Transparency is key to achieving affordability of health care
There is increasing concern about the sustainability of health care in Organisation for Economic Co-operation and Development (OECD) countries. Australia currently spends US$6140 per capita — or 9.1% of its gross domestic product — on health care.1 Moreover, there is evidence that health care costs, including out-of-pocket (OOP) expenses, are rising.2 In Australia, 68% of health care costs are funded through the public health system, with 32% from other sources, including private health insurers and OOP expenses.2 To encourage Australians to take out health insurance, the private health system is subsidised by a private health insurance rebate, which costs the public about $5 billion per year.2 Private health insurers derive their income from premiums, which have risen an average of just under 6% per year since 2012, well above the inflation rate or the consumer price index.3 Individual OOP expenses are also rising at an average rate of 6.2%; they have more than doubled in a decade and accounted for 17.8% of Australia’s $140 billion health care spending in 2013–14.2
Value is defined as the health outcomes achieved per dollar spent.4 Moreover, data on performance and outcomes are fundamental to the ability to determine value. Reports on variation across the country,5 including comparison with other OECD countries,6 may prompt a review of activity (the treatments and procedures the health system provides), but cannot determine their value without measurement of costs and outcomes.
To ensure high value, the procedures performed must be appropriately indicated, avoiding overservicing or selecting a particular treatment when its likelihood of success, compared with the alternatives, is limited. Health professionals have an ethical responsibility to avoid waste in health care — not only by better targeting resources, but also because “useless tests and treatments cause harm”.7
The interim report on the Medicare Benefits Schedule (MBS) review8 highlights a recurring theme of how to better inform the system through stakeholder feedback based on contemporaneous data. There is currently limited use of health care data, a lack of meaningful clinical reports and often a failure to engage clinicians in clinical governance. This includes costs and fees charged across the health system and informing consumer choice.
The Royal Australasian College of Surgeons (RACS) and Medibank, Australia’s largest private health insurer, have published reports on surgical variance, which detail the cost and outcomes of care in selected high volume procedures for general surgery, otolaryngology, urology, orthopaedics and vascular surgery.9
Data sources and analysis
The data in the reports were extracted from administrative claims — received by Medibank from private hospitals and specialists — for treatment provided to Medibank policy holders. This initial analysis looked at hospital separations with an admission date in 2014 and any follow-up hospital separation funded by Medibank within 6 months of discharge. The reports were compiled from hospital claims data, hospital casemix protocol data and MBS data relating to diagnoses, interventions and patient demographics. We analysed service use, including transfers to intensive care units (ICUs) and rehabilitation, and plotted outcomes based on length of stay, hospital acquired complications, re-admissions and re-operations. The data on costs included the Medicare item numbers billed, total costs of a hospital admission, cost of prostheses, and OOP expenses.
Procedures were identified by MBS code and selected on the basis of volume to ensure a sufficient spread across surgeons performing them. A principal procedure was identified for each hospital separation, and for most of them, this was the highest value MBS item fee from the medical claim. Where multiple MBS codes described a single procedure, the similar MBS codes were combined. Surgeon level analysis was limited to those with at least five procedures in the dataset. Medibank did not share the identity of the individual surgeon.
Hip replacement as an example
The RACS and Medibank reports on clinical variation focus on specific surgical procedures without risk adjustment.9 For patients who had hip or knee arthroplasty, there was wide variation in the length of stay, use of ICU bed days or rates of transfer to inpatient rehabilitation.
We have used hip replacement as an example in our discussion of costs, fees and value. The rates of hospital acquired complications were reassuringly low.
The cost of a surgical episode of care includes the sum of hospital, surgeon and other providers’ fees, the prosthesis, and pharmaceuticals. The use of ICU after the operation or transfer to rehabilitation following a surgical admission varied considerably. For the 299 surgeons who performed at least five procedures, the average separation cost of a surgeon ranged between $18 309 and $61 699 with a median of $26 661 (the average total cost per hospital separation was $27 310). High volume surgeons showed greater congruity and were closer to the median in terms of the overall cost of a hip replacement. There was little variation in regional (state and territory) total costs.9
Prices for hip prostheses varied from $4908 and $16 178, with a median of $10 727 (Box 1). In Australia, there is considerable disparity in the cost of prostheses when prices are compared between the public and private health systems.10 The amount paid by private health insurers for a prosthesis in the private sector can be twice the amount in public hospitals. Australia also pays a high price for prostheses when compared with other OECD countries.10 The government has recently announced a reduction in the price to be paid for items on the Prostheses List, reducing a hip prosthesis by 7.5%.11
OOP expenses
Medical practitioners in Australia, including surgeons, often augment the fee paid by Medicare and the private health insurer with a copayment paid by the patient. This is known as an OOP charge and is often resented by patients with private health insurance. There is considerable variability in the rebate a health fund will reimburse with regards to a provider’s fee and, therefore, some difference in gap payments is to be expected.
Medibank-insured patients who had a hip replacement incurred an OOP charge by the principal surgeon in 39% of separations, and the average OOP fee was $1778.9
For the 299 surgeons who performed at least five hip replacements, 142 (47%) did not charge any OOP. The average OOP charged ranged from none to $4057.9 The OOP surgical fee is a large but not the only component of gaps paid by patients. OOP charges for other medical services, including charges raised by the anaesthetist, assistant surgeon, and for diagnostics, were charged in 80% of the hospital separations, with an average charge per patient of $342.9
What is a reasonable fee?
The RACS recognises — as does the Australian Medical Association — that gaps are necessary and that, apart from the variability in insurance coverage, the underlying cause of gap fees is the failure of government reimbursement through Medicare to keep pace with inflation and the cost of providing a service.12 The RACS view is that the fees charged should be reasonable and in line with the skill, effort and risks associated with performing a procedure and providing perioperative care.13
Surgeons should not take advantage of the vulnerability of their patients. No one should need to access their superannuation, remortgage their home or resort to crowd funding to have surgery that is clinically indicated. In Australia, the public system is always available for emergency and urgent surgery. RACS has made explicit statements in this regard, published position statements12,13 and provided advice to patients. The RACS code of conduct14 makes clear what is expected of surgeons in setting and informing patients about fees.
There was also no correlation between the size of the fee charged and the quality of the surgery. Indeed, an unpublished analysis by the RACS and Medibank found that surgical fees charged were not correlated with the length of stay for any procedures studied (Box 2). Length of stay is a reasonable surrogate for quality in well defined, largely standardised unicomponent elective operations, such as joint replacement, which have well established post-operative and discharge protocols.
There is an opportunity to further reduce the length of stay after a joint replacement when comparing the Medibank Private results with the public sector in Victoria15 and Scotland.16 This reduction may be achieved without diminishing the quality; a shorter stay may make savings and increase in value.
Conclusion
The discussion around the affordability of health care must continue. As key members of the health care team, surgeons cannot ignore the total costs of surgical services, the components within that service or the fees associated with their individual activity. The Medibank and other administrative datasets inform us on variation in the components of value — clinical activity, outcomes, reimbursements and costs. Making the reports publicly available9 provides assurance of transparency and accountability and may better inform surgeons’ and patients’ choices in the future.
Box 1 – Average prosthetic cost for hip replacements
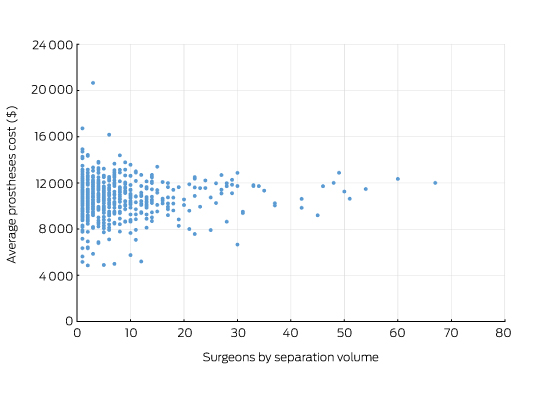
Source: Royal Australasian College of Surgeons and Medibank Surgical Variance Report for Orthopaedic Surgery.9 The data cover the claims paid by Medibank for Medibank policy holders during 2014. Separations that included either Medicare Benefits Schedule items 49318 or 49321 were recorded as the highest value procedural item on the medical claim.
Box 2 – Total knee replacement: plot of the out-of-pocket fee charged by the surgeon and hospital length of stay showing no correlation
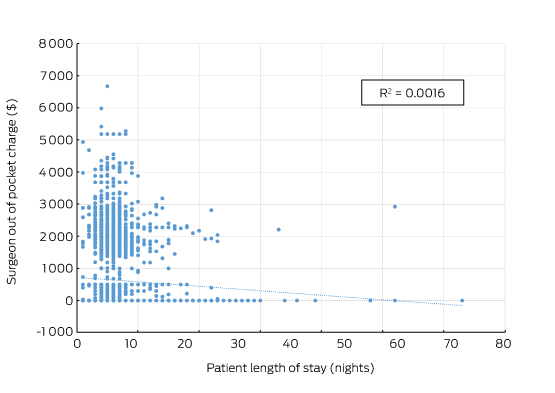
Source: Royal Australasian College of Surgeons and Medibank. The data cover the claims paid by Medibank for Medibank policy holders during 2014. Separations that included either Medicare Benefits Schedule items 49518 or 49521 were recorded as the highest value procedural item on the medical claim.
Provenance: Not commissioned; externally peer reviewed.
- David J Hillis1,2
- David AK Watters3,4
- Lawrie Malisano5
- Nick Bailey6
- David Rankin6
- 1 Chief Executive's Office, Royal Australasian College of Surgeons, Melbourne, VIC
- 2 University of Melbourne, Melbourne, VIC
- 3 Deakin University, Geelong, VIC
- 4 Barwon Health, Geelong, VIC
- 5 Brisbane Orthopaedic and Sports Medicine Centre, Brisbane, QLD
- 6 Provider Networks and Integrated Care Medibank, Melbourne, VIC
We thank the members of the RACS Clinical Variation Working Party for their input towards selecting the data for reporting and their interpretation. We also thank James Aitken, Chair of the Western Australian Audit of Surgical Mortality, for advice on showing the lack of correlation between OOP expenses and length of stay.
No relevant disclosures.
- 1. Hall J. Australian health care — the challenge of reform in a fragmented system. N Engl J Med 2015; 373: 493-497.
- 2. Australian Institute of Health and Welfare. Health expenditure Australia 2013–14 (AIHW Cat. No. HWE 63; Health and Welfare Expenditure Series No. 54). Canberra: AIHW; 2015. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129552833 (accessed Dec 2016).
- 3. Department of Health. 2016 Premium Round Individual private health insurer average premium increases. Canberra: Commonwealth of Australia; 2016. http://www.health.gov.au/internet/main/publishing.nsf/Content/privatehealth-average-premium-round (accessed Nov 2016).
- 4. Porter ME. What is value in health care? N Engl J Med 2010; 363: 2477-2481.
- 5. Australian Commission on Safety and Quality in Health Care. Australian Atlas of Healthcare Variation. Sydney: ACQSHC; 2016. https://www.safetyandquality.gov.au/atlas/ (accessed Nov 2016).
- 6. Australian Commission on Safety and Quality in Health Care. Exploring healthcare variation in Australia: analyses resulting from an OECD study. Sydney: ACQSHC; 2014. https://www.safetyandquality.gov.au/publications/exploring-healthcare-variation-in-australia/ (accessed Nov 2016).
- 7. Brody H. From an ethics of rationing to an ethics of waste avoidance. N Engl J Med 2012; 366: 1949-1951.
- 8. Department of Health. Medicare Benefits Schedule Review Taskforce — interim report to the Minister for Health. Canberra: Commonwealth of Australia; 2016. http://www.health.gov.au/internet/main/publishing.nsf/Content/mbsr-interim-report (accessed Oct 2016).
- 9. Royal Australasian College of Surgeons, Medibank. Surgical variance reports. Melbourne: RACS, Medibank; 2016. http://www.surgeons.org/policies-publications/publications/surgical-variance-reports/ (accessed Oct 2016).
- 10. Private Healthcare Australia. Costing an arm and a leg. Making healthcare more affordable and accessible for Australians. Canberra: PHA; 2015. http://www.privatehealthcareaustralia.org.au/wp-content/uploads/PHA-Report-Costing-an-arm-and-a-leg-Oct-2015.pdf (accessed Oct 2016).
- 11. Ley S. Turnbull government to ease pressure on private health insurance premiums. Canberra: Hon Sussan Ley; 2016. http://sussanley.com/turnbull-government-to-ease-pressure-on-private-health-insurance-premiums/ (accessed Dec 2016).
- 12. Australian Medical Association. Out of pocket costs in Australian health care. Canberra: AMA; 2014. https://ama.com.au/system/tdf/documents/AMA_submission_out_of_pocket_costs_may_2014.pdf?file=1&type=node&id=35220 (accessed Oct 2016).
- 13. Royal Australasian College of Surgeons. Excessive fees. Melbourne: RACS; 2014. http://www.surgeons.org/media/20023066/2014-10-30_pos_fes-pst-036_excessive_fees.pdf (accessed Oct 2016).
- 14. Royal Australasian College of Surgeons. Code of conduct: Melbourne: RACS; 2016. https://www.surgeons.org/media/24335322/2016-04-29_mnl_racs_code_of_conduct.pdf (accessed Dec 2016).
- 15. Christelis N, Wallace S, Sage CE, et al. An enhanced recovery after surgery program for hip and knee arthroplasty. Med J Aust 2015; 202: 363-368. <MJA full text>
- 16. National Health Services Scotland. Optimal patient pathways for hip and knee arthroplasties: use of Enhanced Recovery After Surgery principles — 2013. A report from the Musculoskeletal Audit on behalf of the Scottish Government. Edinburgh: NHS Scotland; 2013. http://www.qihub.scot.nhs.uk/media/576341/orthopaedics%20-%20sosdg%20-%20enhanced%20recovery%20-%20msk%20audit%204%20-%20report%20-%20march%202014.pdf (accessed Nov 2016).





Peter Burke
The article, ‘Variation in the costs of surgery: seeking value’. MJA: 2017: 206(4) 153-154, by Hillis et al., is of perennial interest, both within and without the medical profession.
Browsing through some books left to me by my late medical practitioner father, I came across a small tome entitled, ‘The Doctor Wears Three Faces’.
Written by Mary Bard and published in London by Hammond, Hammond & Co. Ltd in 1949, it appears to have achieved modest success, with a total of three ‘Impressions’ within a year.
The dustjacket remnant provides some ‘Press Opinions’; an example: “This is a delightful book, in which sturdy commonsense and an ether mask are made amusing”.
The frontispiece takes the form of a simple poem with an anonymous author: indeed, it is this poem, which provides the title for the book.
Those sage words are now reproduced for today’s readers, to confirm, as if needed, that some things never change!
Three faces wears the doctor: when first sought
An angel’s; and a god’s the cure half wrought;
But when, the cure complete, he seeks his fee
The devil looks less terrible than he.
Mr. Peter F. Burke.
MBBS FRCS FRACS FACEM DHMSA FAMA
Competing Interests: No relevant disclosures
Mr Peter Burke
Latrobe Regional Hospital
john owen
They say there was no correlation between the fee charged and the quality of surgery which was measured by "Length of stay" (LOS) on basis that LOS is a reasonable surrogate for quality. Where is the proof that the shorter time in hospital, the better the operation?
When the DRGs hit Victorian Hospitals, LOS became an 'obsession'. It is possible to discharge patients the day after a major joint replacement. It generally requires a strict protocols, significant hospital resources , selection and education of patients to manage their expectations but what does that have to do with the quality of the surgeons work and therefore the Value of the fee. Of more importance is the observation I heard the President of the BOA make about early discharge of frail patients after major orthopaedic surgery, "I know it is possible , but is it kind?"
The price gouging by multinational companies manufacturing orthopaedic implants is scandalous but some clawback is occurring . That is the biggest single cost of the episode of care for a joint replacement. Almost half of the Orthopaedic surgeons do not charge an OOP. Quality of joint replacements in this country is measured in our Joint registry. The revision rate is falling. That is a good outcome
Competing Interests: No relevant disclosures
Mr john owen
St Vincents east Melbourne