We celebrate another exciting year and wish our readers a restful break and a prosperous 2020
Welcome to our 2019 Christmas issue, in which we celebrate the MJA year in review together with the traditional holiday season Down Under. As many of our readers and authors across Australia commence their well deserved breaks, we hope this more light‐hearted issue of the MJA will still inform, inspire — and amuse.
Santa epidemics, a new syndrome (MiSeRY), Sherlock Holmes, miracles, recycling, call bells, and blondes all share the limelight
We received 23 submissions for our Christmas competition this year, and it was even harder than usual to select the best for publication. What if Santa came down with measles on Christmas Eve (presumably having missed being vaccinated at the North Pole)? What would be the risk to all the children and households around the world? Perish the thought experiment!1 A new syndrome is also described in this issue: ManuScript Rejection sYndrome or MiSeRY, a grief reaction almost everyone who has written a medical paper has experienced at some point, including your editor‐in‐chief (often).2 Doctors are trained to be expert diagnostic detectives, and although more than 100 years have passed since his first story was published, Sherlock Holmes remains an inspiring figure, as discussed in this issue.3 You will also read about a medical miracle in Bethlehem associated with the birth of Jesus.4 In this age of disposable everything, to the detriment of the environment, I appreciated the article on re‐purposing medical equipment; who would have thought that so many devices could assist with our national coffee‐making obsession?5 You will learn that the symbols on patient call bells in hospitals across the globe may (or should) inspire a new revolution.6 And you will find out whether blondes really do have more fun, as Rod Stewart proposed in a famous and popular song — and you may be surprised.7 We hope you will enjoy this eclectic selection of witty and often amusing contributions to our competition, and we congratulate this year's winners, Hui‐Chen Han, Anoop Ninan Koshy, and colleagues2 for their exploration of factors that influence the MiSeRY of rejected authors!
A great year for our Journal
It has been a very exciting year for the MJA. First, our quality, impact, and ranking have risen thanks to the increasing excellence of the submissions we receive.8 The MJA now proudly ranks among the top 10% of general medical journals globally (16th of 160 journals; source: Journal Citation reports, Clarivate, 2019). Second, the MJA has secured the next annual meeting of the Asia Pacific Association of Medical Editors (APAME) for Australia, to be held in Manly on 10–12 September 2020. We invite authors, clinicians, peer reviewers, researchers, academics, medical students, PhD candidates, and aspiring editors from all health and science fields to participate in what will be an outstanding program; further details will be shared early in the new year. Third, the first online MJA flipbook is currently being tested by 500 subscribers; if successful, this innovation will greatly enhance the online reading experience for all MJA subscribers. Fourth, we continue to increase our national and international presence and relevance. For example, we have continued our successful partnership with the Lancet that commenced in 20189 with the 2019 follow‐up of the MJA–Lancet Countdown on health and climate change in this issue (a print summary and the full report online).10 Fifth, we are working to broaden the dissemination of MJA content, and are proud that all our research articles are available without cost on the MJA website, as are all articles on Indigenous health. Sixth, we now offer our authors both Green and Gold Open Access options for publishing their articles. Finally, we are actively commissioning new content for 2020, as well as continuing to welcome author submissions from around the world: your ideas, suggestions, feedback, and articles are always welcome.
MJA impact is on the rise
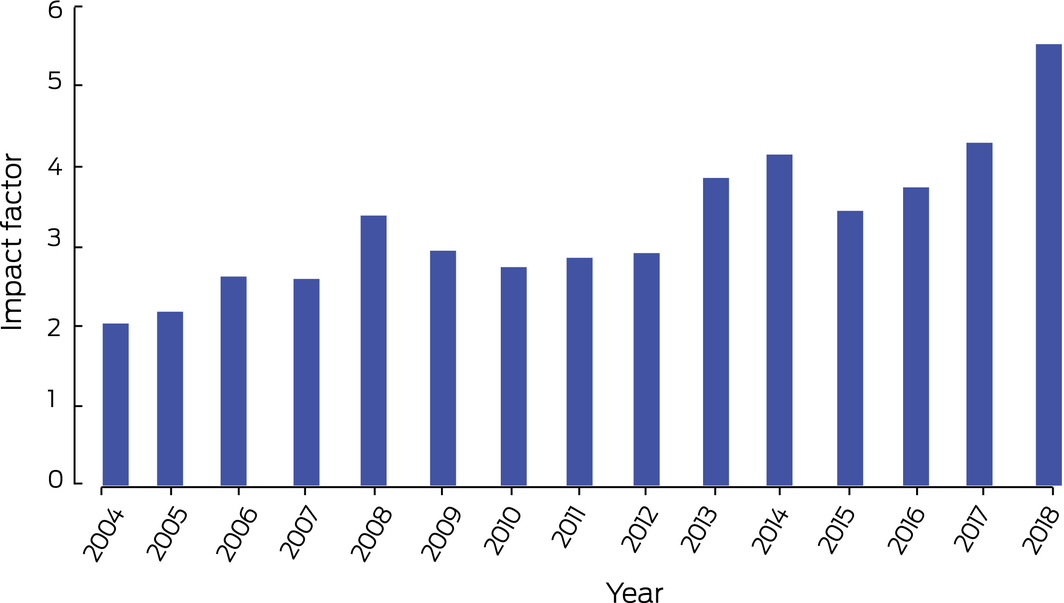
The MJA is a high impact medical journal read around the world; more than 3.4 million mja.com.au page views, from almost all countries, were counted for January–October 2019. Our articles attract strong mainstream media attention, and this translates into research impact for authors. Like all top journals, we currently reject a high proportion of submitted original research articles (92% during 2019; Box 1), indicating the high quality of the work we publish. We continue to strive to increase our decision speed, and the average time from submission to first decision for original research is now 26 days. The impact factor of the MJA continues to rise, and is now the highest it has ever been (Box 2).
Authors and readers can be confident that each MJA article has undergone rigorous editorial review, including specific statistical and methodologic review of research articles, as well as double blind peer review. Reviewers do not determine whether a manuscript is accepted or rejected, but their input as content experts is essential for identifying design problems and other flaws, and for helping guide the Editorial team to fair decisions. We extend our deep thanks to all our outstanding peer reviewers who have selflessly contributed to the rigour of our Journal and to the quality of Australian medical research (pages 487‐489).
Articles short‐listed for the MJA, MDA National Prize for Excellence in Medical Research
Selecting the top original research papers we have published during the past year is always a highlight for the editors. All articles published in the MJA have reached a very high standard, but for the prestigious MJA, MDA Prize for Excellence in Medical Research we have a two‐stage process: the Editorial team rank and shortlist the twelve best papers, which are then independently reviewed by an expert panel of MJA External Advisory Group members who choose the winner of the annual prize (worth $10 000). We congratulate the authors of the short‐listed articles, the key findings of which are summarised below (in no particular order). Please note the breadth and depth of the papers under consideration for the 2019 prize, to be presented to the winner at the annual meeting of the Australian Medical Association in May 2020:
- Clinicians need reliable tools for identifying people at risk of cardiovascular events. Albarqouni and his colleagues11 calculated predicted 10‐year cardiovascular disease risk for each participant in the Australian Diabetes, Obesity and Lifestyle (AusDiab) study with four existing cardiovascular disease risk prediction models. In terms of discrimination, calibration and clinical utility, the 2013 Pooled Cohort Risk Equation model and the 1991 Framingham risk model were superior to two 2008 Framingham cardiovascular disease risk models, both in men and women, and therefore deemed appropriate for estimating cardiovascular disease risk in Australia.
- Rapid access chest pain clinics (RACPCs) are common in the United Kingdom, and this model of care could improve care for patients with chest pain in Australia. In a prospective cohort study with a historical control group, Black and his colleagues12 found that median review times and the number of clinic reviews required for a diagnosis were lower for patients attending an Australian RACPC than a general cardiology clinic in the same hospital, as were rates of emergency department re‐attendance and adverse events at 30 days and 12 months. Assessing people with new onset chest pain in RACPCs may have significant benefits for Australian hospitals.
- To maximise recovery of function and independence, people who have had strokes need best practice stroke unit care as early as possible. Lynch and her colleagues13 report that one in ten people admitted to hospital after a stroke were not offered goal‐directed rehabilitation during their acute admission, without an evidence‐based reason being recorded for this decision. Not providing optimal acute and post‐acute care rehabilitation is of major concern, as it may reduce the independence of patients and increase the burdens on their carers, their community, and aged care services.
- In their cross‐sectional review of Victorian Cancer Registry data, De Menezes and her co‐authors14 assessed changes over time in the choice of skin biopsy technique for diagnosing invasive melanoma. They found that the proportion of partial biopsies had increased from 20% in 2005 to 36% in 2015, and the proportion of shave biopsies from 9% to 20%, the technique being increasingly popular among both dermatologists and general practitioners. As the high base transection rate with shave biopsy (54%) reduces the accuracy of tumour staging crucial for planning appropriate therapy, the authors concluded that excisional biopsy should be the standard of care for lesions suspected to be invasive melanoma, in keeping with Cancer Council Australia guidelines.
- Machalek and her colleagues15 reported early data from the renewed cervical screening program in their retrospective review of 195 606 specimens that were submitted for HPV testing in Sydney. During six months of 2017–18, cytogenic abnormalities were identified in specimens from 35.5% of women with positive oncogenic human papillomavirus virus (HPV) screening test results; high grade abnormalities were detected in 15.3% of samples positive for HPV types 16/18. These data are reassuring, as they confirm the renewed screening program is performing as expected.
- Organs are often rejected for transplantation if potential donors are at increased risk of blood‐borne virus infections, including men who have sex with men, injecting drug users, sex workers, and prisoners. Waller and her colleagues16 undertook a rigorous systematic review and meta‐analysis to estimate the residual risk in Australia of infection with human immunodeficiency virus (HIV) or hepatitis C (HCV) or B viruses (HBV) by organ donors from groups at increased risk who have negative viral test results. They found that the absolute residual risks of infection were very low, and that judicious acceptance of organs from such donors could reduce transplant waitlist mortality by providing organs for as many as 30 additional recipients each year in NSW alone.
- The Getting it Right Collaborative Group17 undertook an important validation study of a culturally adapted version of the nine‐item Patient Health Questionnaire (aPHQ‐9) as a screening tool for depression in Indigenous Australians. In their prospective observational study including 500 Indigenous Australians from ten primary health care centres, they found that the aPHQ‐9 is an effective tool for screening for current major depressive episodes, and could help clinicians and researchers confidently identify depression in Indigenous patients, facilitating initiation of effective treatment.
- The dearth of dedicated clinical mental health support and intervention services in remote Australia can dissuade people from seeking help until they are in crisis. In an original prospective study during 2014–2017, Gardiner and his colleagues18 found that the Royal Flying Doctor Service transported 2257 people from rural and remote locations to larger towns and cities for the treatment of mental and behavioural disorders, the major diagnoses of patients including schizophrenia, bipolar affective disorder, depression, and, particularly among younger patients, substance misuse disorders.
- The most frequently implicated drug in fatal overdoses in Australia is paracetamol (acetaminophen). Cairns and her colleagues19 retrospectively reviewed paracetamol overdose‐related hospital admissions and deaths in Australia and the overdose sizes of intentional paracetamol overdoses, as reflected in data from several national databases. Paracetamol poisoning diagnoses increased by 3.8% per year between 2007–08 and 2016–17; overdose sizes also increased, and overdoses with modified release paracetamol preparations became more common. The findings suggest that availability should be restricted by, for example, reducing pack sizes for non‐prescription paracetamol.
- The increasing misuse of the anticonvulsant pregabalin, widely used for treating neuropathic pain, is associated with adverse psychiatric and medical effects. In their retrospective cross‐sectional study, Crossin and her colleagues20 found that the rate of pregabalin‐related ambulance attendances increased tenfold in Australia between 2012 and 2017, and that the rise was correlated with the national prescription rate. Patients frequently misused pregabalin together with other sedatives, particularly benzodiazepines, and almost 40% of misuse‐related events requiring paramedic attendance were suicide attempts. Caution is required when prescribing pregabalin, especially for patients using other sedatives.
- In a cluster randomised controlled trial in 18 NSW hospitals, Cheung and his colleagues21 examined whether screening emergency department patients improves the detection of unrecognised diabetes. The investigators found that automatically requesting HbA1c assessments of patients with blood glucose levels of 14 mmol/L or more and notifying hospital diabetes services were insufficient for improving care, and needed to be supported by more comprehensive, systems‐based solutions.
- In an open label randomised controlled trial in a tertiary maternity hospital, White and his co‐authors22 found that circulating Rh(D)‐immunoglobulin (anti‐D) was detectable at delivery in a greater proportion of Rh(D)‐negative women who had received antenatal anti‐D prophylaxis as two doses (at 28–30 and 34–36 weeks of pregnancy: 111 of 129, 86%) than of women who received it as a single dose (28–30 weeks: 70 of 125, 56%). The authors concluded that the two‐dose schedule, recommended in Australia, provides better protection against Rh(D) sensitisation than the single dose preferred in some overseas countries.
Stepping up nationally and globally
I have repeatedly stated publicly that Australian health and medical researchers need and deserve an outstanding local general medical journal with national and global perspectives. A great journal does not just publish excellent peer‐reviewed, evidence‐based articles that have been subjected to the highest quality editorial processes; a great journal is much more than a collection of original research papers. In my view, a great journal promotes research excellence, influences medical practice and policy by providing the best evidence, stimulates debate, discussion and further research, is a trusted source of information for the profession, community and government, and helps shape the evolving role of medical practice over time. The MJA will continue to aspire to be a globally leading general medical journal, with the broad objective of improving health outcomes for all Australians. As we journey forward, we thank you and all our readers for your support during 2019, and the entire MJA team sends you and your families our season's greetings, and best wishes for a great 2020.
Box 1 – Manuscripts received and accepted by the MJA, 1 July 2018 – 30 June 2019, by type; number of peer reviewers, 2018–2019; and Journal Impact Factor (Clarivate), 2018
|
Manuscripts |
Received |
Accepted |
Proportion accepted |
||||||||||||
|
|
|||||||||||||||
|
All manuscripts |
1222 |
341 |
28% |
||||||||||||
|
Research articles |
481 |
38 |
8% |
||||||||||||
|
Research letters |
56 |
15 |
27% |
||||||||||||
|
Narrative reviews/meta‐analyses |
94 |
21 |
22% |
||||||||||||
|
Guidelines/Guideline summaries |
12 |
5 |
42% |
||||||||||||
|
Editorials |
43 |
41 |
95% |
||||||||||||
|
Lessons from practice/Snapshots |
492 |
29 |
6% |
||||||||||||
|
Perspectives |
226 |
62 |
27% |
||||||||||||
|
Letters to the Editor |
113 |
87 |
77% |
||||||||||||
|
Peer reviewers (31 October 2018 – 1 November 2019) |
|
809 |
|
||||||||||||
|
Journal Impact Factor, 2018* |
|
5.44 (2017: 4.23) |
|
||||||||||||
|
|
|||||||||||||||
|
* Source: Journal Citation reports, Clarivate, October 2019. |
|||||||||||||||
- 1. Furuse Y. What would happen if Santa Claus is sick? His impact on communicable disease transmission. Med J Aust 2019; 211: 523–524.
- 2. Han H‐C, Koshy AN, Lin T, et al. Predictors of ManuScript Rejection sYndrome (MiSeRY): a cohort study. Med J Aust 2019; 211: 511–513.
- 3. Kampmann JD. Medical references and curiosities in the Sherlock Holmes stories. Med J Aust 2019; 211: 525–527.
- 4. Rajagopalan A, Rajagopalan E. Standards of obstetric care in first century Bethlehem. Med J Aust 2019; 211: 518.
- 5. Massie RJH. Repurposing medical equipment. Med J Aust 2019; 211: 527–528.
- 6. Chapman LRE, Mellow S. Symbolic sexism: superficial or serious bias? An investigation into images on patient call bells. Med J Aust 2019; 211: 514–517.
- 7. Zetner D, Ryg J, Andresen K, et al. Blondes do not have more fun: a non‐blinded crossover field study. Med J Aust 2019; 211: 519–522.
- 8. Foley PB, Gee CE, Talley NJ. The MJA in 2019: a long tradition and increasingly high and broad impact. Med J Aust 2019; 211: 101–102. https://www.mja.com.au/journal/2019/211/3/mja-2019-long-tradition-and-increasingly-high-and-broad-impact
- 9. Zhang Y, Beggs PJ. The 2019 report of the MJA‐Lancet Countdown on health and climate change: a turbulent year with mixed progress. Med J Aust 2019; 211: 490–491.
- 10. Zhang Y, Beggs PJ, Bambrick H, et al. The MJA–Lancet Countdown on health and climate change: Australian policy inaction threatens lives. Med J Aust 2018; 209: 474. https://www.mja.com.au/journal/2018/209/11/mja-lancet-countdown-health-and-climate-change-australian-policy-inaction
- 11. Albarqouni L, Doust JA, Magliano D, et al. External validation and comparison of four cardiovascular risk prediction models with data from the Australian Diabetes, Obesity and Lifestyle study. Med J Aust 2019; 210: 161–167. https://www.mja.com.au/journal/2019/210/4/external-validation-and-comparison-four-cardiovascular-risk-prediction-models
- 12. Black JA, Cheng K, Flood JA, et al. Evaluating the benefits of a rapid access chest pain clinic in Australia. Med J Aust 2019; 210: 321–325. https://www.mja.com.au/journal/2019/210/7/evaluating-benefits-rapid-access-chest-pain-clinic-australia
- 13. Lynch EA, Mackintosh S, Luker JA, Hillier SL. Access to rehabilitation for patients with stroke in Australia. Med J Aust 2019; 210: 21–26. https://www.mja.com.au/journal/2019/210/1/access-rehabilitation-patients-stroke-australia
- 14. de Menezes SL, Kelly JW, Wolfe R, et al. The increasing use of shave biopsy for diagnosing invasive melanoma in Australia. Med J Aust 2019; 211: 213–218. https://www.mja.com.au/journal/2019/211/5/increasing-use-shave-biopsy-diagnosing-invasive-melanoma-australia
- 15. Machalek DA, Roberts JM, Garland SM, et al. Routine cervical screening by primary HPV testing: early findings in the renewed National Cervical Screening Program. Med J Aust 2019; 211: 113–119. https://www.mja.com.au/journal/2019/211/3/routine-cervical-screening-primary-hpv-testing-early-findings-renewed-national
- 16. Waller KMJ, De La Mata NL, Kelly PJ, et al. Residual risk of infection with blood‐borne viruses in potential organ donors at increased risk of infection: systematic review and meta‐analysis. Med J Aust 2019; 211: 414–420. https://www.mja.com.au/journal/2019/211/9/residual-risk-infection-blood-borne-viruses-potential-organ-donors-increased
- 17. The Getting it Right Collaborative Group. Getting it Right: validating a culturally specific screening tool for depression (aPHQ‐9) in Aboriginal and Torres Strait Islander Australians. Med J Aust 2019; 211: 24–30. https://www.mja.com.au/journal/2019/211/1/getting-it-right-validating-culturally-specific-screening-tool-depression-aphq-9
- 18. Gardiner FW, Coleman M, Teoh N, et al. Aeromedical retrievals of people for mental health care and the low level of clinical support in rural and remote Australia. Med J Aust 2019; 211: 351–356. https://www.mja.com.au/journal/2019/211/8/aeromedical-retrievals-people-mental-health-care-and-low-level-clinical-support
- 19. Cairns R, Brown JA, Wylie CE, et al. Paracetamol poisoning‐related hospital admissions and deaths in Australia, 2004–2017. Med J Aust 2019; 211: 218–223. https://www.mja.com.au/journal/2019/211/5/paracetamol-poisoning-related-hospital-admissions-and-deaths-australia-2004-2017
- 20. Crossin R, Scott D, Arunogiri S, et al. Pregabalin misuse‐related ambulance attendances in Victoria, 2012–2017: characteristics of patients and attendances. Med J Aust 2019; 210: 75–79. https://www.mja.com.au/journal/2019/210/2/pregabalin-misuse-related-ambulance-attendances-victoria-2012-2017
- 21. Cheung NW, Campbell LV, Fulcher GR, et al. Routine glucose assessment in the emergency department for detecting unrecognised diabetes: a cluster randomised trial. Med J Aust 2019; 211: 454–459. https://www.mja.com.au/journal/2019/211/10/routine-glucose-assessment-emergency-department-detecting-unrecognised-diabetes
- 22. White SW, Cheng JC, Penova‐Veselinovic B, et al. Single dose v two‐dose antenatal anti‐D prophylaxis: a randomised controlled trial. Med J Aust 2019; 211: 261–265. https://www.mja.com.au/journal/2019/211/6/single-dose-v-two-dose-antenatal-anti-d-prophylaxis-randomised-controlled-trial





I would like to thank the tireless efforts of the Editorial team throughout 2019, without which the quality and timely publication of our Journal in print and online would not be possible: our Head of Publishing Content, Lilia Kanna; Senior Deputy Medical Editor, Christine Gee; Deputy Medical Editors, Francis Geronimo, Robyn Godding, Tania Janusic, Selina Lo, Wendy Morgan, and Zoë Silverstone; our Structural and Scientific Editors, Graeme Prince, Paul Foley, and Laura Teruel; our Consultant Biostatistician, Elmer Villanueva; our News and Online Editor, Cate Swannell; our Graphic Designer, Leilani Widya; and our Senior Publishing Coordinator, Kerrie Harding.
No relevant disclosures for this article. A complete list of my conflict of interest disclosures is found at https://www.mja.com.au/journal/staff/