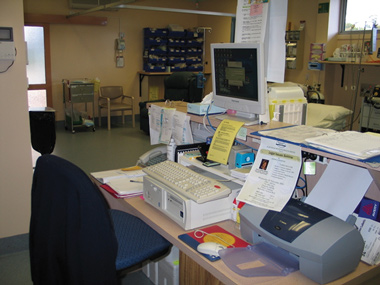
Nurses undertook the organisational aspects of patient care (recall systems, reminders, feedback of patient results, follow-up of specialist appointments) and systems supporting patient care (stocking drugs, cleaning and sterilising instruments, managing contaminated waste). A range of nurses’ desks, demonstrating the way they configure their workstations as places that communicate organisational and clinical activity, is shown in Box. The organisational features, such as crowded pin-up boards, “post-it” notes and flyers, are typical of nurses’ rather than doctors’ desks.
I was involved in the first accreditation process and I really needed her expertise. Nurses, they understand a lot of — because of their hospital background — a lot of this bureaucracy-speak which is foreign to general practice. [GP, Practice 16]
Nursing work is generally very busy, with nurses rapidly cycling between many roles or undertaking them concurrently. An example of cycling between five roles in one rural general practice is presented in Box 4. While undertaking several clinical tasks, the nurse also left the room to locate lost files, oversee the transfer of pathology specimens to the courier, and have a conversation with a patient in the waiting room. She then educated her nursing colleague about oral rehydration. The layout of the practice, with a central treatment room affording ready access from the GP consultation rooms and reception desk, reinforced her connectivity role.
The nurse roles addressed in Substudy 2 are listed in Box 5. The patient carer role was addressed most frequently, reflecting its primacy in the eyes of all clinicians in general practice. Enhancing the nurse role in one area often had the complementary effect of advancing other roles (Box 6). Open communication between GPs, managers and nurses was an important determinant of successful enhancement of nurse roles. In Practice 29, which failed to enhance the patient carer role through one project, the collaborative planning process resulted in identification of another project to (successfully) enhance this role. The inability of Practice 27 to introduce a change in the educator role was because of the lack of priority given to education and connectivity by doctors in a practice that lacked systems for formal interdisciplinary communication.
Our study showed that practice nurses perform at least six roles, often alternating rapidly between them. The six roles elaborate on, and are consonant with, the four domains of practice articulated in a 2004 Australian report on practice nurse roles: administration, clinical care, integration and practice management.14 The connectivity role represents a fundamental nursing strength that has also been described in Australian hospital studies.19 The function of nurses as agents of connectivity has been implicitly taken up in the interim report of the National Health and Hospitals Reform Commission20 in its calls for nurses to be in schools, provide aged-care outreach, support disabled patients, and foster connections between hospital and community. Complexity theory suggests that interconnecting, complex relationships and linkages within an organisation help it to be resilient and adaptive.21-23 Our study suggested that the connectivity role of nurses may help drive organisational resilience in general practice.
Although GPs recognised the nurse roles of patient carer, organiser and quality controller, they were less aware of the problem-solver, educator and connectivity roles. Representations from GPs on the potential scope of practice of nurses may, therefore, underplay some key nursing contributions to general practice. At present, these roles are supported by the more flexible working patterns of nurses. In adjusting the funding structure for nurses, care should be taken not to create perverse incentives to limit nurses’ clinical capacity or undermine the flexibility that gives practice nursing much of its savour for nurses and value for practices.24,25
1 Characteristics of participating practices, Substudy 1
Private + experimental collaborative model with state partners |
|||||||||||||||
2 Description of datasets for each substudy
A range of nursing stations in general practice, illustrating the organiser role of nurses
5 Changes introduced to nurse roles, Substudy 2
Nurse-led collaboration for better mental health care communication |
|||||||||||||||
- Christine B Phillips1
- Christopher Pearce2,3
- Sally Hall1
- Marjan Kljakovic1
- Bonnie Sibbald4
- Kathryn Dwan1
- Julie Porritt5
- Rachel Yates5
- 1 Academic Unit of General Practice and Community Health, Australian National University, Canberra, ACT.
- 2 Melbourne East General Practice Network, Melbourne, VIC.
- 3 University of Melbourne, Melbourne, VIC.
- 4 National Primary Care Research and Development Centre, University of Manchester, Manchester, UK.
- 5 Australian General Practice Network, Canberra, ACT.
Our research was funded by a grant from the Australian Government Department of Health and Ageing through the Australian Primary Health Care Research Institute (APHCRI). We are grateful to the staff of all participating general practices, the Divisions of General Practice who supported the research, and to Monika Thompson, Hannah Walker, Daniel Sybaczynskyj and Miriam Glennie for their research assistance. The opinions expressed in this article are not the opinions of APHCRI or the Department of Health and Ageing.
None identified.
- 1. Australian Divisions of General Practice. National practice nurse workforce survey report 2003. Canberra: ADGP, 2004.
- 2. Australian General Practice Network. National practice nurse workforce survey report 2007. Canberra: AGPN, 2008.
- 3. Australian Institute of Health and Welfare. Nursing and midwifery labour force 2005. Canberra: AIHW, 2008. (AIHW Cat. No. HWL 40; National Health Labour Force Series No. 39.)
- 4. Australian Institute of Health and Welfare. Nursing labour force 2002. Canberra: AIHW, 2003. (AIHW Cat. No. HWL 29; National Health Labour Force Series No. 29.)
- 5. Hall S. Divisions of general practice and practice nurse development in Australia. Contemp Nurse 2007; 26: 37-47.
- 6. Walker L. Practice nurses — working smarter in general practice. Aust Fam Physician 2006; 35: 20-22.
- 7. Taylor SJ, Candy B, Bryar RM, et al. Effectiveness of innovations in nurse led chronic disease management for patients with chronic obstructive pulmonary disease: systematic review of evidence. BMJ 2005; 331: 485-488.
- 8. Renders CM, Valk GD, Griffin S, et al. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev 2001; (1): CD001481.
- 9. Wiseman H. Sharing the load. Aust Doct 2007; 6 Nov: 19-22. http://www.australiandoctor. com.au/news/e3/0c0519e3.asp (accessed Jun 2009).
- 10. Cresswell A. Nurses seek expanded role. The Australian 2009; 7 Feb. http://www.theaustralian.news.com.au/story/0,,25013316-23289,00.html (accessed Apr 2009, link updated July 2009).
- 11. Halcomb EJ, Davidson PM, Daly JP, et al. Nursing in Australian general practice: directions and perspectives. Aust Health Rev 2005; 29: 156-166.
- 12. Tolhurst H, Madjar L, Schultz L, Schmidt A. Nurses in urban and rural general practice. Who are they and what do they do? Aust Fam Physician 2004; 33: 185-187, 190.
- 13. Condon J, Willis E, Litt J. The role of the practice nurse. An exploratory study. Aust Fam Physician 2000; 29: 272-277.
- 14. Watts IF, Hutchinson E, Pasoe R, et al. General practice nursing in Australia. Melbourne: Royal Australian College of General Practitioners and Royal College of Nursing, Australia, 2004.
- 15. Halcomb EJ, Davidson PM, Salamonson Y, et al. Nurses in Australian general practice: implications for chronic disease management. J Clin Nurs 2008; 17: 6-15.
- 16. McIlvain H, Crabtree B, Medder J, et al. Using practice genograms to understand and describe practice configurations. Fam Med 1998; 30: 490-496.
- 17. Greenwood DJ, Levin M. Introduction to action research: social research for social change. Thousand Oaks, Calif: Sage Publications, 1998.
- 18. Lincoln YS, Guba EG. Naturalistic inquiry. Newbury Park, Calif: Sage Publications, 1985.
- 19. Duffield C, Roche M, O’Brien-Pallas L, et al. Gluing it together: nurses, their work environment and patient safety. Final report. Sydney: Centre for Health Services Management, University of Technology, Sydney, 2007.
- 20. National Health and Hospitals Reform Commission. A healthier future for all Australians: interim report December 2008. Canberra: Commonwealth of Australia, 2009. http://www.nhhrc.org.au/internet/nhhrc/publishing.nsf/Content/interim-report-december-2008 (accessed Jun 2009).
- 21. Paley J. Complex adaptive systems and nursing. Nurs Inq 2007; 14: 233-242.
- 22. Miller WL, Crabtree BF, McDaniel R, Stange KC. Understanding change in primary care practice using complexity theory. J Fam Pract 1998; 46: 369-376.
- 23. Checkland K. Understanding general practice: a conceptual framework developed from case studies in the UK NHS. Br J Gen Pract 2007; 57: 56-63.
- 24. Pearce C, Phillips C, Hall S, et al. Contributions from the lifeworld: quality, caring and the general practice nurse. Qual Prim Care 2009; 17: 5-13.
- 25. Phillips CB, Dwan K, Pearce C, et al. Time to talk, time to see: changing microeconomies of professional practice among nurses and doctors in Australian general practice. Contemp Nurse 2007; 26: 136-144.







Abstract
Objective: To describe the evolving roles of practice nurses in Australia and the impact of nurses on general practice function.
Design, setting and participants: Multimethod research in two substudies: (a) a rapid appraisal based on observation, photographs of workspaces, and interviews with nurses, doctors and managers in 25 practices in Victoria and New South Wales, conducted between September 2005 and March 2006; and (b) naturalistic longitudinal case studies of introduced change in seven practices in Victoria, NSW, South Australia, Queensland and Western Australia, conducted between January 2007 and March 2008.
Results: We identified six roles of nurses in general practice: patient carer, organiser, quality controller, problem solver, educator and agent of connectivity. Although the first three roles are appreciated as nursing strengths by both nurses and doctors, doctors tended not to recognise nurses’ educator and problem solver roles within the practice. Only 21% of the clinical activities undertaken by nurses were directly funded through Medicare. The role of the nurse as an agent of connectivity, uniting the different workers within the practice organisation, is particularly notable in small and medium-sized practices, and may be a key determinant of organisational resilience.
Conclusion: Nurseing roles may be enhanced through progressive broadening of the scope of the patient care role, fostering the nurse educator role, and addressing barriers to role enhancement, such as organisational inexperience with interprofessional work and lack of a career structure. In adjusting the funding structure for nurses, care should be taken not to create perverse incentives to limit nurses’ clinical capacity or undermine the flexibility that gives practice nursing much of its value for nurses and practices.