The known Australian studies have identified adverse respiratory effects in children of indoor environmental exposures, but their contribution to the national asthma burden has not been quantified.
The new Exposure of Australian children to damp housing and gas stove emissions is common, and is respectively associated with 7.9% and 12.3% of the total asthma burden in children aged 14 years or under.
The implications A coordinated national strategy is needed to increase awareness of indoor environmental exposures in the context of asthma prevention, and of interventions for reducing exposure to gas stove emissions and dampness.
The prevalence of asthma in Australia is among the highest in the world; 10% of the population has current asthma,1 and it is the leading contributor to disease burden in Australian children aged 14 years or less.1 Children spend 60–75% of their time indoors at home, which can expose them to several risk factors for asthma,2 including damp housing and gas stove emissions. Although several Australian studies have reported negative associations between indoor exposures and respiratory health in children,3-5 there have been no systematic attempts to quantify their contribution to the national childhood asthma burden.
In this study, we sought to estimate this contribution, with the aims of informing clinicians about the magnitude of the burden and equipping policy makers with recommendations for improving population health.
Methods
We selected damp housing and gas stoves as the two indoor residential exposures to investigate because exposure to gas stoves has been associated with childhood asthma, and damp housing has been causally linked with childhood asthma. Both are common in Australia, and are amenable to interventions for reducing exposure.6,7 Although gas heaters are also common in many parts of Australia and have been associated with respiratory irritation and asthma symptoms,8,9 we did not include them in our analysis because our preliminary search found no recent meta-analyses of their association with childhood asthma.
We applied a comparative risk assessment approach,10 which requires data on the proportion of the population exposed, effect estimates for asthma among those exposed, and the total asthma burden in children aged 14 years or under expressed as disability-adjusted life years (DALYs). We selected 2011 as our reference year because it was the year with the greatest overlap of input data.
Dampness definition and exposure estimation
We defined dampness as the presence of visible mould in a dwelling (apart from the bathroom) and assumed, as have similar studies, that visible mould was entirely attributable to excessive dampness.11 As there are no national estimates of household dampness in Australia, we searched PubMed, Web of Science, Scopus, and Google Scholar for peer-reviewed studies reporting the prevalence of dampness in Australian homes (online Appendix). The nine studies we identified, undertaken in four of six Australian states and published during 1998–2014, included a total of 7538 homes. We weighted the results from each study by the number of homes sampled and the 2011 census population of the greater metropolitan area of the city in which the studies were performed to estimate the proportion of children exposed to dampness at home.
Gas stove definition and exposure estimation
We defined gas stove exposure as the presence of a gas stove in the home. To estimate the proportion of children exposed to gas stoves, we used data from the 2011 Energy Use and Conservation Survey of the Australian Bureau of Statistics, which collected information on the main energy source used for stoves, including piped natural gas (ie, mains gas).12 These data were employed because of the large sample size of the survey (12 841 households), its national coverage, and the well documented quality assurance information on sampling error.12 We focused on piped gas stoves as a proxy measure of exposure to gas combustion products because they are more common than piped gas ovens. We did not include homes using liquid petroleum gas cylinders for stovetop cooking (fewer than 10% of all homes12) because detailed data were not available. The Energy Use survey did not collect data on range hoods, which can reduce exposure to gas combustion products. We therefore performed an additional analysis that assessed their effect, based on data from a recent experimental study which found that about 75% of gas and particle emissions are captured by high flow range hoods.13
Effect estimates for dampness and gas stoves
We used pooled effect estimates from recent meta-analyses, rather than individual studies, to quantify associations between the exposures of interest and asthma to ensure the robustness and generalisability of associations. We searched PubMed for peer-reviewed meta-analyses published in the past 5 years (ie, since 2011) of the association between household dampness or gas stoves and asthma in children (online Appendix). We sought meta-analyses that reported pooled effect estimates and confidence intervals from studies identified by a systematic search, assessed associations with prevalent or incident asthma, reported fixed and random effect estimates (odds ratios or relative risks) adjusted for confounders, and assessed publication bias. While we were interested in cross-sectional (effects on prevalent asthma) and longitudinal associations (effects on incident asthma), we favoured meta-analyses of incident asthma when available.
Asthma burden
The 2011 national census counted 4 144 024 children aged 14 years or under.14 Data from the 2010 Global Burden of Disease (GBD) study (obtained using the GBD results tool: http://ghdx.healthdata.org/gbd-results-tool) were used to estimate the burden of asthma in this age group in Australia, expressed as a point estimate of DALYs — the sum of years of life lost (YLLs) and years lived with disability (YLDs) because of asthma — with 95% uncertainty intervals, without discounting or weighting for age. The data sources and methods for quantifying the burden of asthma in Australia have been described in detail elsewhere.15 The GBD data were used because the study applied a well documented, systematic methodology that exhaustively identified input data.15
Estimating the contribution of dampness and gas stoves to childhood asthma
We estimated the population attributable fraction (PAF) and the asthma burden (DALYs) associated with each indoor risk factor. The PAF is the theoretical proportion of asthma burden that could be averted were the risk factor removed. Because estimating the PAF can introduce uncertainty at each step, particularly if point estimates are used, our approach was to incorporate all available data on the spread and precision of the variables used to calculate PAF and the burden for each risk factor. However, summary statistics rather than raw data for exposure, effect size, and disease burden variables were available for our analysis; we therefore used these descriptive statistics to generate normal distributions for each variable, from which we randomly drew 10 000 values. Our calculations began with a randomly selected value from the distribution of the proportion of children exposed, which was then combined with a randomly selected value from the distribution of the effect estimate to calculate an estimate of the PAF for each risk factor:10
where p = proportion of children exposed to the risk factor; RR = relative risk (or odds ratio) of asthma for children exposed to the risk factor.16 The PAF estimate was multiplied by a randomly selected value from the asthma burden distribution to calculate the estimated disease burden in DALYs:10

where BoDTOTAL = the total burden of asthma among children, and BoDINDOOR = burden attributable to the risk factor. This calculation was repeated 10 000 times, generating PAF and disease burden distributions with 10 000 values each, from which we derived the mean values and 95% confidence intervals (CIs). We explored alternative distribution shapes and the sensitivity to the number of iterations before settling on these parameters. All analyses were conducted in R 3.2.2 (R Foundation for Statistical Computing).
Sensitivity analyses
We undertook additional analyses to assess the sensitivity of our PAF results to plausible changes in input parameters: the proportion of children exposed (including and excluding certain studies used to estimate dampness; assessing the effects of range hoods on gas stove exposure), effects (using different effect estimates reported by the meta-analyses), and changing the age range for childhood to include those aged 19 years or under when calculating asthma-associated DALYs.
Ethics approval
Our modelling study was based on exposure prevalence and effect estimates identified in literature searches and publicly available, aggregated estimates of national asthma burden. Further, national data were drawn from Australian Bureau of Statistics surveys collected under the Census and Statistics Act 1905 (Cwlth). Formal ethics approval for our investigation was therefore not required.
Results
We estimated that the population-weighted prevalence of dampness in Australian homes is 26.1% (standard deviation, 9.4%), based on data in the identified studies for a total of 7538 dwellings (online Appendix). There was substantial variation between states in the proportions of households using natural gas for stovetop cooking, ranging from 2% in Tasmania to 56% in Western Australia and 67% in Victoria.12 Overall, 38.2% of Australian households used piped natural gas for stovetop cooking.12
Three meta-analyses that examined the association between exposure to dampness and asthma met our inclusion criteria.7,17,18 We selected the analysis by Quansah and colleagues7 for our study because it was the most recent (2012), included studies from a wide geographic range of locations, and focused on new asthma diagnoses in cohort and incident case–control studies. The single eligible meta-analysis that examined gas stove exposure and asthma6 was based primarily on cross-sectional studies and cross-sectional analyses within cohort studies (38 of 41 included studies).
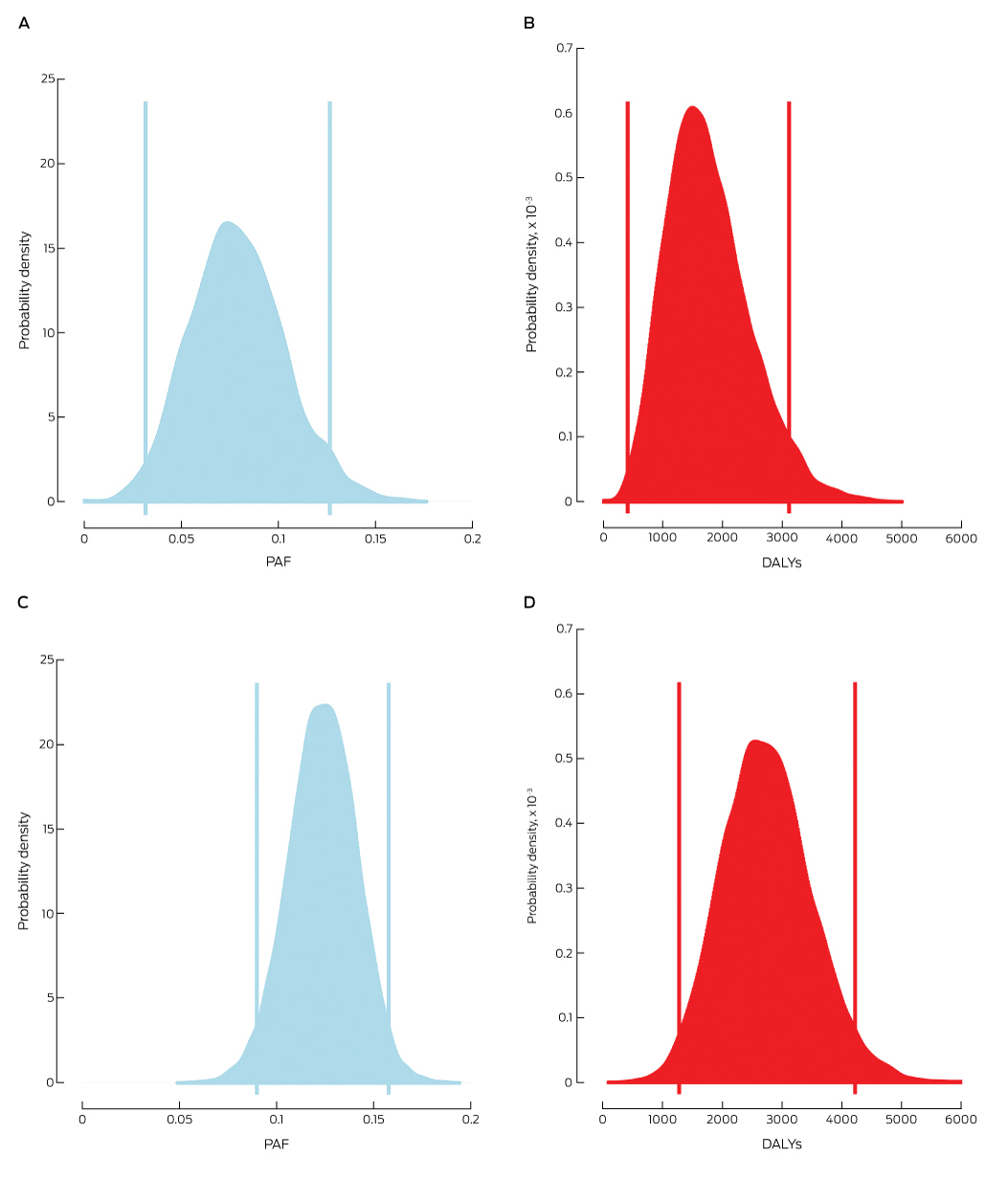
We estimated that the PAF for childhood asthma associated with damp housing was 7.9% (95% CI, 3.2–12.6%; Box, A), causing 1760 DALYs (95% CI, 416–3104 DALYs; Box, B), or 42 DALYs per 100 000 children aged 14 years or younger. The results were robust to changing values of the input parameters (online Appendix, table 1).
Our PAF estimate for childhood asthma associated with gas stoves was 12.3% (95% CI, 8.9–15.8%; Box, C), corresponding to 2756 DALYs (95% CI, 1271–4242; Box, D), or 67 DALYs per 100 000 children aged 14 years or less. These estimates did not change markedly when then input parameters changed (online Appendix, table 2). Our most conservative scenario for the effects of range hoods assumed that all gas stoves were vented outdoors with 75% efficiency (ie, reduced exposure to combustion products by 75%). Our PAF and burden estimates for exposure to gas stoves in this scenario were 3.4% (95% CI, 2.2–4.6%) and 761 DALYs (95% CI, 322–1199).
Discussion
We estimated that damp housing and gas stoves respectively account for 7.9% and 12.3% of the childhood asthma burden in Australia. Although the risks at the level of the individual are relatively small, the proportion of the population exposed is relatively large, so that the contribution to the population asthma burden is considerable.
Exposure of Australian children aged 15 years or younger to indoor second-hand smoke declined from 31.3% in 1995 to 3.7% in 2013.19 This improvement is impressive, but our results suggest that the respiratory health of children is still affected by common but less easily recognised indoor risk factors. Dampness in housing promotes the proliferation of fungi, bacteria and dust mites, and their metabolites and spores have inflammatory, cytotoxic, and immunosuppressive effects.20,21 Gas combustion causes the emission of nitrogen dioxide, formaldehyde, nitrous acid, and ultrafine particles (under 100 nm diameter), and is associated with airway inflammation.22
We estimated that 26.1% of Australian homes have dampness problems, consistent with findings by studies in the United States, Canada and Europe, where at least 20% of homes had indications of dampness.20 Eliminating dampness in dwellings would avert almost 8% of the childhood asthma burden, but the extent to which this is practicable is unclear. Indoor dampness occurs when moisture-sensitive materials, such as plasterboard, are not adequately protected from water, or indoor humidity is excessive.20,21 Parts of most homes are transiently damp, but problems arise when dampness is persistent and supports continuous microbial growth in and near living areas. Controlling dampness requires a multifaceted approach that includes minimising the exposure of interior walls to water and nutrients, as well as using mould-resistant building products and installing vapour barriers in new buildings.20,21 Dampness in existing building stock is more challenging, but all homes can benefit from increasing natural ventilation (eg, open windows), avoiding drying laundry in living areas, and using dehumidifiers.21 Heavily contaminated dwellings may require professional remediation and repair.20
The prevalence of gas cooking in Australia was relatively low compared with that of many western European countries (mean, 63%).23 While our results suggest that 12.3% of the childhood asthma burden could be averted were gas replaced by a different energy source for cooking, this assumes that the new energy source would not produce indoor emissions; this is unlikely, as cooking itself can be a major source of emissions.13 More important is our finding that the burden of asthma associated with gas stoves could be reduced from 12.3% to 3.4% were all homes with gas stoves fitted with high efficiency range hoods that vented outdoors. Particles and gases can be captured with greater than 75% efficiency by such hoods, while lower flow rates and recirculating range hoods offer less protection.13 Range hoods also remove cooking-related water vapour, reducing indoor dampness. However, 44% of people in Melbourne with range hoods reported that they did not use them regularly,24 indicating that their potential health benefits should be communicated to the Australian public. We acknowledge that fitting all homes with range hoods would be impractical, but improving natural ventilation in all homes should be recommended to reduce exposure to gas combustion products.
Public education with the aim of reducing the burden of asthma should include information about how indoor exposures can affect health and how to recognise problem areas, as well as offering a range of suggestions for reducing exposure, from the simple and inexpensive to more complex and expensive but more effective options. Relevant information is disseminated by the New South Wales Ministry of Health25 and other state health departments as general factsheets; these should be reviewed to ensure that they are up to date and easily accessible. Given the degree of exposure to dampness and gas stoves in Australia, a national approach in the context of asthma prevention is required.
Like most modelling studies, the main limitation of our investigation is the validity of the input data. We used standard methods, were selective in what we included, and performed sensitivity analyses, but we may have under- or overestimated the burden of asthma attributable to each risk factor. Further, we assessed children to 14 years of age as a single group with respect to the effects of indoor exposures on asthma. Asthma in younger children, however, may be exacerbated to a greater extent than in older children by other factors, such as respiratory infections. A more comprehensive investigation could examine further indoor risk factors and assess the feasibility of intervention-based studies for reducing the asthma burden. Clinicians treating children should be aware of the potential significance of indoor exposures for children with or at increased risk of asthma.
Received 16 May 2017, accepted 21 September 2017
- Luke D Knibbs1
- Solomon Woldeyohannes1
- Guy B Marks2,3
- Christine T Cowie4
- 1 University of Queensland, Brisbane, QLD
- 2 Woolcock Institute of Medical Research, Sydney, NSW
- 3 Liverpool Hospital, Sydney, NSW
- 4 South Western Sydney Clinical School, University of New South Wales, Sydney, NSW
This work was supported by the National Health and Medical Research Council (Luke Knibbs: Early Career Fellowship [APP1036620]; Guy Marks: Centres of Research Excellence grant [APP1030259]), the Centre for Air Quality and Health Research and Evaluation (Luke Knibbs, Christine Cowie: postdoctoral fellowships), and the New South Wales Ministry of Health (funding to Christine Cowie and Guy Marks).
No relevant disclosures.
- 1. Australian Centre for Asthma Monitoring. Asthma in Australia 2011: with a focus chapter on chronic obstructive pulmonary disease (AIHW Cat. No. ACM 22; Asthma Series no. 4). Canberra: Australian Institute of Health and Welfare, 2011. https://www.aihw.gov.au/reports/asthma-other-chronic-respiratory-conditions/asthma-in-australia-2011-with-chapter-on-copd/contents/table-of-contents (viewed Apr 2017).
- 2. Institute of Medicine. Climate change, the indoor environment, and health. Washington (DC): The National Academies Press, 2011. https://www.nap.edu/catalog/13115/climate-change-the-indoor-environment-and-health (viewed Apr 2017).
- 3. Garrett MH, Hooper MA, Hooper BM, Abramson MJ. Respiratory symptoms in children and indoor exposure to nitrogen dioxide and gas stoves. Am J Resp Crit Care Med 1998; 158: 891-895.
- 4. Franklin P, Dingle P, Stick S. Raised exhaled nitric oxide in health children is associated with domestic formaldehyde levels. Am J Resp Crit Care Med 2000; 161: 1747-1749.
- 5. Ponsonby AL, Couper D, Dwyer T, et al. The relation between infant indoor environment and subsequent asthma. Epidemiology 2000; 11: 128-135.
- 6. Lin W, Brunekreef B, Gehring U. Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheeze in children. Int J Epidemiol 2013; 42: 1724-1737.
- 7. Quansah R, Jaakkola MS, Hugg TT, et al. Residential dampness and molds and the risk of developing asthma: a systematic review and meta-analysis. PLoS One 2012; 7: e47526.
- 8. Pilotto LS, Nitschke M, Smith BJ, et al. Randomized controlled trial of unflued gas heater replacement on respiratory health of asthmatic schoolchildren. Int J Epidemiol 2003; 33: 208-214.
- 9. Marks GB, Ezz W, Aust N, et al. Respiratory health effects of exposure to low-NOx unflued gas heaters in the classroom: a double-blind, cluster-randomized, crossover study. Environ Health Perspect 2010; 118: 1476-1482.
- 10. Hänninen O, Knol A (editors). European perspectives on environmental burden of disease: estimates for nine stressors in six European countries. Helsinki: National Institute for Health and Welfare, 2011. https://www.julkari.fi/bitstream/handle/10024/79910/b75f6999-e7c4-4550-a939-3bccb19e41c1.pdf (viewed Apr 2017).
- 11. Fisk WJ, Lei-Gomex Q, Mendell MJ. Meta-analyses of the associations of respiratory health effects with dampness and mould in homes. Indoor Air 2007; 17: 284-296.
- 12. Australian Bureau of Statistics. 4602.0.55.001. Energy use and conservation survey, 2011. Energy use and conservation additional tables (data cube). http://www.abs.gov.au/AUSSTATS/subscriber.nsf/log?openagent&4602055001do002_201103.xls&4602.0.55.001&Data%20Cubes&E32C173D338FE75FCA257953000EE41A&0&Mar%202011&28.11.2011&Previous (viewed Apr 2017).
- 13. Lunden MM, Delp WW, Singer BC. Capture efficiency of cooking-related fine and ultrafine particles by residential exhaust hoods. Indoor Air 2015; 25: 45-58.
- 14. Australian Bureau of Statistics 2013, 2011 Census community profiles. Basic community profile, table B04. http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/communityprofile/0 (viewed Feb 2018).
- 15. Australia Institute of Health and Welfare. Assessment of global burden of disease 2010 methods for the Australian context (Working paper no. 1). Canberra: AIHW, 2014. http://content.webarchive.nla.gov.au/gov/wayback/20170421063605/http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129547710 (viewed Apr 2017).
- 16. Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998; 280: 1690-1691.
- 17. Tischer C, Chen C-M, Heinrich J. Association between domestic mould and mould components, and asthma and allergy in children: a systematic review. Eur Respir J 2011; 38: 812-824.
- 18. Tischer CG, Hohmann C, Thiering E, et al. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy 2011; 66: 1570-1579.
- 19. Australian Institute for Health and Welfare. National drug household survey: detailed report 2013 (AIHW Cat. No. PHE 183; Drug Statistics Series No. 28). http://www.aihw.gov.au/publication-detail/?id=60129549469 (viewed Apr 2017).
- 20. Institute of Medicine. Damp indoor spaces and health. Washington (DC): The National Academies Press, 2004. https://www.nap.edu/catalog/11011/damp-indoor-spaces-and-health (viewed Apr 2017).
- 21. World Health Organization. WHO guidelines for indoor air quality: dampness and mould. Copenhagen: WHO Regional Office for Europe, 2009. http://www.who.int/indoorair/publications/7989289041683/en/ (viewed Apr 2017).
- 22. Heinrich J. Influence of indoor factors in dwellings on the development of childhood asthma. Int J Hyg Environ Health 2011; 214: 1-25.
- 23. Jarvis D, Chinn S, Sterne J, et al. The association of respiratory symptoms and lung function with the use of gas for cooking. Eur Respir J 1998; 11: 651-658.
- 24. Dharmage S, Bailey M, Raven J, et al. Prevalence and residential determinants of fungi within homes in Melbourne, Australia. Clin Exp Allergy 1999; 29: 1481-1489.
- 25. New South Wales Ministry of Health. Environmental health fact sheets [website]. Updated Sept 2017. http://www.health.nsw.gov.au/environment/factsheets/Pages/default.aspx (viewed Sept 2017).





Abstract
Objective: To determine the proportion of the national childhood asthma burden associated with exposure to dampness and gas stoves in Australian homes.
Design: Comparative risk assessment modelling study.
Setting, participants: Australian children aged 14 years or less, 2011.
Main outcome measures: The population attributable fractions (PAFs) and number of disability-adjusted life years (DALYs) for childhood asthma associated with exposure to damp housing and gas stoves.
Results: 26.1% of Australian homes have dampness problems and 38.2% have natural gas as the main energy source for cooktop stoves. The PAF for childhood asthma attributable to damp housing was 7.9% (95% CI, 3.2–12.6%), causing 1760 disability-adjusted life years (DALYs; 95% CI, 416–3104 DALYs), or 42 DALYs/100 000 children. The PAF associated with gas stoves was 12.3% (95% CI, 8.9–15.8%), corresponding to 2756 DALYs (95% CI, 1271–4242), or 67 DALYs/100 000 children. If all homes with gas stoves were fitted with high efficiency range hoods to vent gas combustion products outdoors, the PAF and burden estimates were reduced to 3.4% (95% CI, 2.2–4.6%) and 761 DALYs (95% CI, 322–1199).
Conclusions: Exposure to damp housing and gas stoves is common in Australia, and is associated with a considerable proportion of the childhood asthma burden. Strategies for reducing exposure to indoor dampness and gas combustion products should be communicated to parents of children with or at risk of asthma.