The known The prevalence of chronic disease is rapidly increasing as the Australian population ages. Chronic disease self-management support (CDSMS) programs have been widely implemented here and overseas, but evidence for their effectiveness is limited.
The new A clinician-led CDSMS program including goal setting and the development of individualised care plans improved the self-reported health of older people with multiple chronic conditions to a greater degree than did positive attention and health education. It did not, however, improve any of a range of specific health outcomes.
The implications CDSMS may benefit some older people with multiple chronic conditions to a greater extent than health education and positive attention.
The prevalence of chronic disease in Australia is rapidly increasing as the population ages. Chronic disease self-management support (CDSMS) programs seek to increase patients’ skills and confidence in managing their chronic diseases, and include regular assessment of progress and problems, goal setting, and problem-solving support.1 CDSMS is a key feature of the Chronic Care Model,2 and Australia’s National Chronic Disease Strategy similarly recommends that Australia’s health care system place greater emphasis on self-management.3
Despite support for CDSMS as an important approach to managing chronic disease, evidence for its effectiveness is mixed; systematic reviews of randomised trials have found small positive outcomes for patients with some chronic diseases, and in some contexts but not in others. For example, positive effects for patients with chronic obstructive pulmonary disease have been reported,4 but not for those with moderate to severe chronic obstructive pulmonary disease.5 CDSMS was of limited benefit for people with osteoarthritis.6 CDSMS may achieve clinically important benefits for older people with diabetes mellitus and hypertension, but the program elements responsible for these benefits are not clear.7
Reviewers of the CDSMS trial literature have noted the diversity of the programs (disease-specific, generic, individual, group programs) and the heterogeneous outcomes, as well as widespread problems with the design and reporting of trials.4,5 Problems include high rates of attrition, inadequate blinding, and the lack of an appropriate comparator group controlling for the positive benefits of receiving attention from a health professional.6 In addition, trials have often recruited participants from hospital or ambulatory specialist centres, and this limits the generalisability of their findings to the primary care settings in which care for people with chronic diseases is routinely provided.
A further significant limitation of the evidence base is that many trials of CDSMS programs have excluded patients with two or more chronic diseases.8 It is increasingly common, however, for patients to have more than one disorder; in Australia, about one-third of patients seeking care from a general practitioner will have at least two chronic conditions strongly associated with ageing.9 The clinical care of patients with multiple disorders can be challenging, requiring competing priorities to be balanced and collaboration and communication between primary care and several secondary care specialists to be efficient. The evidence base for effective programs in primary care and community settings that recognise the prevalence of multimorbidities and their impact on older patients is limited.10
We therefore compared the outcomes of a generic (not disease-specific), clinician-led CDSMS program for older people with multiple chronic conditions with the outcomes of an attention-based control program. Self-rated health, an important predictor of a range of health outcomes, was the primary outcome measure of our study. Secondary outcome measures included health status (eg, fatigue, pain, health distress), health behaviour (exercise, medication adherence), self-efficacy, and health care utilisation. The perceived usefulness and acceptability of the CDSMS program for participants were also evaluated.
Methods
Study design
We undertook a randomised controlled trial that compared the effectiveness of a CDSMS intervention with outcomes of an attention-based control program. The study protocol has been published in detail elsewhere.11
Setting and participants
The trial was conducted in metropolitan Adelaide, South Australia, between September 2009 and June 2010. Participants were recruited from five general practices. We used electronic medical records to identify patients at least 60 years old who had two or more chronic diseases. Patients received a letter from their GP inviting them to participate. They were informed that the researchers were examining the effectiveness of a program designed to improve the health of people over 60 with chronic illnesses, and that the results would provide useful knowledge about how health professionals could best help people with chronic illnesses. Those interested in participating forwarded their details by phone or email to the study team. Patients were later contacted by a member of the team to arrange a home visit to explain the study, assess eligibility, obtain consent, and administer baseline measures.
Eligibility criteria
People were eligible for the study if they had two or more chronic diseases (cardiovascular, respiratory, musculoskeletal, psychological, digestive, kidney disease, diabetes [type 1 or 2], cancer). Only patients who were ambulatory and spoke English were recruited. Patients were ineligible if they had a terminal illness, a significant cognitive impairment, or severe hearing loss. Patients were also excluded if they rated their health as “very good” or “excellent”, or if they resided in a long term care facility. Participants continued taking routine medications and visiting their usual primary care physician throughout the study.
The CDSMS and positive attention programs
Two interventions were run in parallel: a CDSMS program and an attention (control) program. The treatment program was based on the CDSMS component of the Flinders Chronic Condition Management Program.12 The CDSMS program employs a set of tools (Partners in Health scale, Cue and Response interview, Problems and Goals assessment) and a structured process that enable clinicians and patients to collaboratively assess self-management behaviour, identify problems, set goals, and develop individual care plans that address key self-care, medical, psychosocial, and carer problems. Participants in the control program received health information relevant to their conditions, as well as scheduled contact with our clinicians, who were instructed to provide positive attention. There was no direct contact between our clinical staff and the participants’ GPs or other health care providers (Box 1).
Participants in each program received three home visits and four follow-up phone calls over a 6-month period from a clinician with qualifications in nursing or psychology. The responses and safety of participants were regularly assessed during the trial. Ongoing mentoring from accredited trainers was available to clinicians delivering the CDSMS and control programs. Formal audits of case files ensured that each program was implemented at a high standard.
Randomisation and blinding
Participants were randomly assigned to one of the programs by research staff not involved in delivering either intervention, using computer-generated random numbers. The sequence in which programs were allocated was determined by block design, and randomisation, carried out after the baseline interview, was stratified by sex and marital status. A printed record of the allocation sequence was retained by an independent, centrally located hospital pharmacy. All participants provided written, informed consent for participation; they were blinded to their allocation, but the investigators were not.
Data collection and measures
Participants were assessed at baseline and at 6 months by research staff not involved in delivering either program. All participants were interviewed at the end of their program to assess its perceived usefulness in improving their health. These interviews were also analysed to determine whether the management of their health conditions had changed, and whether the program had affected the relationships of participants with their GPs.
Outcomes were measured with scales provided by the Stanford Patient Education Research Center. The primary outcome measure was self-rated health. Participants were asked to rate their health (“In general, would you say your health is …”) on a five-point Likert scale ranging from poor (1) to excellent (5); this item was originally used by the United States National Health and Nutrition Examination Survey. Self-rated health status has been found to reliably predict future objective health status.13 Secondary outcome measures included health status (including fatigue, pain, health distress, energy, depression, illness intrusiveness), health behaviours (exercise, medication adherence), self-efficacy (confidence that one can achieve desired outcomes), responses to the Health Education Impact Questionnaire (heiQ),14 and health care utilisation (numbers of general practice visits, emergency department visits, and hospital admissions).
Statistical analyses
For the primary outcome, we performed ordinal logistic regression, using the mixed module in Stata 14.1 (StataCorp). For the secondary outcomes we used linear regression models, and Poisson regression models for health utilisation count data.
The analyses were intention-to-treat analyses; that is, all participants were included regardless of whether they completed the study or not. Missing data were imputed according to the baseline-value-carried-forward method. We also undertook three sensitivity analyses of the primary outcome (completed cases only; an alternative imputation method; and an analysis taking into account the reason for data being missing).
All models included the baseline value of the dependent variable, the intervention (CDSMS v control), time as a categorical variable (baseline v 6 months) and an intervention × time interaction. GP and participant were included as random intercepts.
We calculated that enrolling 252 subjects would be required to detect a medium effect size (0.54) on the primary outcome measure of self-rated health.11 Power in the trial was set at 80%, with an attrition rate of 25% and a design effect (caused by GP clustering) of 1.59. All statistical tests were two-sided (a = 0.05); odds ratios for the frequencies of outcomes in the two groups were calculated with 95% confidence intervals (CIs). There was one primary analysis (of self-rated health). P values were not adjusted for multiple testing of secondary outcomes.
Ethics approval
Ethics approval was granted by the Human Research Ethics Committee at Flinders University (reference, 209/09).
Results
Invitation letters were sent to 1663 patients, of whom 634 responded; 541 (33%) were contacted, and 254 (15%) were ultimately enrolled and randomised to treatment. Thirteen participants (10%) did not complete the CDSMS program, ten (8%) the control program; the main reasons for withdrawing were deteriorating health (ten participants) and loss of interest (eight participants). Full outcomes data were available for 231 participants (91% of all randomised participants) (Box 2).
The baseline demographic characteristics and disease profiles of participants in the two programs were similar (Box 3). At baseline, 187 participants (74%) rated their general health as either “poor” or “fair” (Box 4). Almost all participants who completed the study received the allocated number of home visits and phone calls (CDSMS program, 112 of 114; control program, 116 of 117).
Primary and secondary outcomes
At the completion of the 6-month study, the overall distribution of self-rated health scores had improved in the CDSMS group. CDSMS participants were more likely than control group participants to report a better health rating category (odds ratio, 2.50; 95% CI, 1.13–5.50; P = 0.023). Sensitivity analyses applying different methods to the missing outcomes data for 23 participants yielded similar results (Box 4).
For most participants, however, self-rated health was unchanged between baseline and the end of the intervention (CDSMS, 72 of 127 participants [57%]; control, 88 of 127 participants [69%]). Forty-three participants (34%) in the CDSMS program and 24 participants (19%) in the control program reported improved health (ie, at least a one-point change) (Box 5).
None of the estimated between-group differences for the secondary health outcome measures were statistically significant (online Appendix).
Participant feedback
More CDSMS than control participants regarded the program as very or extremely useful (59 of 114 [52%] v 38 of 117 [32%]) and as having changed the management of their health conditions (61% v 33%). Fewer than one-third of participants from each program reported that it had improved their relationship with their GP (CDSMS, 37 of 114 [32%]; control, 28 of 117 [24%]). High proportions of participants in each program would have recommended it to other patients (CDSMS, 90%; control, 85%) (Box 6).
Discussion
In this randomised controlled trial, the proportion of older people with multiple chronic conditions receiving the CDSMS (Flinders) program who reported that their health had improved was higher than that of participants who received a control (positive attention) intervention. The CDSMS program, however, did not improve specific features of health, such as pain, fatigue, depression, illness intrusiveness, and walking for exercise. There was also no effect on health education outcomes measured by the heiQ, reported to be sensitive to changes achieved by self-management programs.15
This pattern of results was unexpected; we had anticipated that overall improvements in the self-rated health of CDSMS program participants would be accompanied by improvements in our more specific measures of health. At a population level, the level of self-rated health (measured by a single item) is correlated with use of health services, changes in functional status, and mortality.16 The meaning of self-rated health at the individual patient level, however, is less clear,17 and the consequences of changes to self-rated health require further study.18
We found that CDSMS participants were significantly more likely than control group participants to report a better health rating category (odds ratio, 2.50), but the 95% CI for this figure was quite wide (1.13–5.50), indicating uncertainty about the average treatment benefit of the CDSMS program, and suggesting that the treatment benefit differed between individuals. Although a greater proportion of CDSMS participants reported improved health, most people in both groups reported unchanged self-rated levels.
CDSMS programs are often designed for people at high risk of unplanned hospitalisation because of their chronic diseases, in the expectation that providing better care in the community can avert some unplanned hospitalisations. Consistent with this approach, our study targeted individuals at higher risk in a two-stage process. First, participants were selected by age and chronic disease status according to electronic general practice patient records, and were personally invited by their GPs. Second, respondents who rated their health as very good or excellent were excluded from the study.
The aim of this two-stage selection process was to identify a group of participants who were at greater risk of poor health outcomes in the future. Self-rated health is commonly employed as a predictor of preventable hospitalisation, and its discriminative capacity is reported to be similar to that of more sophisticated models.19 Our study participants therefore represent a group of primary health care patients who are typically targeted by chronic disease management programs, including the proposed Health Care Homes.20
However, we found no evidence that the level of health service utilisation was different for CDSMS and control participants. In absolute terms, CDSMS participants reported more general practice visits, emergency department visits, and hospital admissions than control group participants, but the differences were not statistically significant. Greater health service utilisation by CDSMS participants was also recently found by a large New South Wales CDSMS evaluation21 and in the Integrated Care pilot studies in the United Kingdom.22
Our study was conducted in the ideal circumstances of a university-based trial focused on achieving high levels of fidelity and very high proportions of participants receiving the intended interventions. We were able to overcome the obstacles that clinicians face in routine service settings when attempting to implement CDSMS programs with high levels of intensity and fidelity.23 Nonetheless, there were several limitations to our study.
The outcome measures were based on patient self-report, and the follow-up period was relatively short (6 months). It is possible that benefits for patients only become apparent over a longer period of time. The two interventions operated independently of GPs and their practice staff; in addition, the CDSMS program did not include case management or coordination elements. Coordination is a component of many chronic disease management programs, and may be particularly important for older people and those with lower health literacy, people who require support for accessing services or engaging in activities included in a care plan. It is possible that a CDSMS program better integrated into routine clinical care and including additional elements could have achieved more.
A key strength of the study was the inclusion of a comparison program that provided supportive listening and tailored health information, minimising the risk of bias in estimating the effect of the CDSMS program. The positive attention group was arguably superior to a usual care comparator group because it allowed blinding the patients to treatment, which is important when outcomes are assessed by the participants.6 The nature of the control group also encouraged participation in the study by general practices.24
In conclusion, our results suggest that a clinician-led CDSMS program including goal setting and individualised care plan development as elements may improve the self-reported health of some older people. We did not, however, detect improvements in more specific health outcomes. A CDSMS program that also includes care coordination and is better integrated with general practice care may achieve better outcomes.
Box 1 – Comparison of the key elements of the chronic disease self-management support (CDSMS) and the positive attention (control) programs
|
|
Attention program (control) |
CDSMS program |
|||||||||||||
|
|
|||||||||||||||
|
Program model |
Semi-structured intervention, providing health information, non-directive counselling and supportive listening |
Structured intervention based on cognitive behavioural therapy and motivational interviewing |
|||||||||||||
|
Role of health professional |
Develop rapport with participant and provide positive attention |
Facilitate goal setting; act as coach and adviser |
|||||||||||||
|
Role of participant |
Passively receive health information; participate in informal conversations |
Active decision making in collaboration with health professional |
|||||||||||||
|
Therapeutic approach |
|
|
|||||||||||||
|
Intervention intensity |
Three home visits and four telephone conversations |
Three home visits and four telephone conversations |
|||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 2 – Flow diagram of patient recruitment, randomisation to the chronic disease self-management support (CDSMS) or control programs, and follow-up
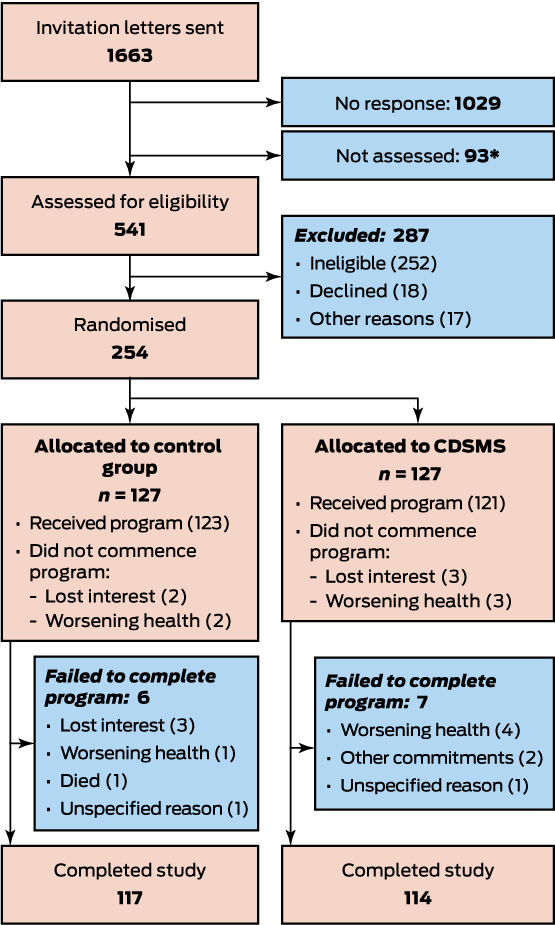
* These eligible patients were not assessed because the target sample size had been reached.
Box 3 – Baseline demographic characteristics and disease profiles of the participants in each program
|
|
Positive attention (control) |
Chronic disease self-management support |
|||||||||||||
|
|
|||||||||||||||
|
Number of patients |
127 |
127 |
|||||||||||||
|
Sex (women) |
77 (61%) |
75 (59%) |
|||||||||||||
|
Age, years |
|
|
|||||||||||||
|
60–75 |
58 (46%) |
61 (48%) |
|||||||||||||
|
76–85 |
51 (40%) |
46 (36%) |
|||||||||||||
|
> 85 |
18 (14%) |
20 (16%) |
|||||||||||||
|
Country of birth |
|
|
|||||||||||||
|
Australia |
97 (76%) |
97 (76%) |
|||||||||||||
|
Ireland or United Kingdom |
17 (13%) |
18 (14%) |
|||||||||||||
|
Europe |
10 (8%) |
11 (9%) |
|||||||||||||
|
Other |
3 (2%) |
1 (1%) |
|||||||||||||
|
Marital status |
|
|
|||||||||||||
|
Married |
80 (63%) |
82 (65%) |
|||||||||||||
|
Separated or divorced |
10 (8%) |
7 (6%) |
|||||||||||||
|
Widowed |
34 (27%) |
35 (28%) |
|||||||||||||
|
Never married |
3 (2%) |
3 (2%) |
|||||||||||||
|
Education |
|
|
|||||||||||||
|
Left school at age 15 or earlier |
62 (49%) |
50 (39%) |
|||||||||||||
|
Left school after age 15 |
65 (51%) |
77 (61%) |
|||||||||||||
|
Work status |
|
|
|||||||||||||
|
Retired from employment |
108 (85%) |
108 (85%) |
|||||||||||||
|
Home duties |
13 (10%) |
11 (9%) |
|||||||||||||
|
Other |
6 (5%) |
8 (6%) |
|||||||||||||
|
Household income |
|
|
|||||||||||||
|
$0–20 000 |
39 (31%) |
36 (29%) |
|||||||||||||
|
$20 001–40 000 |
60 (47%) |
56 (44%) |
|||||||||||||
|
> $40 000 |
21 (17%) |
27 (22%) |
|||||||||||||
|
Missing data |
7 (6%) |
8 (6%) |
|||||||||||||
|
Disease type* |
|
|
|||||||||||||
|
Cardiovascular |
122 (96%) |
119 (94%) |
|||||||||||||
|
Respiratory |
52 (41%) |
46 (36%) |
|||||||||||||
|
Musculoskeletal |
107 (84%) |
108 (85%) |
|||||||||||||
|
Psychological |
49 (39%) |
60 (47%) |
|||||||||||||
|
Digestive |
66 (52%) |
62 (49%) |
|||||||||||||
|
Diabetes |
34 (27%) |
47 (37%) |
|||||||||||||
|
Kidney disease |
15 (12%) |
13 (10%) |
|||||||||||||
|
Cancer |
31 (24%) |
33 (26%) |
|||||||||||||
|
Other |
90 (71%) |
74 (58%) |
|||||||||||||
|
Number of disease types |
|
|
|||||||||||||
|
1–4 |
70 (55%) |
72 (57%) |
|||||||||||||
|
5 or more |
57 (45%) |
55 (43%) |
|||||||||||||
|
Mean number (SD) |
4.5 (0.12) |
4.4 (0.11) |
|||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. * Multiple responses possible. |
|||||||||||||||
Box 4 – Primary outcome: self-rated health at baseline and at end of program (A); likelihood that self-reported health had improved (B)
|
A |
Positive attention (control) |
Chronic disease self-management support (CDSMS) |
|||||||||||||
|
Baseline |
6 months |
Baseline |
6 months |
||||||||||||
|
|
|||||||||||||||
|
Number of patients |
127 |
127 |
127 |
127 |
|||||||||||
|
Self-rated health |
|
|
|
|
|||||||||||
|
Poor |
6 (5%) |
12 (10%) |
14 (11%) |
16 (13%) |
|||||||||||
|
Fair |
89 (70%) |
72 (57%) |
78 (61%) |
50 (39%) |
|||||||||||
|
Good |
32 (25%) |
37 (29%) |
35 (28%) |
48 (38%) |
|||||||||||
|
Very good |
0 |
6 (5%) |
0 |
13 (10%) |
|||||||||||
|
Excellent |
0 |
0 |
0 |
0 |
|||||||||||
|
B |
Odds ratio (95% CI) |
P |
|||||||||||||
|
|
|||||||||||||||
|
Intention-to-treat analysis, CDSMS v control* |
2.50 (1.13–5.50) |
0.023 |
|||||||||||||
|
Sensitivity analyses, CDSMS v control |
|
|
|||||||||||||
|
Expectation–maximisation (EM) mixed model† |
2.92 (1.31–6.51) |
0.009 |
|||||||||||||
|
Reason for drop-out model‡ |
2.23 (1.03–4.83) |
0.041 |
|||||||||||||
|
Completed cases only§ |
2.65 (1.18–5.95) |
0.018 |
|||||||||||||
|
|
|||||||||||||||
|
* For all 254 randomised participants; values for missing self-rated health outcome data (23 participants) were imputed with the baseline-value-carried-forward method. † For all 254 participants; values for missing self-rated health outcome data (23 participants) were calculated from maximum likelihood estimates with an EM algorithm. ‡ For all 254 participants; values for missing self-rated health outcome data (23 participants) were imputed according to reason for dropping out of the study. For ten participants who did not commence their program and seven participants who started but dropped out because of loss of interest (three), other commitments (two) or other reasons (two), the self-rated health base value was carried forward. For five participants who started their programs but dropped out because of declining health, a point was deducted from the self-rated health base value and then used. For one participant who started the program but died, the poorest possible health value (1) was used. § For the 231 participants who provided self-rated health data at both baseline and outcome. |
|||||||||||||||
Box 5 – Change in self-rated health between baseline and end of program, by treatment group*
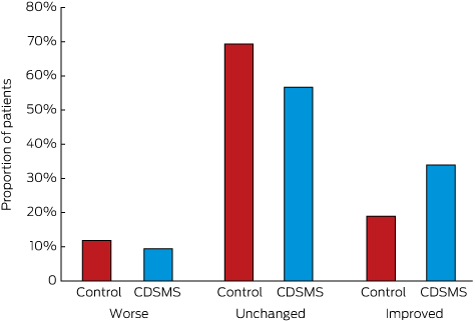
CDSMS = chronic disease self-management support. * Percentages are based on the intention-to-treat sample (127 patients in each group).
Box 6 – Program feedback by participants, by treatment group
|
|
Control |
CDSMS |
P |
||||||||||||
|
|
|||||||||||||||
|
Number of participants |
117 |
114 |
|
||||||||||||
|
Usefulness of the program |
|
|
0.001 |
||||||||||||
|
None at all |
35 (30%) |
12 (11%) |
|
||||||||||||
|
Somewhat useful |
43 (37%) |
43 (38%) |
|
||||||||||||
|
Very useful |
32 (28%) |
54 (47%) |
|
||||||||||||
|
Extremely useful |
6 (5%) |
5 (4%) |
|
||||||||||||
|
Missing data |
1 (1%) |
0 |
|
||||||||||||
|
Changed management of health |
|
|
< 0.001 |
||||||||||||
|
Not at all |
78 (67%) |
45 (39%) |
|
||||||||||||
|
Somewhat |
33 (28%) |
59 (52%) |
|
||||||||||||
|
A great deal |
6 (5%) |
10 (9%) |
|
||||||||||||
|
Improved relationship with general practitioner |
|
|
0.33 |
||||||||||||
|
Not at all |
89 (76%) |
76 (67%) |
|
||||||||||||
|
Somewhat |
23 (20%) |
30 (27%) |
|
||||||||||||
|
A great deal |
5 (4%) |
7 (6%) |
|
||||||||||||
|
Missing data |
0 |
1 (< 1%) |
|
||||||||||||
|
Would recommend program to others |
|
|
0.029 |
||||||||||||
|
Definitely |
29 (25%) |
36 (32%) |
|
||||||||||||
|
Yes |
70 (60%) |
65 (58%) |
|
||||||||||||
|
Maybe |
10 (9%) |
12 (11%) |
|
||||||||||||
|
No |
8 (7%) |
0 |
|
||||||||||||
|
Missing data |
0 |
1 (1%) |
|
||||||||||||
|
|
|||||||||||||||
|
CDSMS = chronic disease self-management support. |
|||||||||||||||
Received 9 February 2017, accepted 15 June 2017
- Richard L Reed1
- Leigh Roeger1
- Sara Howard1
- Jodie M Oliver-Baxter1
- Malcolm W Battersby1,2
- Malcolm Bond1
- Richard H Osborne3
- 1 Flinders University, Adelaide, SA
- 2 Flinders Human Behaviour and Health Services Unit, Flinders University, Adelaide, SA
- 3 Health System Improvement Unit, Centre for Population Health Research, Deakin University, Geelong, VIC
This investigation was supported by a grant to Flinders University from the Australian Department of Health and Ageing (DoHA) under the Sharing Health Care Initiative – Innovations in Chronic Disease Self-Management Research Grants program. The DoHA had no role in the study design, collection, analysis, and interpretation of data, writing of the article, or the decision to submit it for publication. We thank the patients and general practitioners from Chandlers Hill, Flagstaff Hill and Colonel Light Gardens, and Chris Moschou for their support. We also thank members of the research team for their contributions: the Flinders Program adviser (Vee Pols), Flinders Program clinicians (Angela Eastwood, Katrina Reschke, Melissa Day, Pauline Kelly), attention control group health professionals (Lauren Bullivant, Marie Iannos), our research nurse (Bridgit McAteer-Carr), and the qualitative researchers (Chris Barton, Linda Isherwood, Stacey Masters). Richard Osborne was supported in part by a National Health and Medical Research Council Population Health Research Fellowship (Career Development Award).
Malcom Battersby is the developer of the Flinders Program. He has no financial interest in the Flinders Program, but Flinders University has received funding from government, commercial and charitable sponsors for the research, development and dissemination of the Flinders Program.
- 1. Institute of Medicine Committee on Identifying Priority Areas for Quality Improvement; Adams K, Corrigan JM, editors. Priority areas for national action: transforming health care quality. Washington (DC): National Academies Press (US), 2003. https://www.ncbi.nlm.nih.gov/books/NBK221294/ (viewed May 2017).
- 2. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996; 74: 511-544.
- 3. National Health Priority Action Council. National chronic disease strategy. Canberra: Australian Government Department of Health and Ageing, 2006. http://webarchive.nla.gov.au/gov/20141215061219/http://www.health.gov.au/internet/main/publishing.nsf/Content/pq-ncds-strat (viewed May 2017).
- 4. Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; (3): CD002990.
- 5. Jordan RE, Majothi S, Heneghan NR, et al. Supported self-management for patients with moderate to severe chronic obstructive pulmonary disease (COPD): an evidence synthesis and economic analysis. Health Technol Assess 2015; 19: 1-516.
- 6. Kroon FP, van der Burg LR, Buchbinder R, et al. Self-management education programmes for osteoarthritis. Cochrane Database Syst Rev 2014; (1): CD008963.
- 7. Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 2005; 143: 427-438.
- 8. Kenning C, Coventry PA, Bower P. Self-management interventions in patients with long-term conditions: a structured review of approaches to reporting inclusion, assessment, and outcomes in multimorbidity. J Comorb 2014; 4: 37-45.
- 9. Britt HC, Harrison CM, Miller GC, et al. Prevalence and patterns of multimorbidity in Australia. Med J Aust 2008; 189: 72-77. <MJA full text>
- 10. Smith SM, Soubhi H, Fortin M, et al. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012; 345: e5205.
- 11. Reed RL, Battersby M, Osborne RH, et al. Protocol for a randomised controlled trial of chronic disease self-management support for older Australians with multiple chronic diseases. Contemp Clin Trials 2011; 32: 946-952.
- 12. Battersby M, Harvey P, Mills PD, et al. SA HealthPlus: a controlled trial of a statewide application of a generic model of chronic illness care. Milbank Q 2007; 85: 37-67.
- 13. Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. Am J Public Health 1990; 80: 446-452.
- 14. Osborne RH, Elsworth GR, Whitfield K. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns 2007; 66: 192-201.
- 15. Nolte S, Elsworth GR, Sinclair AJ, et al. The extent and breadth of benefits from participating in chronic disease self-management courses: a national patient-reported outcomes survey. Patient Educ Couns 2007; 65: 351-360.
- 16. Bowling A. Just one question: If one question works, why ask several? J Epidemiol Community Health 2005; 59: 342-345.
- 17. Meurer LN, Layde PM, Guse CE. Self-rated health status: a new vital sign for primary care? WMJ 2001; 100: 35-39.
- 18. Fayers PM, Sprangers MA. Understanding self-rated health. Lancet 2002; 359: 187-188.
- 19. Sansoni JE, Grootemaat P, Seraji MH, et al. Targeting integrated care to those most likely to need frequent health care: a review of social and clinical risk factors. Wollongong:: Centre for Health Service Development, Australian Health Services Research Institute, University of Wollongong, 2015. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0008/274742/Evidence_Check_Targeting_integrated_care_Social_and_clinical_risk_factors.pdf (viewed May 2017).
- 20. Primary Health Care Advisory Group. Better outcomes for people with chronic and complex health conditions: final report. Canberra: Australian Government Department of Health, 2016. http://www.health.gov.au/internet/main/publishing.nsf/Content/primary-phcag-report (accessed May 2017).
- 21. Billot L, Corcoran K, McDonald A, et al. Impact evaluation of a system-wide chronic disease management program on health service utilisation: a propensity-matched cohort study. PLoS Med 2016; 13: e1002035.
- 22. RAND Europe, Ernst & Young LLP. National evaluation of the Department of Health’s integrated care pilots: final report. London: Department of Health; 2012. http://www.rand.org/content/dam/rand/pubs/technical_reports/2012/RAND_TR1164.pdf (accessed May 2017).
- 23. Battersby M, Harris M, Smith D, et al. A pragmatic randomized controlled trial of the Flinders Program of chronic condition management in community health care services. Patient Educ Couns 2015; 98: 1367-1375.
- 24. Reed RL, Barton CA, Isherwood LM, et al. Recruitment for a clinical trial of chronic disease self-management for older adults with multimorbidity: a successful approach within general practice. BMC Fam Pract 2013; 14: 125.





Abstract
Objective: To determine whether a clinician-led chronic disease self-management support (CDSMS) program improves the overall self-rated health level of older Australians with multiple chronic health conditions.
Design: Randomised controlled trial: participants were allocated to a clinician-led CDSMS group (including client-centred goal setting and the development of individualised care plans) or to a control group in which they received positive attention only.
Setting and participants: Patients aged 60 years or more with at least two chronic conditions, recruited between September 2009 and June 2010 from five general practices in Adelaide.
Main outcome measures: The primary outcome was self-rated health. Secondary outcome measures related to health status (fatigue, pain, health distress, energy, depression, illness intrusiveness), health behaviour (exercise, medication adherence), and health service utilisation.
Results: 254 participants were randomised to the CDSMS and control groups, of whom 231 (117 control and 114 CDSMS participants) completed the 6-month programs and provided complete outcomes data (91%). An intention-to-treat analysis found that CDSMS participants were more likely than control participants to report improved self-rated health at 6 months (odds ratio, 2.50; 95% confidence interval, 1.13–5.50; P = 0.023). Between-group differences for secondary outcomes were not statistically significant.
Conclusion: CDSMS may benefit some older people with multiple chronic conditions to a greater extent than positive attention and health education.
Trial registration: Australian New Zealand Clinical Trials Registry ACTRN12609000726257.