The known: The management of patients in Australia presenting to hospital with acute coronary syndrome is reported to differ according to whether the hospital of first presentation can provide cardiac catheterisation.
The new: For Australian hospitals enrolled in the CONCORDANCE clinical quality registry, differences in catheterisation rates and major outcomes between patients who initially present to catheterisation‐capable or non‐capable hospitals are not as large as found by earlier studies.
The implications: Improved access to angiographic facilities across the Australian health care system has largely overcome challenges to providing equitable outcomes for all patients with acute coronary syndromes.
Invasive coronary angiography during hospital admission reduces the frequency of adverse outcomes (mortality, recurrent myocardial infarction, stroke) for patients with non‐ST elevation acute coronary syndromes (NSTEACS).1 Guidelines recommend and immediate invasive strategy (within two hours of admission) for patients at very high risk, an early invasive strategy (within 24 hours) for patients at high risk, and an invasive strategy (within 72 hours) for patients at intermediate risk of cardiovascular events.2 Similarly, time is critical when treating patients with an ST elevation myocardial infarction (STEMI).3 Reperfusion can be achieved by primary percutaneous coronary intervention (PCI) or fibrinolysis, but PCI is preferred if readily available, because of its better outcomes.4 Further, emergency angiography is required for 18‒32% of patients in whom fibrinolysis fails to achieve reperfusion, and angiography within 3‒24 hours of fibrinolysis is recommended for all other patients to treat residual stenoses and to limit re‐occlusion.2
Timely access to angiography is consequently advocated by Australian guidelines as an important component of care for patients with acute coronary syndrome (ACS).2 However, inequities in access have been described, driven in part by geographic challenges, and may be associated with poorer outcomes for patients presenting to hospitals that cannot provide angiography.5,6,7,8,9
The aims of our study were to determine whether the availability of invasive coronary angiography at the hospital of presentation influences catheterisation rates for patients presenting with ACS; whether the clinical and risk characteristics of patients selected for angiography differ between hospitals of presentation according to whether they have on‐site catheterisation laboratories; and whether presenting to a catheterisation‐capable hospital is associated with better outcomes for patients with ACS.
Methods
We analysed data from the Cooperative National Registry of Acute Coronary Events (CONCORDANCE). The registry collected information on patients who presented with ACS from the medical records of 43 metropolitan and regional hospitals from all Australian states and territories during 23 February 2009 ‒ 16 October 2018 (Supporting Information, table 1).10 Catheterisation‐capable hospitals were defined as those with, and catheterisation non‐capable hospitals as those without cardiac catheterisation facilities. All patients were followed up by phone six months after discharge and again at 12 months (patients enrolled 2014‒2018) or 24 months (patients enrolled 2009‒2013).
Patients: eligibility criteria and classification
Eligible for inclusion in the CONCORDANCE registry were all patients over 18 years of age admitted to hospital with presumed ACS who had elevated cardiac biomarker levels, an electrocardiographic abnormality, prior history of coronary heart disease, newly documented coronary heart disease, or two high risk features predictive of recurrent in‐hospital events: haemodynamic compromise (systolic blood pressure less than 90 mmHg and heart rate exceeding 100 per minute), left ventricular systolic dysfunction (left ventricular ejection fraction less than 0.40%), diabetes, or chronic kidney disease (estimated glomerular filtration rate less than 60 mL/min/1.73 m2).
We included patients with confirmed ACS for whom the index admission hospital contributed data to CONCORDANCE, so that complete medical history and in‐hospital data were available for analysis. Patients were first classified according to whether they were admitted to hospitals with or without on‐site cardiac catheterisation facilities; the catheterisation laboratory status did not change for any included hospital during the study period. Patients were then classified according to whether they underwent cardiac catheterisation during their index admission.
Outcomes
Outcomes were major adverse cardiovascular events (MACE) — myocardial infarction, stroke, congestive heart failure, shock, or cardiovascular death — and all‐cause deaths in hospital and by follow‐up at 12 or 24 months. The process measure was prescription on discharge of at least four of five indicated evidence‐based medication types: aspirin, platelet ADP receptor‐inhibiting agents (clopidogrel, prasugrel, or ticagrelor), a statin or other lipid‐lowering medication, beta blockers, and angiotensin‐converting enzyme inhibitors or angiotensin receptor blockers.
Statistical analysis
Missing baseline categorical data were recoded as “no” or “normal”; that is, if something was not documented, it was deemed not to have been present. Analyses were not adjusted for other missing data. Demographic data, clinical characteristics, in‐hospital management, and events were compared for patients who presented to catheterisation‐capable and non‐capable hospitals. Categorical data are summarised as numbers and proportions; the statistical significance of differences was assessed in Rao‒Scott χ2 tests. Continuous data were summarised as means with standard deviation (SDs) and compared in unadjusted regression analyses in a generalised estimating equations (GEE) framework with an exchangeable correlation matrix. The normality of continuous data was assessed in Kolmogorov‒Smirnov tests. Rao‒Scott testing and the GEE analysis each accounted for clustering by hospital.
We assessed factors associated with outcomes by multivariable logistic regression in a GEE framework. For in‐hospital outcomes, we included cardiac catheterisation, age (four categories), sex, Indigenous status, diabetes, peripheral artery disease, history of myocardial infarction, congestive heart failure, chronic renal failure, dementia, ACS diagnosis, catheterisation laboratory availability, urban/rural hospital, and hospital size (bed number; three groups) as independent variables. For follow‐up outcomes, we included these variables as well as referral to a cardiac rehabilitation program and discharge prescription of four or more of the five evidence‐based medication types. P < 0.05 (two‐tailed) was deemed statistically significant. Statistical analyses were conducted in SAS 9.4.
Ethics approval
Ethics approval for our study was granted by the human research ethics committee of the Concord Repatriation General Hospital (reference, HREC/08/CRGH/180). Each participating site had appropriate approval for data collection.
Results
CONCORDANCE data were available for 8245 patients: 5637 (68%) who had presented to 31 catheterisation‐capable hospitals and 2608 (32%) who had presented to 12 catheterisation non‐capable hospitals. The proportion of women among patients who presented to catheterisation‐capable hospitals was smaller than for catheterisation non‐capable hospitals (1575 [28%]) v 873 [33%]), but the mean ages of all patients were similar (65.3 years [SD, 13.4 years] v 66.7 years [SD, 13.5 years]). The proportions of patients with hypertension (3471 [62%] v 1730 [66%]), chronic renal failure (438 [8%] v 310 [12%]), prior stroke (409 [7%] v 242 [9%]), and prior myocardial infarction (1705 [30%] v 922 [35%]) were significantly lower for patients who presented to catheterisation‐capable hospitals, and that of patients diagnosed with STEMI significantly higher (1786 [32%] v 510 [20%]) (Box 1). At total of 1144 patients could not be contacted for the 6‐month follow‐up, and 2924 patients could not be contacted for the 12‐ or 24‐month follow‐up.
Cardiac catheterisation and revascularisation
The proportions of patients who underwent cardiac catheterisation (4557 [81%] v 1832 [70%]) or PCI (2739 [49%] v 915 [35%]) were each higher for those who presented to catheterisation‐capable hospitals (Box 2). Catheterisation rates for people who presented to catheterisation‐capable hospitals were higher than for those who presented to catheterisation non‐capable hospitals for all ACS diagnoses: STEMI, 1698 (95%) v 454 (89%); non‐STEMI (NSTEMI), 2170 (82%) v 1067 (74%); unstable angina, 689 (58%) v 311 (47%). The baseline characteristics of patients admitted to hospitals with or without catheterisation facilities were similar, both for those who underwent cardiac catheterisation (Supporting Information, table 2) and those who did not (Supporting Information, table 3). A larger proportion of patients who presented to catheterisation‐capable hospitals were discharged with at least four of the five evidence‐based medication types than of those who presented to hospitals without catheterisation facilities (4033 [72%] v 1728 [66%]) (Box 2).
Patient outcomes in catheterisation‐capable and catheterisation non‐capable hospitals
In‐hospital outcomes during the index admission were similar for hospitals with and without catheterisation facilities (MACE: 712 [13%] v 326 [13%]; all‐cause death, 219 [4%] v 93 [4%]) (Box 3), as were outcomes at 6‐month (MACE 283 [6%] v 154 [7%]; all‐cause deaths, 146 [3%] v 90 [4%]; Box 4) and 12‐ or 24‐month follow‐up (MACE, 169 [32%] v 93 [36%]; all‐cause deaths, 99 [3%] v 48 [3%]; Box 5).
Factors associated with adverse outcomes: in‐hospital outcomes
Presenting to a hospital with a catheterisation laboratory did not influence the frequency of in‐hospital MACE (adjusted odds ratio [aOR], 0.90; 95% confidence interval [CI], 0.55–1.48) or death (aOR, 1.11; 95% CI, 0.76–1.62). Undergoing cardiac catheterisation was associated with lower rates of MACE (aOR, 0.48; 95% CI, 0.38–0.61) and death (aOR, 0.07; 95% CI, 0.04–0.13) (Box 6; online Supporting Information, figure 1).
The odds of in‐hospital MACE was higher for older patients, for patients with diabetes, chronic renal failure, or dementia or cognitive impairment; it was higher for patients diagnosed with STEMI or NSTEMI than for those diagnosed with unstable angina (Box 6).
The odds of in‐hospital death were higher for older patients, for patients with prior myocardial infarction, chronic renal failure, or dementia or cognitive impairment; they were higher for patients diagnosed with STEMI or NSTEMI than for those diagnosed with unstable angina (Supporting Information, figure 1).
Factors associated with adverse outcomes: six‐month follow‐up
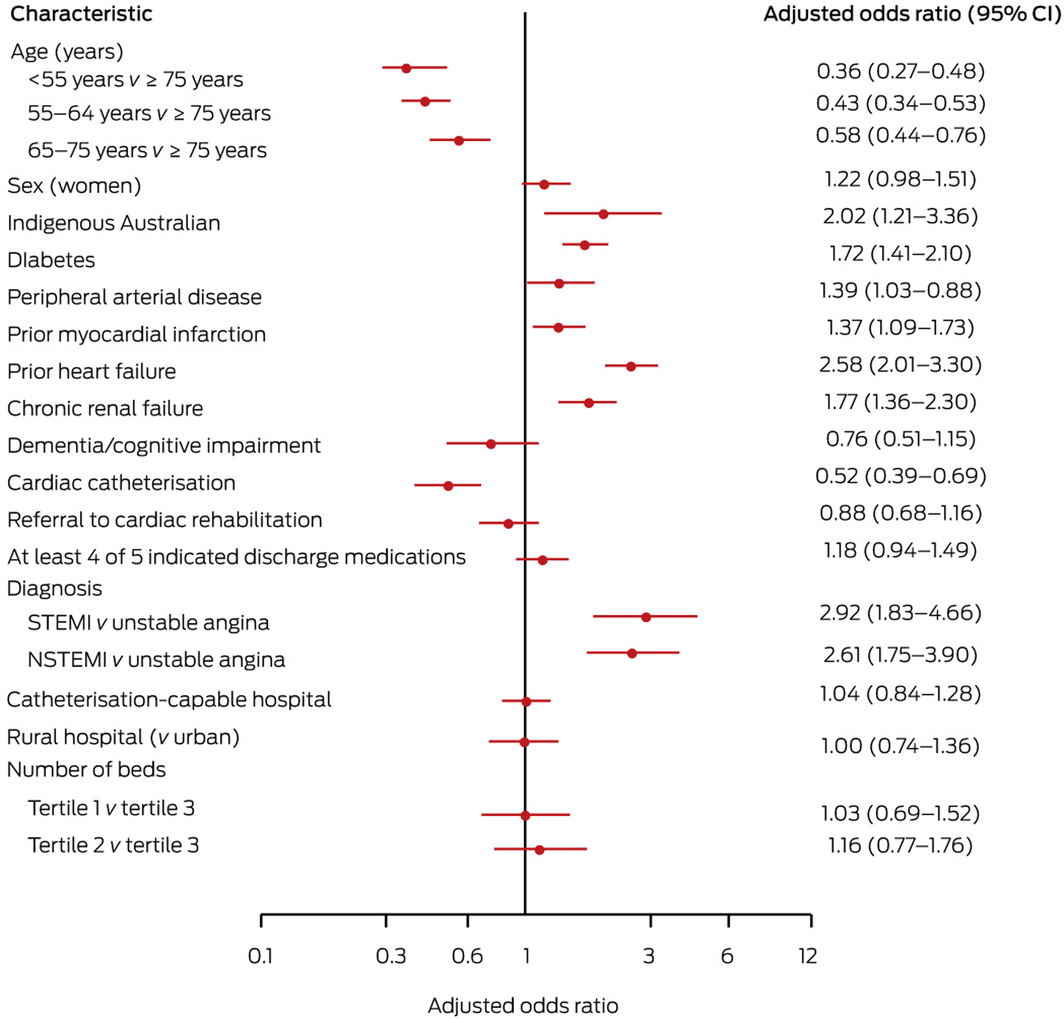
Six‐month follow‐up was completed for 6759 patients (82%); the baseline characteristics of patients followed up and those not followed up were similar (Supporting Information, table 4). Presenting to a hospital with a catheterisation laboratory did not influence the odds of MACE (aOR, 1.04; 95% CI, 0.84–1.28) or death by six months (aOR, 1.01; 95% CI, 0.61–1.68). Undergoing cardiac catheterisation was associated with lower rates of MACE (aOR, 0.52; 95% CI, 0.39–0.69) and death (aOR, 0.60; 95% CI, 0.42‒0.86) (Box 7; Supporting Information, figure 2).
The odds of MACE by 6‐month follow‐up they were higher for older patients, for patients with diabetes mellitus, peripheral arterial disease, prior myocardial infarction or heart failure, or chronic renal failure, and for Indigenous Australian patients; they were higher for patients diagnosed with STEMI or NSTEMI than for those diagnosed with unstable angina (Box 7).
The odds of death by 6‐month follow‐up were higher for older patients, for patients with prior heart failure, chronic renal failure, or dementia or cognitive impairment, and for Indigenous Australian patients; they were higher for patients diagnosed with STEMI or NSTEMI than for those diagnosed with unstable angina. It was lower for patients referred to cardiac rehabilitation (Supporting Information, figure 2).
Factors associated with adverse outcomes: 12‐ or 24‐month follow‐up
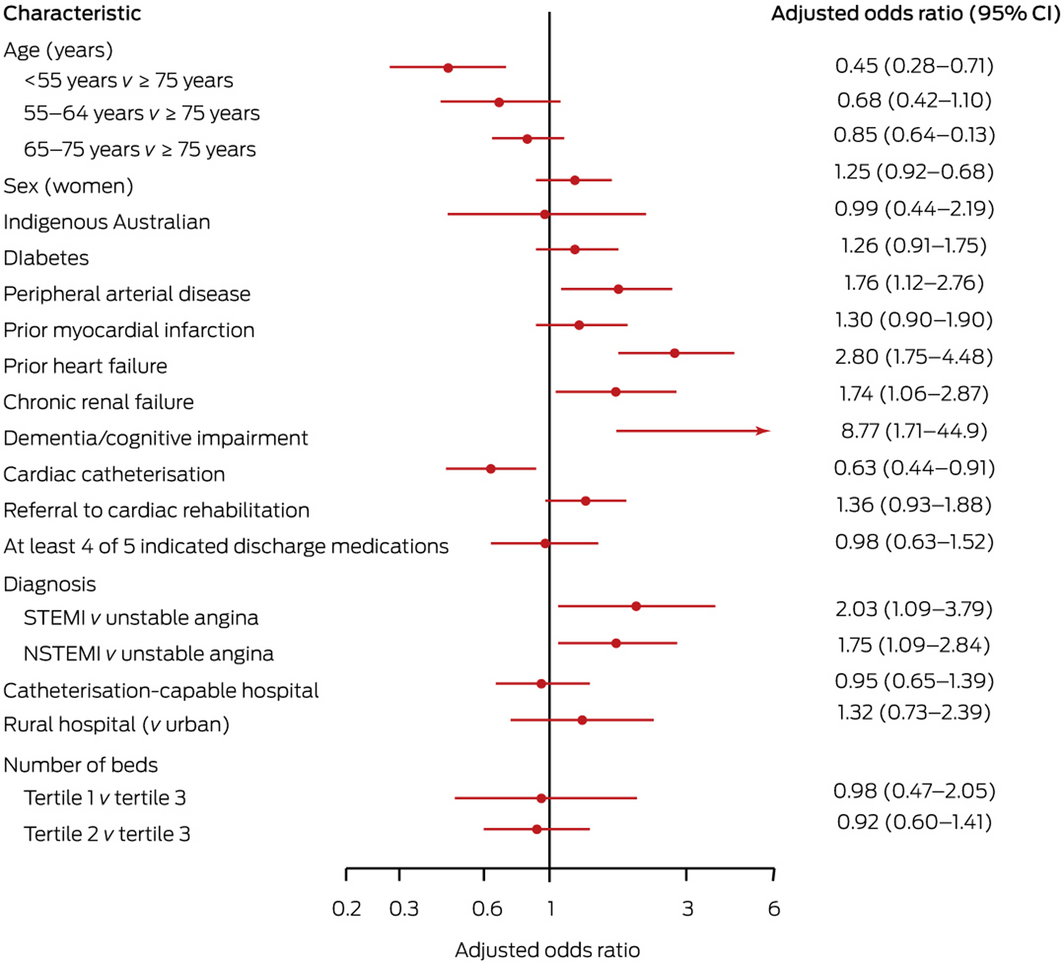
Twelve‐ or 24‐month follow‐up was completed for 4979 patients (60%); the baseline characteristics of patients followed up and those not followed up were similar (Supporting Information, table 5). Presenting to a hospital with a catheterisation laboratory did not influence the odds of MACE (aOR, 0.95; 95% CI, 0.65–1.39) or death (aOR, 1.11; 95% CI, 0.61–2.04). Undergoing cardiac catheterisation was associated with lower rates of MACE (aOR, 0.63; 95% CI, 0.44–0.91) and death (aOR, 0.50; 95% CI, 0.33–0.74) (Box 8, Supporting Information, figure 3).
The odds of MACE by 12‐ or 24‐month follow‐up were higher for patients with peripheral arterial disease, prior heart failure, chronic renal failure, or dementia or cognitive impairment; they were higher for patients diagnosed with STEMI or NSTEMI than for those diagnosed with unstable angina (Box 8).
The odds of death by 12‐ or 24‐month follow‐up were higher for older patients, and for patients with prior myocardial infarction or heart failure or chronic renal failure; they were higher for patients diagnosed with NSTEMI than for those diagnosed with unstable angina, and lower for those referred to cardiac rehabilitation (Supporting Information, figure 3).
Discussion
In our comprehensive analysis of 8245 patients who presented with ACS to 43 Australian hospitals during 2009–2018, the availability of coronary angiography at the hospital of presentation influenced catheterisation rates. However, the clinical characteristics of patients who underwent catheterisation were similar for both hospital categories, which suggests that practice patterns and decisions to offer invasive treatment are similar in both settings. Despite differences in the proportions of patients who ultimately underwent catheterisation, outcomes for patients with ACS who presented to catheterisation‐capable and non‐capable hospitals were similar, suggesting that they are not significantly influenced by the availability of on‐site coronary angiography in the hospital of presentation.
The angiography rates we report — 81% in catheterisation‐capable hospitals, 70% in hospitals without these facilities — are higher than those found by previous studies. The Heart Protection Project, conducted in 27 Australian hospitals during 2003–2005,7 reported invasive angiography rates of 66.4% in catheterisation‐capable and 20.1% in catheterisation non‐capable hospitals; the 2012 SNAPSHOT ACS audit (Australia and New Zealand) reported rates of 61.5% and 50.8% respectively.6 The differences presumably reflect growing acceptance of coronary angiography as the standard of care for patients with ACS at high risk of cardiovascular events, and the increased capacity to transfer patients to catheterisation‐capable hospitals that contribute data to the CONCORDANCE registry.
Despite differences in the proportions who received angiography after presenting to catheterisation‐capable and non‐capable hospitals, the clinical characteristics of patients selected for angiography were similar. Diagnoses of STEMI were more frequent among people who presented to hospitals with catheterisation laboratories, probably reflecting pre‐hospital triage of patients and direction of patients with STEMI to primary PCI hospitals. This could also explain the mildly higher comorbidity rates (prior myocardial infarction, prior stroke, hypertension, chronic renal failure) among patients presenting to hospitals without catheterisation facilities, reflecting the higher proportion of patients with NSTEACS. Similarly, catheterisation rates were higher among patients presenting to catheterisation‐capable hospitals for all ACS diagnoses, probably reflecting greater comorbidity among patients who presented to catheterisation non‐capable hospitals.12
Outcomes in hospital and at 6 and 12 or 24 months after discharge were similar for patients admitted to catheterisation‐capable and non‐capable hospitals. A number of baseline characteristics — prior heart failure, chronic renal failure, peripheral arterial disease, diabetes mellitus, dementia or cognitive impairment, and diagnoses of STEMI and NSTEMI — were associated with poor outcomes in both the short and long terms, consistent with previous reports.13 After adjusting for these factors, cardiac catheterisation was associated with lower incidence of MACE and death at all time points, indicating the importance of invasive coronary angiography and appropriate revascularisation. Importantly, patients with similar characteristics were offered cardiac catheterisation, regardless of whether the hospital to which they presented had a catheterisation laboratory or not, suggesting that triage and transfer systems in hospitals enrolled in CONCORDANCE are sufficiently mature to overcome previously documented inequities in access to invasive procedures.5,6,7,9
Limitations
Confounding in our retrospective cohort study and loss of patients to follow‐up may have affected our findings. While the CONCORDANCE registry included both urban and rural tertiary hospitals from all Australian states and territories, smaller hospitals in rural and remote areas were not included; our findings may not reflect practice in these less well resourced hospitals. Analyses were not adjusted for multiple comparisons.
Conclusions
It has been reported that the management of patients presenting with ACS to Australian hospitals differed according to whether the hospital of first presentation had a catheterisation laboratory.6,7 We found, however, that catheterisation rates were higher than previously reported, regardless of whether the hospital of presentation was catheterisation‐capable or not. Adverse outcomes were less frequent among patients who received coronary angiography, and patients with similar characteristics received this treatment, whether they presented to catheterisation‐capable or non‐capable hospitals, consistent with the similar outcomes for these patients.
Box 1 – Baseline characteristics of the 8245 patients admitted to hospital with presumed acute coronary syndrome, Australia, Feb 2009 – Oct 2018
|
Characteristic |
Catheterisation‐capable hospital |
Catheterisation non‐capable hospital |
Total |
P |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
5637 |
2608 |
8245 |
|
|||||||||||
|
Age (years), mean (SD) |
65.3 (13.4) |
66.7 (13.5) |
65.8 (13.4) |
0.41 |
|||||||||||
|
Age group (years) |
|
|
|
0.17 |
|||||||||||
|
< 55 |
1214 (22%) |
512 (20%) |
1726 (21%) |
|
|||||||||||
|
55–64 |
1450 (26%) |
561 (22%) |
2011 (24%) |
|
|||||||||||
|
65–74 |
1494 (27%) |
722 (28%) |
2216 (27%) |
|
|||||||||||
|
≥ 75 |
1460 (26%) |
809 (31%) |
2269 (28%) |
|
|||||||||||
|
Sex (women) |
1575 (28%) |
873 (33%) |
2448 (30%) |
< 0.001 |
|||||||||||
|
Body mass index (kg/m2) |
|
|
|
0.43 |
|||||||||||
|
< 18 (underweight) |
38 (1%) |
21 (2%) |
59 (1%) |
|
|||||||||||
|
18 to < 25 (healthy) |
988 (26%) |
344 (26%) |
1332 (26%) |
|
|||||||||||
|
25 to < 30 (overweight) |
1490 (39%) |
488 (37%) |
1978 (38%) |
|
|||||||||||
|
≥ 30 (obese) |
1314 (34%) |
480 (36%) |
1794 (35%) |
|
|||||||||||
|
Indigenous Australians |
199 (4%) |
202 (8%) |
401 (5%) |
0.28 |
|||||||||||
|
Smoking history |
|
|
|
0.66 |
|||||||||||
|
Never smoked |
2143 (38%) |
1057 (41%) |
3200 (39%) |
|
|||||||||||
|
Ex‐smoker |
2008 (36%) |
908 (35%) |
2916 (35%) |
|
|||||||||||
|
Current smoker |
1474 (26%) |
630 (24%) |
2104 (26%) |
|
|||||||||||
|
Comorbid conditions |
|
|
|
|
|||||||||||
|
Hypertension |
3471 (62%) |
1730 (66%) |
5201 (63%) |
0.003 |
|||||||||||
|
Diabetes |
1550 (27%) |
809 (31%) |
2359 (29%) |
0.14 |
|||||||||||
|
Dyslipidaemia |
3125 (56%) |
1538 (59%) |
4663 (57%) |
0.11 |
|||||||||||
|
Peripheral arterial disease |
336 (6%) |
188 (7%) |
524 (6%) |
0.20 |
|||||||||||
|
Prior myocardial infarction |
1705 (30%) |
922 (35%) |
2627 (32%) |
0.008 |
|||||||||||
|
Prior percutaneous coronary intervention |
1235 (22%) |
635 (24%) |
1870 (23%) |
0.10 |
|||||||||||
|
Prior coronary artery bypass graft |
662 (12%) |
350 (13%) |
1012 (12%) |
0.21 |
|||||||||||
|
Prior heart failure |
452 (8%) |
229 (9%) |
681 (8%) |
0.48 |
|||||||||||
|
Prior stroke/transient ischemic attack |
409 (7%) |
242 (9%) |
651 (8%) |
0.041 |
|||||||||||
|
Chronic renal failure |
438 (8%) |
310 (12%) |
748 (9%) |
< 0.001 |
|||||||||||
|
Dementia/cognitive impairment |
161 (3%) |
103 (4%) |
264 (3%) |
0.08 |
|||||||||||
|
Killip class |
|
|
|
0.40 |
|||||||||||
|
1 |
4955 (88%) |
2302 (88%) |
7257 (88%) |
|
|||||||||||
|
2 |
538 (10%) |
230 (9%) |
768 (9%) |
|
|||||||||||
|
3 |
100 (2%) |
65 (2%) |
165 (2%) |
|
|||||||||||
|
4 |
44 (1%) |
11 (< 1%) |
55 (1%) |
|
|||||||||||
|
GRACE risk score, mean (SD) |
108.2 (31.9) |
108.6 (32.3) |
108.3 (32.0) |
0.66 |
|||||||||||
|
Cardiac arrest on admission |
236 (4%) |
73 (3%) |
309 (4%) |
0.040 |
|||||||||||
|
Diagnosis |
|
|
|
0.001 |
|||||||||||
|
ST‐elevation myocardial infarction |
1786 (32%) |
510 (20%) |
2296 (28%) |
|
|||||||||||
|
Non‐ST‐elevation myocardial infarction |
2661 (47%) |
1442 (55%) |
4103 (50%) |
|
|||||||||||
|
Unstable angina |
1187 (21%) |
655 (25%) |
1842 (22%) |
|
|||||||||||
|
Admitted to a rural hospital |
1429 (25%) |
1647 (63%) |
3076 (37%) |
0.06 |
|||||||||||
|
Beds in hospitals |
|
|
|
< 0.001 |
|||||||||||
|
Tertile 1 (< 330) |
671 (12%) |
1817 (70%) |
2488 (30%) |
|
|||||||||||
|
Tertile 2 (330–600) |
2246 (40%) |
561 (22%) |
2807 (34%) |
|
|||||||||||
|
Tertile 3 (> 600) |
2720 (48%) |
230 (9%) |
2950 (36%) |
|
|||||||||||
|
|
|||||||||||||||
|
GRACE = Global Registry of Acute Coronary Events;11 SD = standard deviation. |
|||||||||||||||
Box 2 – Hospital investigations and treatment, and discharge medications for 8245 patients admitted with presumed acute coronary syndrome, Australia, Feb 2009 – Oct 2018
|
Characteristic |
Catheterisation‐capable hospital |
Catheterisation non‐capable hospital |
Total |
P |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
5637 |
2608 |
8245 |
|
|||||||||||
|
Cardiac catheterisation |
4557 (81%) |
1832 (70%) |
6387 (78%) |
< 0.001 |
|||||||||||
|
Revascularisation (any type) |
3153 (56%) |
1131 (43%) |
4284 (52%) |
0.001 |
|||||||||||
|
Coronary artery bypass graft |
446 (8%) |
224 (9%) |
670 (8%) |
0.47 |
|||||||||||
|
Percutaneous coronary intervention |
2739 (49%) |
915 (35%) |
3654 (44%) |
< 0.001 |
|||||||||||
|
Percutaneous coronary intervention: type |
|
|
|
< 0.001 |
|||||||||||
|
Primary |
1606 [59%] |
107 [12%] |
1713 [47%] |
|
|||||||||||
|
Rescue |
170 [6%] |
170 [19%] |
340 [9%] |
|
|||||||||||
|
Other |
962 [35%] |
637 [70%] |
1599 [44%] |
|
|||||||||||
|
Discharge medications |
|
|
|
|
|||||||||||
|
Aspirin |
4811 (85%) |
2179 (84%) |
6990 (85%) |
0.31 |
|||||||||||
|
Clopidogrel |
2388 (42%) |
1283 (49%) |
3671 (45%) |
0.06 |
|||||||||||
|
Prasugrel |
302 (5%) |
39 (1%) |
341 (4%) |
< 0.001 |
|||||||||||
|
Ticagrelor |
1081 (19%) |
318 (12%) |
1399 (17%) |
0.08 |
|||||||||||
|
Coplavix (clopidogrel/aspirin) |
212 (4%) |
69 (3%) |
281 (3%) |
0.36 |
|||||||||||
|
Lipid‐lowering agent |
5043 (89%) |
2243 (86%) |
7286 (88%) |
0.022 |
|||||||||||
|
Beta blocker |
4190 (74%) |
1885 (72%) |
6075 (74%) |
0.30 |
|||||||||||
|
Angiotensin‐converting enzyme inhibitors or angiotensin receptor blockers |
3905 (69%) |
1721 (66%) |
5626 (68%) |
0.14 |
|||||||||||
|
Four or more evidence‐based medicine types |
4033 (72%) |
1728 (66%) |
5761 (70%) |
0.018 |
|||||||||||
|
Anticoagulant |
487 (9%) |
282 (11%) |
769 (9%) |
< 0.001 |
|||||||||||
|
Referral to cardiac rehabilitation |
3488 (62%) |
1565 (61%) |
5053 (62%) |
0.85 |
|||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – In‐hospital outcomes for 8245 patients admitted to hospital with presumed acute coronary syndrome, Australia, Feb 2009 – Oct 2018
|
Outcome |
Catheterisation‐capable hospital |
Catheterisation non‐capable hospital |
Total |
P |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
5637 |
2608 |
8245 |
|
|||||||||||
|
Major adverse cardiac events* |
712 (13%) |
326 (13%) |
1038 (13%) |
0.84 |
|||||||||||
|
Myocardial infarction |
133 (2%) |
55 (2%) |
188 (2%) |
0.73 |
|||||||||||
|
Stroke |
31 (1%) |
21 (1%) |
52 (1%) |
0.16 |
|||||||||||
|
Congestive heart failure |
478 (9%) |
214 (8%) |
692 (9%) |
0.97 |
|||||||||||
|
Cardiovascular death |
192 (3%) |
83 (3%) |
275 (3%) |
0.82 |
|||||||||||
|
All‐cause deaths |
219 (4%) |
93 (4%) |
312 (4%) |
0.74 |
|||||||||||
|
Renal failure |
329 (6%) |
125 (5%) |
454 (6%) |
0.29 |
|||||||||||
|
Major bleeding |
428 (8%) |
191 (7%) |
619 (8%) |
0.83 |
|||||||||||
|
Cardiogenic shock |
186 (3%) |
51 (2%) |
237 (3%) |
< 0.001 |
|||||||||||
|
|
|||||||||||||||
|
* Myocardial infarction, stroke, congestive heart failure, cardiogenic shock, or cardiovascular death. |
|||||||||||||||
Box 4 – Outcomes by 6‐month follow‐up for 6759 patients admitted to hospital with presumed acute coronary syndrome, Australia, Feb 2009 – Oct 2018
|
Outcome |
Catheterisation‐capable hospital |
Catheterisation non‐capable hospital |
Total |
P |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
4642 |
2117 |
6759 |
|
|||||||||||
|
Major adverse cardiac events* |
283 (6%) |
154 (7%) |
437 (7%) |
0.18 |
|||||||||||
|
Myocardial infarction |
120 (3%) |
65 (3%) |
185 (3%) |
0.51 |
|||||||||||
|
Stroke |
22 (0%) |
14 (1%) |
36 (1%) |
0.41 |
|||||||||||
|
Congestive heart failure |
138 (3%) |
79 (4%) |
217 (3%) |
0.11 |
|||||||||||
|
Cardiovascular death |
48 (1%) |
24 (1%) |
72 (1%) |
0.81 |
|||||||||||
|
All‐cause deaths |
146 (3%) |
90 (4%) |
236 (4%) |
0.09 |
|||||||||||
|
Major bleeding |
34 (1%) |
26 (1%) |
60 (1%) |
0.12 |
|||||||||||
|
Re‐hospitalised for heart disease or a bleeding event |
941 (21%) |
478 (23%) |
1419 (22%) |
0.25 |
|||||||||||
|
|
|||||||||||||||
|
* Myocardial infarction, stroke, congestive heart failure, cardiogenic shock, or cardiovascular death. |
|||||||||||||||
Box 5 – Outcomes by 12‐ or 24‐month follow‐up for 4979 patients admitted to hospital with presumed acute coronary syndrome, Australia, Feb 2009 – Oct 2018
|
Outcome |
Catheterisation‐capable hospital |
Catheterisation non‐capable hospital |
Total |
P |
|||||||||||
|
|
|||||||||||||||
|
Number of patients |
3592 |
1387 |
4979 |
|
|||||||||||
|
Major adverse cardiac events* |
169 (32%) |
93 (36%) |
262 (33%) |
0.23 |
|||||||||||
|
Myocardial infarction |
86 (17%) |
46 (18%) |
132 (17%) |
0.53 |
|||||||||||
|
Stroke |
13 (2%) |
11 (4%) |
24 (3%) |
0.06 |
|||||||||||
|
Congestive heart failure |
80 (15%) |
40 (16%) |
120 (15%) |
0.86 |
|||||||||||
|
Cardiovascular death |
28 (1%) |
9 (1%) |
37 (1%) |
0.58 |
|||||||||||
|
All‐cause deaths |
99 (3%) |
48 (3%) |
147 (3%) |
0.32 |
|||||||||||
|
Major bleeding |
31 (6%) |
16 (6%) |
47 (6%) |
0.85 |
|||||||||||
|
Re‐hospitalised for heart disease or a bleeding event |
523 (15%) |
253 (18%) |
776 (16%) |
0.10 |
|||||||||||
|
|
|||||||||||||||
|
* Myocardial infarction, stroke, congestive heart failure, cardiogenic shock, or cardiovascular death. |
|||||||||||||||
Box 6 – Predictors of in‐hospital major adverse cardiovascular events (MACE): multivariable analysis
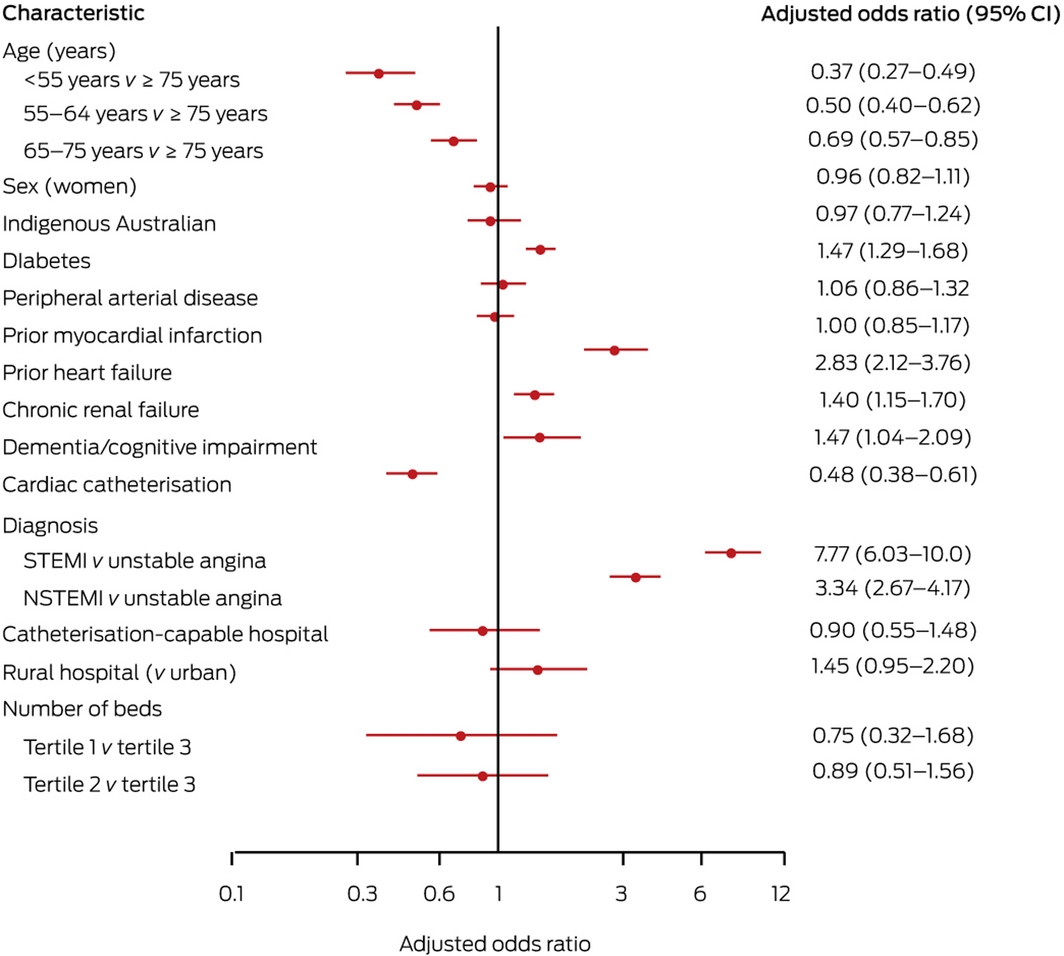
* CI = confidence interval; STEMI = ST‐elevation myocardial infarction; NSTEMI = non‐ST‐elevation myocardial infarction.
Received 25 June 2020, accepted 26 October 2020
- Michael Ayad1
- Karice Hyun2,3
- Mario D’Souza2
- Julie Redfern3
- Janice Gullick4
- Mark Ryan5
- David B Brieger2
- 1 The University of Sydney, Sydney, NSW
- 2 Concord Repatriation General Hospital, Sydney, NSW
- 3 Westmead Clinical School, University of Sydney, Sydney, NSW
- 4 Sydney Nursing School, University of Sydney, Sydney, NSW
- 5 Shoalhaven District Memorial Hospital, Nowra, NSW
The CONCORDANCE registry was supported by unrestricted educational grants from Astra Zeneca, Sanofi Aventis, Merck Sharpe and Dohme/Schering joint venture, Eli Lilly, Boehringer Ingelheim, and the National Heart Foundation of Australia. We thank the CONCORDANCE investigators and their patients who contributed data to this registry.
No relevant disclosures.
- 1. Hoenig MR, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina and non‐ST elevation myocardial infarction in the stent era. Cochrane Database Syst Rev 2010; CD004815.
- 2. Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Heart Lung Circ 2016; 25: 895–951.
- 3. Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 1996; 348: 771–775.
- 4. Kumar A, Cannon CP. Acute coronary syndromes: diagnosis and management, part II. Mayo Clin Proc 2009; 84: 1021–1036.
- 5. Chew DP, Amerena JV, Coverdale SG, et al. Invasive management and late clinical outcomes in contemporary Australian management of acute coronary syndromes: observations from the ACACIA registry. Med J Aust 2008; 188: 691–697. https://www.mja.com.au/journal/2008/188/12/invasive-management-and-late-clinical-outcomes-contemporary-australian
- 6. Chew DP, French J, Briffa TG, et al. Acute coronary syndrome care across Australia and New Zealand: the SNAPSHOT ACS study. Med J Aust 2013; 199: 185–191. https://www.mja.com.au/journal/2013/199/3/acute-coronary-syndrome-care-across-australia-and-new-zealand-snapshot-acs-study
- 7. Walters DL, Aroney CN, Chew DP, et al. Variations in the application of cardiac care in Australia. Med J Aust 2008; 188: 218–223. https://www.mja.com.au/journal/2008/188/4/variations-application-cardiac-care-australia
- 8. Astley CM, Ranasinghe I, Brieger D, et al. Expertise and infrastructure capacity impacts acute coronary syndrome outcomes. Aust Health Rev 2018; 42: 277–285.
- 9. Brieger DB, Chew DP, Redfern J, et al. Survival after an acute coronary syndrome: 18‐month outcomes from the Australian and New Zealand SNAPSHOT ACS study. Med J Aust 2015; 203: 368. https://www.mja.com.au/journal/2015/203/9/survival-after-acute-coronary-syndrome-18-month-outcomes-australian-and-new
- 10. Aliprandi‐Costa B, Ranasinghe I, Turnbull F, et al. The design and rationale of the Australian Cooperative National Registry of Acute Coronary care, Guideline Adherence and Clinical Events (CONCORDANCE). Heart Lung Circ 2013; 22: 533–541.
- 11. Fox KAA, Dabbous OH, Goldberg RJ, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 2006; 333: 1091.
- 12. Joynt KE, Huynh L, Amerena JV, et al. Impact of acute and chronic risk factors on use of evidence‐based treatments in patients in Australia with acute coronary syndromes. Heart 2009; 95: 1442–1448.
- 13. Kastorini CM, Georgousopoulou E, Vemmos KN, et al. Comparative analysis of cardiovascular disease risk factors influencing nonfatal acute coronary syndrome and ischemic stroke. Am J Cardiol 2013; 112: 349–354.





Abstract
Objective: To determine whether the availability of invasive coronary angiography at the hospital of presentation influences catheterisation rates for patients with acute coronary syndrome (ACS), and whether presenting to a catheterisation‐capable hospital is associated with better outcomes for patients with ACS.
Design, setting: Retrospective cohort study; analysis of Cooperative National Registry of Acute Coronary Events (CONCORDANCE) data.
Setting, participants: Adults admitted with ACS to 43 Australian hospitals (including 31 catheterisation‐capable hospitals), February 2009 – October 2018.
Main outcome measures: Major adverse cardiovascular events (myocardial infarction, stroke, congestive heart failure, cardiogenic shock, cardiovascular death) and all‐cause deaths in hospital and by six and 12‐ or 24‐month follow‐up.
Results: The proportion of women among the 5637 patients who presented to catheterisation‐capable hospitals was smaller than for the 2608 patients who presented to hospitals without catheterisation facilities (28% v 33%); the proportion of patients diagnosed with ST elevation myocardial infarction was larger (32% v 20%). The proportions of patients who underwent catheterisation (81% v 70%) or percutaneous coronary intervention (49% v 35%) were larger for those who presented to catheterisation‐capable hospitals. The baseline characteristics of patients who underwent catheterisation were similar for both presentation hospital categories, as were rates of major adverse cardiovascular events and all‐cause death in hospital and by 6‐ and 12‐ or 24‐month follow‐up.
Conclusions: Although a larger proportion of patients who presented to catheterisation‐capable hospitals underwent catheterisation, patients with similar characteristics were selected for the procedure, independent of the hospital of presentation. Major outcomes for patients were also similar, suggesting equitable management of patients with ACS across Australia.