First Nations Yolŋu women are speaking up to reclaim control and return of childbirth services
Over the millennia, First Nations women across Australia have given birth on their Country, supported by family and cultural caring practices, until recent disruption from European colonisation.1 Today, First Nations women, babies and families experience profound health inequities when comparing health outcomes to their Australian counterparts. A disproportionate number of First Nations women experience adverse outcomes in pregnancy and birth. For the past ten years, there has been little or no improvement in perinatal indicators. Maternal death for First Nations mothers is 3.7 times higher than for other Australian women,2 and perinatal deaths, largely driven by complications of pregnancy, are twice as high, although slightly improved between 2008 and 2018.3
Preterm birth is the largest contributor to infant and child mortality. It is associated with life course health inequities including developmental and behavioural problems, with negative impacts on schooling and educational attainment, childhood disability, and chronic diseases in adulthood.4 Preterm birth rates are 1.7 times higher for First Nations babies across Australia and are highest in remote regions, especially in the Top End of the Northern Territory, where about one in five babies are born prematurely (18–22% a year) compared with premature birth rates for all NT Aboriginal women (17%) and NT non‐Aboriginal women (7%).5 Prevention of avoidable preterm birth in First Nations families living in remote areas is an important issue requiring innovative solutions.
Government policy has seen the closure of many maternity services across regional and remote Australia, resulting in relocation of many women,6 centralised and specialised maternity management in tertiary hospitals, and inequitable service distribution across Australia.7 This disproportionality impacts First Nations families,7 with closure of services amplifying social risk factors for women and families, which exacerbates clinical risk.8 Centralisation of maternity services is also correlated with increasing rates of babies being born before arrival to hospital, unplanned in transit and with no access to midwifery and/or medical support.9
In the North East Arnhem Land region in the NT (Box 1), First Nations Yolŋu women from the island town of Galiwin’ku experience some of most extreme structural inequities in all of Australia, including overcrowding, homelessness, unemployment and poverty, resulting in profound health inequities. Led by Yolŋu scholar and Ancestral knowledge holder Associate Professor Elaine Ḻäwurrpa Maypilama, the Caring for Mum on Country project has been working with local women to begin addressing the region’s entrenched perinatal inequities. Women are speaking up to reclaim the control and return of childbirth services to their community. They aim to achieve this by establishing a national very remote exemplar demonstration Birthing on Country maternity service, providing evidence‐based Western medical maternity care (earlier in pregnancy and more frequently than currently occurs), integrated with cultural caring practices delivered by a workforce of skilled Yolŋu djäkamirr — the cultural caretakers of pregnancy and birth.10 Djäkamirr are doulas who have undergone government recognised vocational educational training alongside a Yolŋu knowledge curriculum. The community wants clinically and culturally safe care, with referral pathways to manage medical and sociocultural complications, using both knowledge systems and workforces.
Birthing on Country is an international social justice movement to redress the negative impact of colonisation and return childbirth services to First Nations communities and their control.1 Building on these aspirations, Birthing on Country maternity services are complex, evidence‐based interventions that include: a redesigned maternity service prioritising a First Nations workforce and governance; 24/7 continuity of midwifery carer; holistic support; programs that strengthen cultural identity and connection; and integrated care pathways across primary and tertiary services.11 A Queensland urban exemplar Birthing on Country service has been established and its evaluated impact found women were more likely to attend five or more antenatal visits (adjusted odds ratio [AOR], 1.54; 95% CI, 1.13–2.09; P = 0·0064), less likely to have an infant born preterm (AOR, 0.62; CI, 0.42–0.93; P = 0·019), and more likely to exclusively breastfeed on discharge from hospital (AOR, 1.34; CI, 1.06–1.70; P = 0·014).12 A key contributor to this was thought to be an over 500% increase in the First Nations workforce,13 which increased the cultural capability of the service while also targeting the social determinants of health for First Nations women through employment and training.13
Few interventions designed to prevent preterm birth in socio‐economically disadvantaged and vulnerable women in high income countries have been as effective, highlighting the importance of this research. The intervention was multifaceted and drove structural sustainable changes to care provision. The observed reduction in preterm birth is extraordinary considering there has been no change to national preterm rates for First Nations women since the Closing the Gap strategy began in 2008.3 The approach is yet to be trialled in regional or remote Australia.
In October 2020, the Caring for Mum on Country project, in partnership with the Birthing on Country Centre for Research Excellence and Yalu Aboriginal Corporation, convened a workshop in Nhulunbuy, NT. The workshop was in response to a previous Galiwin’ku community consultation in which senior Yolŋu women called for birthing services to be returned to their island, and that services should better incorporate Yolŋu cultural care. Yolŋu women from Galiwin’ku, alongside researchers from the Molly Wardaguga Research Centre at Charles Darwin University, gathered with local services to explore how a Birthing on Country service could improve Yolŋu perinatal outcomes. Over 40 participants attended the workshop, comprising Yolŋu women and leaders, local midwives, doctors, child health nurses, service managers, key leaders from NT Health, Miwatj Health Aboriginal Corporation, CareFlight and other service providers. The workshop included many First Nations participants.
The workshop established wide community and service support to urgently redesign the maternity system in North East Arnhem Land. There was no consensus on returning birthing services to Galiwin’ku. Yolŋu women alongside researchers were more supportive of this goal. The Birthing on Country RISE framework, which demonstrates four potential phases of redesign (Box 2),13 had already been established as transferable and acceptable in this setting and was endorsed as a useful tool to guide this process. Using the RISE framework,1 participants established local priorities:
- ▪ Redesigning the system: increasing coordination, communication, collaboration and continuity of carers; investigating the reasons non‐Yolŋu health staff leave; and incorporating cultural practices and support into childbirth care.
- ▪ Investing in the workforce: recruiting and supporting more midwives and doctors to provide culturally and clinical exceptional care; increasing the numbers of First Nations midwives and student midwives; rolling out the djäkamirr pilot program through the region; and streamlining community liaison and support roles that exist in multiple agencies.
- ▪ Strengthening the capacity of Yolŋu families: instigating culturally appropriate reproductive health literacy education; enabling cultural practices to be conducted across the maternity journey in all settings (tertiary and primary care); keeping families strong by physically connecting them with Patient Assistance Travel Scheme funds; providing family‐friendly spaces in the hospital; and addressing overcrowding of houses in remote communities.
- ▪ Embedding community governance, control and engagement: recruiting and supporting Yolŋu women in leadership roles; providing stakeholder access to health outcome statistics; increasing access to interpreters; and developing a regional steering committee to drive and coordinate systematic change to address the equities.
Following the Nhulunbuy workshop, in 2021 the then NT Health Minister Natasha Fyles stated that imminent restructure of the NT Health Department presented an opportunity to invest in Birthing on Country maternity services.14 In defiance of historical trends, service leaders have now begun participating in a regional steering committee and two working groups to progress Yolŋu‐led decolonising service redesign.15,16 The research team, together with collaborating partners, has received two grants to progress the service redesign. Based on recent research evidence,17 this is a once‐in‐a‐generation opportunity to dismantle some structural inequities, as we collaboratively strive for equitable outcomes for Yolŋu mothers and babies. As the Galiwin’ku community aspires to become a national very remote Birthing on Country exemplar demonstration site, there is responsibility for clinicians, government and service providers to listen, support and adequately resource the community in line with national policy guidelines. For too long Yolŋu women and families have been excluded from maternity service design and delivery in their own community — biomedical services have been imposed upon them and multiple consultations undertaken but ignored. As Yolŋu woman Associate Professor Maypilama states in the documentary describing the journey so far:10 “If you listen carefully and hear what is coming in, it will come into your heart and then you can help. We need your hand please.”
Box 1 – Map of the Top End of the Northern Territory, Australia, with the Arnhem Land region and Yolŋu Country, North East Arnhem Land shaded in green with approximate boundaries

Box 2 – The four pillars of RISE and possible implementation phases for Birthing on Country maternity services
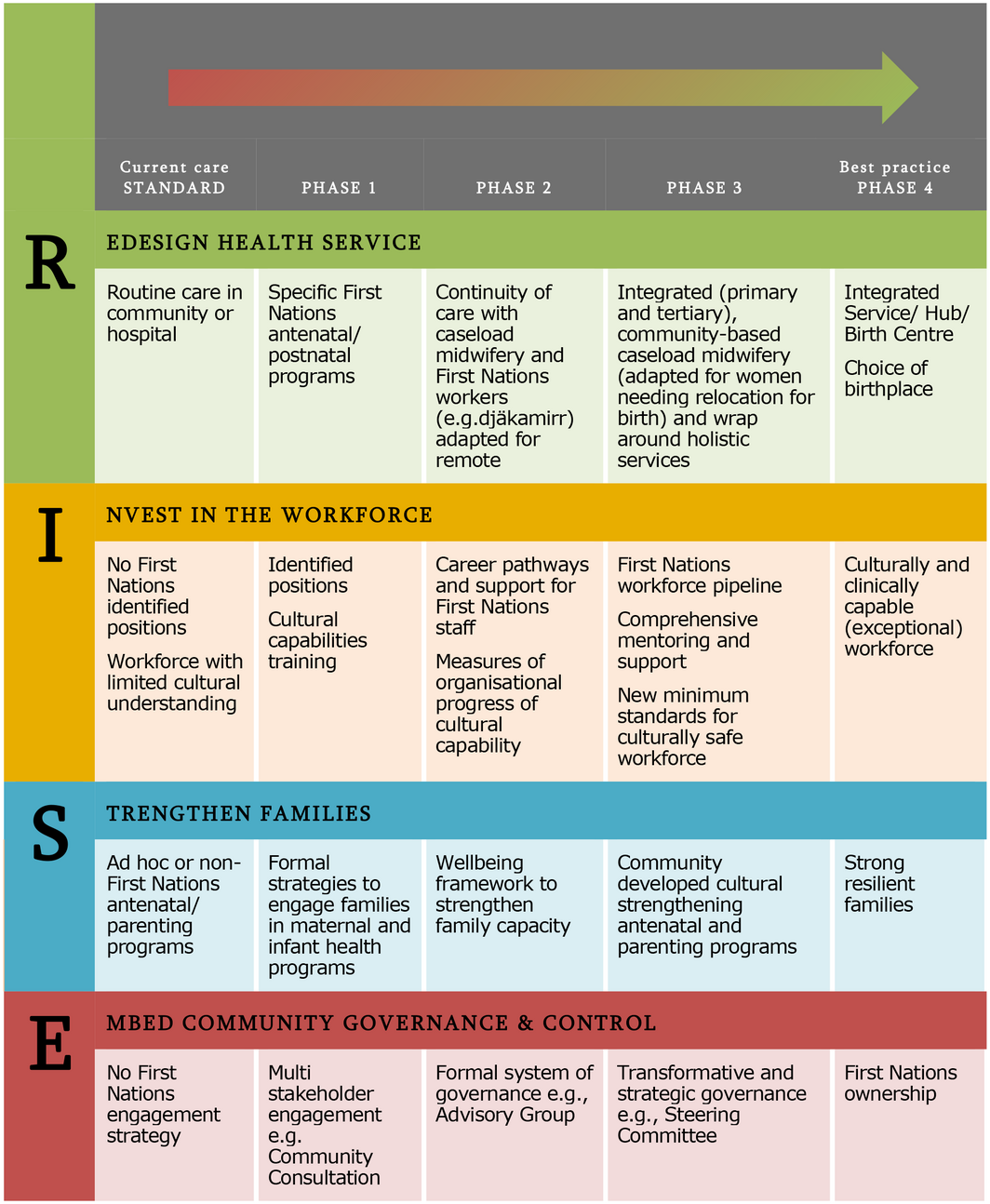
Adapted for the remote context with permission from Kildea et al.13
Provenance: Not commissioned; externally peer reviewed.
- 1. Ireland S, Maypilama EL, Roe Y, et al. Caring for Mum on Country: exploring the transferability of the Birthing on Country RISE framework in a remote multilingual Northern Australian context. Women Birth 2020; 34: 487‐492.
- 2. Australian Institute of Health and Welfare. Maternal deaths in Australia 2009–2018. Canberra: Australian Institute of Health and Welfare, 2020. https://www.aihw.gov.au/reports/mothers‐babies/maternal‐deaths‐in‐australia/contents/maternal‐deaths‐in‐australia (viewed Dec 2021).
- 3. Commonwealth of Australia. Closing the Gap report 2020. Canberra: Australian Government, 2020. https://ctgreport.niaa.gov.au/ (viewed Dec 2021).
- 4. Msall ME, Sobotka SA, Dmowska A, et al. Life course health development outcomes after prematurity: developing a community, clinical, and translational research agenda to optimize health, behaviour, and functioning. In: Halfon N, Forrest CB, Lerner RM, Faustman EM, editors. Handbook of life course health development. Cham: Springer International Publishing, 2018: pp. 321‐348. https://doi.org/10.1007/978‐3‐319‐47143‐3_14 (viewed Oct 2020).
- 5. Li L, O’Neil L. Mothers and babies 2017: Northern Territory Midwives’ Collection. Darwin: Department of Health, 2020. https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/11647/1/Mothers%20and%20Babies%20Report_2017.pdf (viewed Dec 2021).
- 6. Longman J, Kornelsen J, Pilcher J, et al. Maternity services for rural and remote Australia: barriers to operationalising national policy. Health Policy 2017; 121: 1161‐1168.
- 7. Rolfe MI, Donoghue DA, Longman JM, et al. The distribution of maternity services across rural and remote Australia: does it reflect population need? BMC Health Serv Res 2017; 17: 163.
- 8. Barclay L, Kornelsen J, Longman J, et al. Reconceptualising risk: Perceptions of risk in rural and remote maternity service planning. Midwifery 2016; 38: 63‐70.
- 9. Kildea S, McGhie AC, Gao Y, et al. Babies born before arrival to hospital and maternity unit closures in Queensland and Australia. Women Birth 2015; 28: 236‐245.
- 10. Maypilama L, Josse P, Ireland S. Djäkamirr: caretaker of pregnancy and birth [documentary film]. ONE20 Productions, 2021. https://www.birthingoncountry.com/djakamirr (viewed Dec 2021).
- 11. Kildea S, Lockey R, Roberts J, et al. Guiding principles for developing a Birthing on Country service model and evaluation framework, phase 1. Brisbane: Mater Medical Research Unit and the University of Queensland on behalf of the Maternity Services Inter‐Jurisdictional Committee for the Australian Health Ministers’ Advisory Council, 2016. https://www.researchgate.net/publication/309584016_Guiding_Principles_for_Developing_a_Birthing_on_Country_Service_Model_and_Evaluation_Framework_Phase_1 (viewed July 2021).
- 12. Kildea S, Gao Y, Hickey S, et al. Effect of a Birthing on Country service redesign on maternal and neonatal health outcomes for First Nations Australians: a prospective, non‐randomised, interventional trial. Lancet Glob Health 2021; 9: e651‐e659.
- 13. Kildea S, Hickey S, Barclay L, et al. Implementing Birthing on Country services for Aboriginal and Torres Strait Islander families: RISE framework. Women Birth 2019; 32: 466‐475.
- 14. Roberts L. NT Health Minister Natasha Fyles on returning birthing to remote and regional locations. ABC News 2021; 3 June. https://www.abc.net.au/news/health/2021‐06‐03/health‐nt‐health‐minister‐commits‐to‐birthing‐on‐country/100180990 (viewed May 2022).
- 15. Molly Wardaguga Research Centre. To be born upon a pandanus mat. https://www.birthingoncountry.com/to‐be‐born‐upon‐a‐pandanus‐mat (viewed May 2022).
- 16. Charles Darwin University. Molly Wardaguga Research Centre secures $5 million to support First Nations maternal health. 6 Apr 2022. https://www.cdu.edu.au/news/molly‐wardaguga‐research‐centre‐secures‐5‐million‐support‐first‐nations‐maternal‐health (viewed May 2022).
- 17. Kildea S, Gao Y, Hickey S, et al. Reducing preterm birth amongst Aboriginal and Torres Strait Islander babies: a prospective cohort study, Brisbane, Australia. EClinicalMedicine 2019; 12: 43‐51.






Open access
Open access publishing facilitated by Charles Darwin University, as part of the Wiley ‐ Charles Darwin University agreement via the Council of Australian University Librarians.
Our work was supported by the Birthing on Country Centre for Research Excellence at the Molly Wardaguga Research Centre, Charles Darwin University (APP 1197110), a Lowitja Institute Seeding Grant (20‐SG‐12), and Yalu Aboriginal Corporation. Funding contributed to researcher salaries and costs associated with traveling to and hosting the regional workshop. We acknowledge Raisa Brozalevskaia from Charles Darwin University and Alice McCarthy from Yalu Aboriginal Corporation for their dedication and support of Yolŋu researchers.
No relevant disclosures.