The coronavirus disease 2019 (COVID‐19) pandemic reduced routine vaccination activity in many countries.1,2,3 Strict physical distancing and movement restrictions (stage 3 lockdown measures) were implemented in Australia from 23 March 2020, with many health care providers moving to telehealth‐based models of care. Earlier analyses found the first pandemic wave did not affect childhood vaccination activity at the national or state/territory levels to July 2020.4 But vaccination activity has not been assessed during the more stringent stage 4 lockdowns during the second epidemic wave in Victoria (early August ‒ late October 2020). Further, the effects of the shift to remote learning on the vaccination of adolescents, usually delivered in schools, have not been assessed, nor the impact of the epidemic on vaccinations for older adults. We therefore compared vaccination activity in Victoria in 2019 and 2020 by analysing de‐identified Australian Immunisation Register (AIR) surveillance data (status: 28 February 2021). The Sydney Children’s Hospitals Network Human Research Ethics Committee exempted our analysis of AIR data, approved by the Australian Department of Health, from formal ethics approval.
We assessed the administration of selected vaccines scheduled for 2, 4, and 12 months of age, by one‐month birth cohorts and the Indigenous status of recipients. We assessed uptake within one month of the scheduled vaccination date; that is, earlier than for standard vaccination coverage reporting (6‒12 months after scheduled dates).5 The proportion of children vaccinated was based on the total number of eligible children registered in the AIR. Human papillomavirus (HPV) dose 1 and 2 vaccinations for adolescents aged 11‒14 years and herpes zoster vaccinations for people aged 70 years were assessed as monthly dose counts, by Indigenous status. As we analysed AIR data for the entire Victorian populations of the specified age groups (ie, not a population sample), we did not calculate confidence intervals for vaccination rates.
Neither stage 3 nor stage 4 lockdown restrictions were associated with marked changes in administration rates for diphtheria/tetanus/pertussis‐containing vaccine (dose 1: 2 months of age), 13‐valent pneumococcal conjugate vaccine (dose 2: 4 months of age), or measles/mumps/rubella vaccine (12 months of age) (Box 1).
About 20% fewer adolescents received first HPV vaccination doses in March 2020 than in March 2019, and 79% fewer in April 2020 than in April 2019 (schools closed: March‒April 2020), but numbers were subsequently higher, including during August‒October, when students again studied from home. Second HPV vaccination doses exhibited a similar pattern for March and April, but were lower during August–October (Box 2). The overall number of HPV 1 vaccination doses during 2020 was 0.2% lower than in 2019 (68 639 v 68 809), but 39% higher for Indigenous adolescents (1055 v 761); the overall number of second vaccination doses was 17.6% lower (51 403 v 62 419), but 10.3% higher for Indigenous adolescents (696 v 631).
The numbers of 70‐year‐old people who received zoster vaccine doses were lower in May, August, and September 2020 than in the corresponding 2019 months, but higher in March (perhaps because of the earlier influenza vaccination program), November, and December (Box 2). The overall number of people vaccinated was 3.8% lower in 2020 than in 2019 (14 801 v 15 387; Indigenous Australians, 22% lower: 325 v 414). Reporting of zoster vaccination of older adults to the AIR is known to be incomplete;6 if reporting was more complete in 2020 than 2019, we may have underestimated the change in doses administered.
In summary, the COVID‐19 epidemic did not markedly affect vaccination rates for young children in Victoria, despite the longest and most restrictive epidemic response measures in Australia. This finding, also reported for Australia in general,4 probably reflects effective messaging by health authorities that routine vaccination is an essential health service, the provision of COVID‐19‐safe vaccination services, continued engagement of parents and carers, and lower COVID‐19 rates than in many countries. As we assessed vaccination uptake for young children at an earlier time point than is usual (ie, timely vaccination), it will be important to monitor the effect of COVID‐19 on groups for whom timeliness of vaccination is known to be a problem, including Indigenous children.
HPV dose 1 vaccination of adolescents declined noticeably during the first but not the second epidemic wave, probably because the Victorian health department engaged with local councils to facilitate alternative delivery arrangements and supported general practitioners with promoting catch‐up vaccination by providing mainstream and social media information and resources for providers and parents.7 Zoster vaccination of older people, particularly Indigenous Australians, was also lower than usual, perhaps because they delayed routine vaccination as the result of concerns about the COVID‐19 infection risk.
We found that Victorian vaccination delivery was generally resilient in a period of unprecedented social and health care disruption.
Box 1 – Vaccination rates at 2, 4 and 12 month milestones for selected vaccine doses, assessed one month after scheduled vaccination dates for successive one‐month birth cohorts, Victoria, 2019 and 2020*
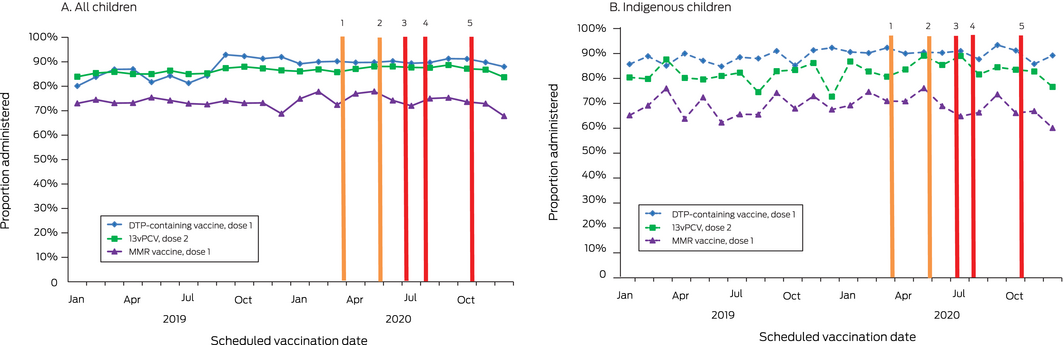
DTP = diphtheria/tetanus/pertussis; 13vPCV = 13‐valent pneumococcal conjugate vaccine; MMR = measles/mumps/rubella.
* Data source: Australian Immunisation Register.
COVID‐19‐related restrictions: 1. Stage 3 lockdown starts (23 March); 2. Stage 3 lockdown ends (partial return to school, 26 May; full return, 9 June); 3. Stage 3 lockdown starts (Melbourne, Mitchell Shire: 8 July); 4. Stage 4 lockdown (Melbourne), stage 3 lockdown (regional Victoria) starts (2 August); 5. Lockdown ends (regional Victoria, 12 October; Melbourne, 26 October).
Box 2 – Monthly administered vaccination doses: human papillomavirus vaccinations for adolescents (11‒14 years; doses 1 and 2) and zoster vaccinations for adults (70 years), Victoria, 2019 and 2020*
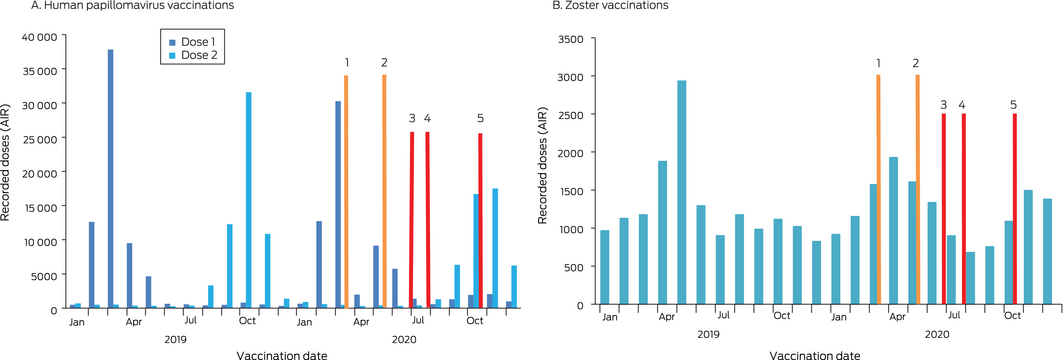
* Data source: Australian Immunisation Register.
COVID‐19‐related restrictions: 1. Stage 3 lockdown starts (23 March); 2. Stage 3 lockdown ends (partial return to school, 26 May; full return, 9 June); 3. Stage 3 lockdown starts (Melbourne, Mitchell Shire: 8 July); 4. Stage 4 lockdown (Melbourne), stage 3 lockdown (regional Victoria) starts (2 August); 5. Lockdown ends (regional Victoria, 12 October; Melbourne, 26 October).
Received 17 December 2020, accepted 26 May 2021
- 1. World Health Organization. WHO and UNICEF warn of a decline in vaccinations during COVID‐19 [media release]. 15 July 2020. https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19 (viewed Dec 2020).
- 2. Santoli JM, Lindley MC, DeSilva MB, et al. Effects of the COVID‐19 pandemic on routine pediatric vaccine ordering and administration: United States, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 591–593.
- 3. Public Health England. Impact of COVID‐19 on childhood vaccination counts to week 43, and vaccine coverage to September 2020 in England: interim analyses [Health Protection Report 14/21]. 10 Nov 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/933545/hpr2120_chldhd-vc_wk43.pdf (viewed Nov 2020).
- 4. National Centre for Immunisation Research and Surveillance. COVID‐19: impact on routine childhood vaccination uptake in Australia. 10 Nov 2020. https://www.ncirs.org.au/sites/default/files/2020-11/COVID-19_Impact_Analysis_Final%20Report.pdf (viewed Dec 2020).
- 5. Hull B, Hendry A, Dey A, et al. Immunisation coverage annual report 2019. Commun Dis Intell (2018); 2021: 45.
- 6. Hull B, Hendry A, Dey A, et al. Exploratory analysis of the first 2 years of adult vaccination data recorded on AIR. Nov 2019. http://ncirs.org.au/sites/default/files/2019-12/Analysis%20of%20adult%20vaccination%20data%20on%20AIR_Nov%202019.pdf (viewed Dec 2020).
- 7. Victorian Department of Health and Human Services. Secondary school immunisation program 2020 during COVID: advice for parents and guardians. 3 Aug 2020. https://www2.health.vic.gov.au/about/publications/factsheets/sec-school-immunisation-2020-covid-fs-parents (viewed Dec 2020).





No relevant disclosures.